193
Dysplasia is a disorder in the formation of tissues, organs, or individual parts of the body. Bone dysplasia is a pathological replacement of bone tissue with fibrous tissue with or without elements of dysplastically transformed bones and calcifications.
Most often, the pathology is congenital, but its development in the postnatal period and even in adults is possible.
What is cementoma
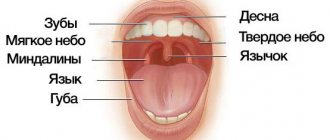
This is a type of benign tumor that forms in the area of the tooth root. It consists of fibrous cement-like tissue and at first does not manifest itself in any way - only a specialist can diagnose the problem. The development of the pathological process is accompanied by the gradual destruction of bone and epithelial tissue in the oral cavity. When the tumor reaches a large size, deformation of the jaw occurs. In some cases, the disease can lead to a fracture of the jaw bone. Women, as well as persons under the age of 20, are more susceptible to pathology.
Only a specialist can diagnose the problem
Most often, cementoma forms in the area of the central teeth of the lower jaw. In other cases, the tumor may be localized in the upper jaw, but this situation is especially dangerous, since here the pathological process can affect the maxillary sinuses. According to ICD-10, cementoma belongs to category D16 - benign neoplasm of bones and articular cartilage, subtype D16.4 - bones of the skull and face.
Congenital malformations of the skeleton. Dysplasia
Due to the fact that the main molecular-biochemical defect for most OCD has not been established, etiopathogenetic treatment for these diseases does not yet exist. Therefore, the only possible option is symptomatic treatment. Since OCD are systemic diseases of connective tissue, they often also involve extraskeletal changes, which should be promptly addressed. Therefore, most patients with OCD require observation and treatment by many specialists (cardiologists, neurologists, pediatricians, ophthalmologists, etc.). An important role belongs to orthopedic treatment - both conservative and surgical.
Conservative treatment for OCD should be applied from the moment of diagnosis.
Conservative treatment can go in three directions:
- preventive treatment;
- correction of deformities;
- treatment of associated complications.
Preventative treatment
Preventive measures are effective only with early detection of OCD and consist in creating conditions for the child during growth that make it possible to slow down the pathological process.
In the first year of life, treatment should be aimed at preventing the development of deformities or their progression. In the first months of a child’s life with OCD, general muscle hypotonia, incorrect position of the head and/or torso, slight deformity of the spine and contractures of the joints of the extremities may be observed. If muscles are weak, from the first days of life it is necessary to create conditions under which the child can make more active movements. To do this, you need to put a romper on the baby and not swaddle him. Swimming strengthens muscles well. Starting from 2 months of age, the child should undergo repeated courses of general massage and constant therapeutic exercises. These procedures have a beneficial effect on muscle trophism and help increase their strength. Therapeutic gymnastics consists of passive and active movements. Passive movements maintain joint mobility. To obtain active movements in the first days of a child’s life, it is necessary to use reflex movements. So, to force the child to straighten his legs with force, you can use the crawling reflex. To do this, the child is placed on his stomach, his legs are bent at the hip and knee joints (frog pose), and his palm is placed on his feet. In this case, the child rests his feet on the hand, straightens his legs and crawls forward. All these exercises are included in the complex for practicing with a healthy child.
Subsequently, you can use gaming techniques: give the toy so that the child reaches for it with either his right or left hand; make him turn over first one way or the other; lying on your stomach, bend your torso first to the right, then to the left, etc.
In AH, in addition to general hypotension, there is looseness of the knee joints due to shortening of the femur and the convergence of the attachment points of the thigh muscles. Therefore, special attention is paid to strengthening these muscles.
A child should not be placed in pillows or taught to walk while holding hands. Such haste leads to deformation of the skeleton. After 6-7 months of life, it is better to put children on the floor and give them the opportunity to do everything they can. The child sits down and stands up only if he has sufficiently strong muscles.
For existing deformities, all therapeutic measures should be aimed at preventing their progression. If the body position is incorrect or there is a visible deformation of the spine, children should be kept in beds with a flat mattress that does not sag under the weight of the child.
With kyphosis in the thoracolumbar spine, children in the first months of life should be placed on their stomach more often and taught to sleep in this position. Lying on his stomach, the child tries to raise his head. These movements strengthen the back muscles. At an older age, the child begins to pull his legs under his body and tries to kneel, while the spine bends forward, which to some extent evens out the kyphosis. If the head position is incorrect (tilting to one side), it is recommended to place the child in a symmetrical position, placing heavy bolsters on the sides of the head (from the shoulder girdle upwards). When a child has a tilt of the head and a bend of the body that cannot be corrected by laying it with bolsters, it is necessary to make a plaster crib with the head held in a position that can be corrected. In addition, these children are recommended to undergo repeated courses of asymmetrical massage, therapeutic exercises, and swimming. During active gymnastics, it is necessary to force the child to turn in the opposite direction from his usual position. To do this, you can call him or place a toy on the side of the convexity of the curvature. After the child begins to sit down on his own, it is necessary to limit sitting as much as possible, and when this is not possible, he must be seated on a chair with a straight, high, firm back and tied to the chair so that the child does not lean forward or sideways. To do this, you need to sew a bra that secures the entire chest; Straps are sewn to the sides of the bra, which tie the child’s torso to the back of the chair.
In patients with a progressive course of the disease, preventive measures include a gentle regimen, prohibition of long walking, physical education and sports. Swimming, skiing and cycling on flat terrain are permitted.
Sanatorium treatment relieves pain, if any; the general condition improves, the child becomes more mobile. With repeated courses of sanatorium treatment, children retain mobility in the joints for a long time, contractures in the joints do not form or progress, and the progression of limb deformities in the area of the epiphyses slows down. In between courses of sanatorium treatment, exercise therapy, repeated courses of massage, and swimming are indicated.
Correction of skeletal deformities. With OCD, a large number of different deformations are observed. However, you should not try to correct every deformity.
Contractures in the elbow joints in OCD due to subluxation of the radial head usually do not respond to conservative treatment, but in the vast majority of cases they do not affect the function of the limb.
Club hand is quite easily corrected with the help of exercise therapy and the application of removable splints, which give the hand a middle position. Splints can be made from gypsum or polymer materials.
Spinal deformities, as a rule, cannot be corrected.
The greatest difficulties are presented by pathological changes in the hip joints. It must be taken into account that dislocation and subluxation of the hip in DD cannot be treated. It is usually not possible to correct a dislocation in this disease, and persistent and long-term treatment can lead to severe contractures and even greater deformation of the femoral head.
In VSED, high-standing proximal ends of the femurs are mistaken for hip dislocation due to sharp coxa vara, despite the fact that the acetabulum is well developed on the pelvic radiograph. They try to straighten the “dislocated” hip - first with splints, and sometimes simultaneously under anesthesia. This treatment results in a sharp progression of coxa vara, and the appearance of the ossification nuclei of the femoral head is further delayed. In order to avoid mistakes, you must be very careful when examining the child, and if a disproportion of the physique is detected, very carefully study the x-ray of the hip joints. If it is impossible to exclude a dislocation, then before starting treatment, contrast arthrography should be performed, which will help establish the correct diagnosis and not cause harm to the child.
Foot deformities due to OCD are treated with staged plaster casts. An exception is clubfoot in DD, as it is difficult to correct. In this case, it is necessary to start treatment from the first days of the child’s life. The treatment method is somewhat different from that for ordinary congenital clubfoot. A plaster cast is applied to the lower limb from the middle third of the thigh to the end of the fingers, but since patients have flexion contractures in the knee joints, when applying the plaster they try to straighten the limb as much as possible. When moving the foot out of a vicious position, the varus position is mainly corrected. At the same time, they try to align the equinus position, but one should not try to completely remove the foot from this position, since it is difficult to correct, and if the foot is forced out of the equinus position, a recurrence of varus deformity may occur. After the foot is moved out of the varus position and the flexion contracture in the knee joint is somewhat corrected, children are given polyvik splints up to the upper third of the thigh, with a heel. In splints, the child begins to learn to walk. Only with this disease do we recommend teaching children to walk, since they may not begin to walk at all, and our task is to give them the opportunity to move on their feet.
In some diseases (TC, Ollier's disease, etc.), asymmetric shortening of the lower extremities is observed. In these cases, it is necessary to equalize the length of the limbs. To do this, shoes on a shortened leg are “knocked”, while the front part and the heel are knocked separately in order to maintain the roll of the foot when walking. The shortening is not fully compensated, since otherwise the valgus curvature may progress. Usually, the difference in limb length is left at 0.5 cm. These children require constant monitoring, since in the first years of life the child grows quickly and the difference in limb length can change quickly.
Treatment of associated complications. Such complications include early arthrosis, acute arthritis and aseptic necrosis of the femoral head.
Early arthrosis is observed in children with severe joint deformation or when a gentle regimen is not observed. At the very beginning of the disease, rest and thermal procedures temporarily relieve pain, but due to the heavy load on the joint, they can recur. These patients are recommended for sanatorium-resort treatment, therapeutic exercises (can be done in water), and massage. Repeated courses of sanatorium-resort treatment (mud therapy, brine baths, massage, swimming, restorative treatment, etc.) delay the development of arthrosis. If left untreated, in most cases, arthrosis deformans progresses rapidly, causing an increase in contractures. The pain symptom becomes more intense and constant.
Treatment of arthritis in EDS and DD is very difficult. For ordinary arthritis, the joint is immobilized to relieve pain. Taking into account the peculiarities of the course of these arthritis, in the acute period, bed rest, slight movements in the joint (preferably in water at a temperature of 36-37°C), and painkillers are recommended. When the pain is relieved, physiotherapeutic treatment is carried out. The most effective are paraffin-ozokerite applications followed by electrophoresis of humisol.
Paraffin-ozokerite applications are applied to the affected joint (sometimes to both) at a temperature of 40-42°C. The procedures are performed daily or every other day (depending on the age and individual tolerance of the procedure to the patient). In total, up to 20 procedures are recommended for a course of treatment. Immediately after the procedure, the patient receives electrophoresis of humisol on the same joint, which is performed every other day (on the day of paraffin-ozokerite applications), also up to 20 procedures per course of treatment. Humisol can be administered from both poles. The complex of treatment measures includes injections of vitamin B12.
Aseptic necrosis of the femoral head in NSHS can be observed in MED, MPS and other diseases. Treatment is the same as for Perthes disease, but without immobilizing the joint. Unloading of the joint must be carried out until the femoral head can be restored.
Surgical treatment of diastrophic dysplasia. Surgical treatment of DD is extremely difficult, which is explained by the prevalence and severity of deformities and their steady progression.
The primary task of the surgeon is to draw up a program of multi-stage conservative and surgical treatment, the ultimate goal of which is to enable the child to move without outside support, at least with the help of crutches.
At the first stage, tissues are prepared for the intervention. The feet are corrected using staged plaster casts, eliminating varus and equinus deformities. At the same time, massage the muscles of the thighs and gluteal muscles.
The second stage is the actual surgical treatment according to the scheme developed at the CITO. It is based on intensive surgical treatment in a short time followed by long-term rehabilitation treatment.
The first operation is performed on the femoral segment. Subspinal myotomy is performed. The bone is crossed at the level of the lesser trochanter, and a wedge is selected from the proximal fragment with its base posterior and outward. The fragments are compared, eliminating flexion and adduction of the hip. If the muscle tension is strong, the femur is shortened or its proximal metaphysis is inserted like a spyglass. Osteosynthesis is performed with an extraosseous plate or an intraosseous Bogdanov nail, which is preferable, since the next osteotomy is performed in the supracondylar region of the femur to eliminate severe flexion contracture. For mild contracture, osteotomy is performed according to Repka; for severe contracture, metaplasia is performed according to Wreden. The operation is completed with plastic surgery of soft tissues according to Roux-Friedland-Volkov with the aim of open reduction of the dislocated patella or its fragmented rudiments. Thus, in one stage the vicious position in the hip and knee joints is corrected.
Correction of equinovarus foot deformity is carried out 3-4 weeks after hip surgery. The Zatsepin operation is performed, supplemented, if necessary, with an economical crescent resection of the foot. Immobilization with a plaster cast for 2 months. Then restorative treatment is carried out.
Surgical treatment of deformities on the other leg is planned similarly. The full cycle of intensive treatment lasts 5-6 months. In case of hip dislocation, only extra-articular operations are permissible.
Rehabilitation of the patient is complemented by the production of splints or lightweight orthopedic devices, orthopedic shoes. The patient is subject to long-term observation by an orthopedist.
The prognosis for the life of patients with DD is favorable.
Surgical treatment of spondyloepimetaphyseal dysplasia. For congenital spondyloepimetaphyseal dysplasia, the indications for surgery are adductor flexion contractures of the hip joints, high hip dislocations in combination with varus deformity of the neck and deformity of the hip joint.
Attempts at closed and open reduction of dislocations end in failure. Extra-articular operations are indicated: intertrochanteric osteotomies. The proximal end of the distal fragment of the femur is shifted 1-1.5 cm inward and the femur is retracted, forming an angle open outward and posteriorly at the level of the osteotomy. In the corrected position, metal osteosynthesis is performed using a bone plate. In adolescents, after osteosynthesis with the Nuzhdin-Trotsenko plate, plaster immobilization is not performed. In young children, a plaster cast is applied until fusion in the osteotomy area.
The load on the operated joint is allowed after movements have been developed. Due to the progression of arthrosis in people after 20-30 years of age, the need for endoprosthetics arises.
In patients with late spondylometaphyseal dysplasia (Kozlovsky type), indications for surgical treatment arise only when valgus deformities of the knee joint progress. Corrective osteotomies are performed according to Repka with fixation of fragments with knitting needles and plaster bandages.
For Kniest dysplasia, operations on the hip joints are performed only in adolescence, as a rule, with severe coxarthrosis with pain. More often, indications for surgery arise for clubfoot. A Zatsepin operation is performed followed by the prescription of orthopedic shoes.
Patients with metatropic dysplasia and Dyggwe-Melchior-Clausen disease are generally not operated on, the former due to respiratory failure, the latter due to mental retardation.
Surgical treatment of spondyloepiphyseal dysplasia. Surgical treatment of children with EDS, carried out in high school and adolescence, makes it possible to radically help the patient. The purpose of surgical interventions is to relieve children from pain, increase range of motion and improve the supporting function of the limbs.
Indications for surgery: flexion contractures of the hip and knee joints, dislocations of the patellas, coxarthrosis and gonarthrosis.
Flexion contractures of the hip joints are the first sign of coxarthrosis. When contracture increases, if it is not yet accompanied by a distinct pain syndrome, i.e., before the age of 10-12 years, decompression of the joint is performed by myotomy of the adductor muscles of the thigh, subspinal myotomy, and also cutting off the attachment site on the lesser trochanter of the iliopsoas muscle. In cases where the contracture is not completely eliminated, an intertrochanteric osteotomy is performed with fixation of the fragments with knitting needles, straight plates, or biopolymer clamps. The operation is performed in stages or in one stage on both sides. A plaster cast with a pelvic girdle is applied to both legs. After the cast is removed (3 weeks after soft tissue operations and 6 weeks after osteotomy), the position of the legs apart is maintained with a Vilensky splint. They prescribe classes in the pool, walking only on crutches, and exercise therapy. 4-6 months after surgery, the load on the joints is increased, but overload should be avoided.
As the child grows, contractures recur and progress, and pain in the joints appears and increases. During this period of disease development, reconstructive surgery on the proximal femur is indicated due to the progression of coxarthrosis.
The operation technique is as follows. With the patient in the lateral position, the outer surface of the femur is exposed from the top of the greater trochanter downwards using an external Langenbeck approach 12-15 cm long. Marks are made on the outer surface of the bone. At the base of the lesser trochanter, the bone is transversely osteotomized. A wedge is selected from the proximal fragment with the base outward, 2 cm high and 1-1.5 cm posterior, depending on the severity of the flexion contracture. Then osteosynthesis is performed using the Trotsenko-Nuzhdin fixator. The operation, if indicated, is complemented by myotomy of the adductor muscles and hip flexors. The leg is placed on a splint. Movements in the joint begin on the 6th-7th day. Walking on crutches is allowed after 2-3 weeks; dosed load - after 2 months and full load - 5-6 months after osteotomy. After the patient has been rehabilitated, a similar operation is performed on the other side.
Changes in the shape of the epiphyses and defective articular cartilage inevitably lead to progression of the process, and in adolescence or young age, movements in the hip joint stop. Coxarthrosis of III-IV degree develops. In these cases, total hip replacement becomes the operation of choice.
The knee joint ranks second in the frequency of clinical manifestations of EDS. These are flexion contractures that form either independently or in combination with contractures of the hip joints. In a significant percentage of cases they are caused by dislocation of the patella. In this case, the operation of choice is open reduction of the dislocation according to Roux-Friedland-Volkov.
The operation technique is as follows. A skin incision is made along the outer surface of the thigh from its upper third downwards along the outer surface of the knee joint, rounding to the tibial tuberosity. After dissecting the fascia, the rectus femoris muscle is isolated from its upper third to its attachment to the patella. The vastus lateralis muscle is cut off at the point where it transitions into a tendon sprain. The knee joint is bent and the cut portion of the quadriceps muscle is sutured to the outer surface of the rectus muscle. On the inside, the rectus muscle is sutured to the vastus medialis muscle. The attachment point of the patellar ligament is cut off together with a bone fragment and fixed with Mylar threads 1-2 cm downwards and inwards. Make sure that the patella does not dislocate when bending the tibia.
Immobilization of the limb with a plaster cast is carried out for 3 weeks. At this time, isometric tension of the thigh muscles is prescribed, and electrical stimulation of the rectus and vastus medialis muscles is performed. After removing the plaster cast, functional treatment is carried out. Physiotherapeutic procedures (paraffin applications on the knee joint), massage of the inner thigh are prescribed. Weight-bearing on the operated leg is possible after 6 weeks, and full movement is restored 6 weeks after surgery.
Congenital dislocation of the patella can be combined with valgus deviation of the tibia due to hypoplasia of the lateral femoral condyle. Under these conditions, the Roux-Friedland-Volkov operation may be ineffective and must be combined with simultaneous correction of bone deformity. From an external approach made for soft tissue surgery, the bone is freed from the periosteum in a limited area and transversely transected at the base of the condyles. By rotating the distal fragment inwards by 8-10°, a position is achieved such that the medial and lateral condyles of the femur with their anterior surface are located in. one plane. The achieved position is fixed with knitting needles, and in adolescents - with a bone plate. Movements in the joint are prescribed if there are signs of fusion.
The prognosis for EDS is favorable for life, but the patient must be under the supervision of an orthopedist all his life. Rational employment of the patient and the fight against excess body weight are especially important.
Surgical treatment of multiple epiphyseal dysplasia. Surgical interventions for MED are indicated for the development of deformity in the knee joint area, dislocation of the patellas, coxarthrosis and gonarthrosis.
In case of curvature, an osteotomy is performed in the supracondylar region of the femur or in the subcondylar region of the tibia. Osteotomy according to Repka is more often practiced. Considering the tendency to ankylosis when fixed with a plaster cast, osteosynthesis with external fixation devices is advisable. For the same reason, during surgery on the proximal end of the femur, it is necessary to use the Nuzhdin-Trotsenko plate for osteosynthesis.
Patellar dislocation in patients with MED may be accompanied by its fragmentation, which causes patellofemoral arthrosis. Therefore, it is advisable to combine the Roux-Friedland-Volkov operation with resection of the patella in the frontal plane with covering of the sawdust with local tissues.
The steady progression of arthrosis leads to the need for hip and knee replacement at a young age.
Surgical treatment of pseudoachondroplasia. Orthopedic surgeries for groin disorders are aimed at correcting deformities of the lower extremities, combating arthrosis of the hip and knee joints, and correcting short stature.
Deformity of the legs is corrected by subcondylar or supramalleolar osteotomy. Fixation of bone fragments is carried out using devices for transosseous osteosynthesis. Intervention on both legs in one stage significantly speeds up the rehabilitation process for patients.
Flexion contractures in the hip joint are eliminated by intertrochanteric osteotomy with external metal osteosynthesis; contractures of the knee joint are eliminated by supracondylar osteotomy.
Interventions aimed at correcting short stature require special care. Indications for lengthening leg segments are limited by the presence of severe deformation of the epiphyses of the bones, especially in the hip joint. Only minor extensions are permissible in case of asymmetry in leg length.
Surgical treatment of Volkoff's disease . At the initial stages, treatment is conservative: orthopedic shoes are prescribed on the healthy leg in order to compensate for the patient’s excess growth. As a preventive measure, preventive epiphysiodesis of the fingers and toes is possible. If the leg is significantly lengthened, the joint is sanitized by removing cartilaginous growths along with the patella, followed by restorative treatment. In case of cartilaginous ankylosis of the joint in combination with sharp lengthening, resection of the knee joint followed by compression arthrodesis is indicated. In the case when movements in the joint are preserved, segmental resection of the bones of the leg or femur is performed, followed by osteosynthesis with one of the external fixation devices. In case of severe damage to the knee, ankle joints, foot with severe trophic disorders, leg amputation followed by prosthetics is indicated. Growths on the bones of the skull, if they have a cosmetic defect, are removed. If cerebral symptoms increase, the patient should be treated by neurosurgeons.
The prognosis for life with damage to the skull bones is unfavorable or questionable. The disease ultimately leads to ankylosis of the affected joints.
Surgical treatment of hemimelic epiphyseal dysplasia. Surgeries should be performed in the early stages, before secondary deformities and arthrosis develop. An arthrotomy is performed, osteochondral growths are removed, and the epiphysis is carefully modeled.
Rehabilitation treatment begins 1-2 days after surgery. Physical therapy is carried out, and orthopedic shoes are prescribed if indicated.
As a rule, GED recurs. In case of relapse, a similar operation is performed in the early stages. It is preferable to carry out 4-5 economical resections without massive damage to the articular cartilage than radical operations with resection of the epiphysis bone, which always leads to severe arthrosis. With the development of segment deformity, a corrective osteotomy is performed; with severe arthrosis in adolescents, arthrodesis is performed.
Surgical treatment of dyschondroplasia. The range of surgical orthopedic treatments for dyschondroplasia is extremely wide and depends on the location and extent of bone lesions, the age of the patient, the severity of deformity and shortening of limb segments, etc.
Indications for surgery are the growth of cartilage tissue, deforming the bone and adjacent joint; deformation and shortening of a limb segment or several segments; threat of malignancy or malignancy of cartilaginous nodes.
Orthopedists are more likely to encounter dyschondroplasia in the case of damage to the metacarpal bones and phalanges of the fingers and toes. Surgical treatment for this localization is indicated for thickening of the phalanges and metacarpal bones before the development of secondary curvatures and tumor-like growths that disfigure the hand and reduce its functionality.
A staged marginal resection of the metacarpal bones and phalanges of the fingers is performed with the removal of foci of cartilaginous tissue. The resulting defects are filled with allografts. In case of relapses, the operations are repeated. This approach provides a good cosmetic result and full preservation of the function of the fingers. A similar principle is used when localizing cartilaginous nodes in the scapula and ilium, where bone resection within healthy tissue is combined with bone grafting.
Multiple deformities of the limbs with their shortening are caused by damage to the proximal and distal metaphyses, as well as the diaphysis. It is clear that it is impossible to remove all foci of embryonic cartilage due to their large number. Therefore, most orthopedic operations for dyschondroplasia are palliative in nature.
If the humerus is damaged, accompanied by its shortening and deformation, a closed correction is performed at the age of 8-10 years by applying an Ilizarov apparatus, taking into account the curvature. Closed correction is also combined with compactotomy or osteotomy through the pathological focus at the apex of the curvature. Distraction corrects deformity and compensates for shortening.
If there is a curvature in children over 10 years of age, as well as in patients with recurrent deformities, marginal bone resection is performed. The pathological tissue is then removed, the humeral axis is corrected, and the defect is filled with long cortical grafts. The Ilizarov apparatus is applied so that the proximal wires pass through the grafts, and the distal wires pass outside them. During the process of distraction in the apparatus, the distal fragment shifts along, and the formation of the regenerate sharply accelerates.
When cartilage lesions are localized in the bones of the forearm, the treatment principle is the same as when localized on the shoulder. An Ilizarov apparatus is used, in which the affected radius or ulna is lengthened by traction of the distal fragment of the bone after its osteotomy. Shortening can also be corrected using a rod apparatus.
Correction of curvatures and deformations of the femurs is carried out in the same way as for curvatures of other etiologies. Ilizarov and rod apparatuses are used.
Correction of deformities and shortening of the legs is carried out using the Volkov-Oganesyan and Ilizarov apparatuses. A combination of compression-distraction osteosynthesis with bone grafting is possible.
The peculiarity of dyschondroplasia is that relapses of shortening and deformation always develop and staged surgical treatment should be completed by the time the patient’s natural growth stops.
Dyschondroplasia is a disease in which individual nodes or several foci can become malignant at once or sequentially. Malignancy is manifested by pain and rapid growth of one of the lesions. If there is a threat of malignancy, segmental bone resection is performed within healthy tissues, followed by bone grafting. This requires close monitoring of the patient throughout his life.
Surgical treatment of metaphyseal chondrodysplasia . Surgical treatment of MCD (Schmidt, Jansen, McCuisick type, Pyle's disease, cranio- and frontometaphyseal dysplasia) is symptomatic. More often, corrective supracondylar and subcondylar osteotomies of the femur and tibia are performed. It should be taken into account that with metaphyseal dysplasias of the Schmidt, Jansen and McKusick type, deformities are prone to recurrence and require repeated corrections. The most optimal period for performing corrective operations for metaphyseal dysplasia coincides with the time of onset of ossification of the metaphyses.
Surgical treatment of mesomelic dysplasia . Indications for surgical correction of deformities are often given for dyschondrosteosis. Corrections are required for curvatures of the forearms, reminiscent of those in Madelung's deformity, as well as for varus curvatures with shortening of the legs.
Correction of deformity of the forearm and wrist joint is carried out by osteotomy of the distal metaphysis of the radius with its lengthening in the Ilizarov apparatus. The treatment technique is the same as for Madelung's deformity. Correction of deformities and shortening of the tibia is carried out by osteotomy, followed by lengthening of the segment and correction of the axis of the tibia in an external fixation device.
Correction of the shins with Nievergelt's dysplasia is more difficult, because it is combined with deformation of the epiphyses of the tibia, disruption of the shape and function of the ankle joint, and flat-valgus deformation of the feet. Such children undergo gentle osteotomies followed by transosseous osteosynthesis. Lengthening of the legs is not advisable in them, as well as in children with Robbinov's dysplasia.
Surgical treatment of mucopolysaccharidosis . Surgical treatment of lower extremity deformities is advisable only in children with preserved intelligence, i.e., with mucopolysaccharidosis type IV (Morquio syndrome).
Curvatures are corrected with subcondylar osteotomies. Operations are performed under exsanguination of the operated limb, as quickly as possible, without blood transfusions. Due to the tendency of deformities to recur in the postoperative period, a splint with a hinge is prescribed for the knee joint.
Surgical treatment of achondroplasia and hypochondroplasia . Surgical interventions for AC are aimed at correcting varus deformities of the legs and short stature.
Varus curvatures of the legs are corrected by subcondylar and supramalleolar osteotomies, using external fixation devices for osteosynthesis.
Leg lengthening with achondroplasia poses a number of problems for the orthopedist. When drawing up a long-term treatment program, it is necessary to clearly understand at what age of the child it is more rational to carry out intervention, from which segments to start lengthening, what technique to use, to know the advantages and disadvantages of all external fixation devices, to clearly know about possible local and general complications, to be able to predict the result and possible negative consequences in the long term after the end of treatment.
Lengthening the legs for a child represents a complex set of negative emotions caused by almost constant, although not intense, pain at the site of osteotomy and the insertion of wires, inconvenience in walking, self-care, and the development of a symptom complex of hospitalism. Only rare children under 10 years of age realize the need for lengthening; the majority of patients suffer from treatment. Therefore, 12 years seems to be the optimal period when leg lengthening should begin.
There are various schemes for lengthening leg segments: simultaneous symmetrical lengthening of segments, lengthening of two adjacent segments at the same time, etc. Experience dictates a differentiated approach to this problem.
In patients with a height of 135-138 cm completed at the age of 14-15 years, simultaneous lengthening of the hips is rational. In patients who are planning long-term multi-stage treatment, it is more rational to cross-lengthen according to the scheme: right thigh - left shin, then left thigh - right shin. In the interval between stages, the disproportion in the length of the segments with this scheme is little noticeable, and in the process of lengthening the patient better tolerates the presence of external fixation devices. Using this scheme, it is possible to increase height by 40-45 cm in 4-5 years, starting from the age of 10.
When lengthening the legs, it is more advisable to use the Volkov-Oganesyan, Ilizarov apparatus. Cross lengthening, especially in patients with hypertrophied muscle and fat layers, is easier to tolerate with a combination: lengthening of the tibia with the Volkov-Oganesyan or Ilizarov apparatus and lengthening of the thigh with a rod apparatus. With such a combination
Reasons for the development of pathology
Experts in the field of dentistry still cannot identify specific reasons that are guaranteed to lead to the formation of a benign tumor on the jaw bone. Today, experts identify several factors that can provoke the development of pathology:
- chronic course of inflammatory processes in the oral cavity - osteomyelitis, actinomycosis, fibrous periodontitis and others,
- severe injury to the jaw bone due to a blow, bruise,
- systematic mechanical damage to hard or soft tissues of the oral cavity - incorrectly installed fillings, dentures, orthodontic apparatus (brackets).
The photo shows osteomyelitis.
Genetic predisposition can also be added to possible predispositions. Negative external influences, such as smoking or radiation therapy, can also contribute to the development of pathology.
Development of the disease in the sacrum and lower back
Lumbar disease manifests itself in various forms.
| Form | Description |
| Lumbalization | Formation of one or more extra vertebrae in the lumbar region. At the same time, the number of vertebrae in the sacral region is reduced. |
| Spondylolysis | As a result of the development of the disease, the vertebral arches become disconnected. |
| Spina bifida in the lumbar region | There are open and closed types. The disease is manifested by protrusion of the spinal cord through the spinal canal. |
| Sacralization | Fusion of vertebrae (S1 and L5). |
Important! Lumbar dysplasia can be detected using a tomograph and x-ray. An orthopedist can identify the problem during the first examination.
This pathology provokes serious changes in the spinal column - most often a change in gait is observed. In more advanced cases, the child loses the ability to walk independently. In addition, the disease causes the development of problems with the kidneys and urinary organs.
This pathology provokes the development of other abnormalities associated with the locomotor system and internal organs
All this applies to congenital pathology. However, in addition to it, there is also acquired dysplasia. Most often it develops as a result of birth or postpartum trauma.
Lumbar myelodysplasia is often diagnosed in childhood. The disease provokes:
- back pain;
- dysfunction of the hip organs;
- flat feet;
- trophic disorders.
With myelodysplasia in a newborn, the risk of death increases sharply.
Characteristic symptoms
One of the most dangerous characteristics of cementoma is its asymptomatic course. In the first stages of development of the pathology, the patient does not experience any discomfort or pain. Therefore, most often the tumor can only be detected at a dentist’s appointment.
“Dangerous disease! I noticed it already at the last stage, when I went to the dentist to treat a tooth, I just wanted to put a filling and remove one. As a result, they discovered cementoma... And indeed, there was no pain at all, I didn’t feel anything. I’m sure that I’m still very lucky that everything coincided like that...”
Nataly, from correspondence on the forum www.32top.ru
The tumor can be identified by x-ray.
As the size of the tumor increases, the thickness of the cortical plate decreases, which creates unnecessary pressure on the periosteum. At this stage of pathology development, the patient may experience the following symptoms:
- discomfort and moderate pain when eating or talking,
- unpleasant sensations at the moment of mechanical impact on the causative area,
- slight deformation of the enamel structure, change in its color.
When the tumor reaches a large size, it can lead to rupture of the mucous membrane and soft tissues in the oral cavity. In the most advanced cases, there is a risk of deformation of facial features and even fracture of the jaw bone.
Types of dental cementoma - classification
Experts identify several forms of cementoma. Each variety is characterized by its own characteristics and symptoms. Let's look at each type in a little more detail.
Benign cementoblastoma
We are talking about a true cementoma, which is understood as a neoplasm of coarse fibrous tissue with varying degrees of mineralization. The tumor is covered with a kind of film - this capsule separates it from healthy cells. This form is characterized by a rather slow course, but the tumor itself can grow to unlimited sizes. The initial stages of this process are not accompanied by any symptoms, but over time there is pronounced resorption of the cortical plate. As a result, the patient experiences discomfort and unpleasant sensations during mechanical action on the causative area, for example, when brushing teeth or eating.
The tumor is covered by a peculiar capsule
An advanced stage can lead to deformation of the jaw bone and the eruption of a tumor, which is fraught with infection and the development of inflammatory processes. Typically, the tumor occurs on the lower jaw in the premolar area.
Cement-forming fibroma
The tumor grows slowly, and the process of its development is usually accompanied by mild symptoms. A lesion with weak mineralization of the neoplasm is formed in the bone tissue, which is due to its fibroblastic structure. In this case, cement-like tissue is formed already at an advanced stage of the pathology, when tumor growth stops. This form of cementoma is especially dangerous when localized in the upper jaw, where its spread is fraught with damage to the maxillary sinus1.
Periapical cement dysplasia
The pathological process occurs in dental cement and bone tissue, which leads to thinning of the walls of the root system of molars. This situation is dangerous due to root fracture. Cement dysplasia usually has many pathological foci, but all of them, as a rule, do not exceed 1 cm in diameter. Tumor formation is also asymptomatic. In this case, there is no deformation of the jaw. Most often, the neoplasm is localized in the anterior parts of the lower dentition.
Periapical cemental dysplasia is often localized in the mandible
Gigantoform cementoma
This form of cementoma is characterized by intensive development, namely the rapid transformation of connective tissue into cementum. The x-ray image clearly shows oval-shaped pathological foci located in close proximity to the root system of the tooth. In this case, the localization can be very different, but usually tumors arise in places that are symmetrical relative to each other. Many experts agree that giganoform cementoma has genetic background, so often a similar diagnosis is given to several members of the same family.
This variety has oval-shaped lesions
general characteristics
Jaw dysplasia is the replacement of the jaw bone with connective tissue containing elements of cement-like calcifications. The fibrous mass consists of cells responsible for the synthesis of collagen, elastin and other components.
The affected jaw bones lose their normal structure, strength, and their composition and morphology change. The pathological process leads to the emergence of factors:
- Changes in bone shape.
- Facial asymmetry.
- Fractures.
- Destruction of surrounding areas.
- The appearance of inflammation, pain and other clinical signs.
In most cases, the disease is asymptomatic.
The first case of pathology was described by Recklinghausen, a pathologist from Germany in 1891.
There is no consensus among doctors regarding the classification, stages and types of this anomaly. The article describes generally accepted formulations and characteristics.
The localization of foci and the prevalence of the disease are determined by its type. Women are more susceptible to this anomaly compared to men. The average incidence rate is 1-6%.
The key cause is non-hereditary gene mutations that disrupt the normal process of bone formation.
How is diagnostics carried out?
Diagnosis of cementoma is possible only in a dental clinic. It is often possible to identify it after the patient contacts him, but for a different purpose, for example, for the treatment of caries or standard prevention. If, during a visual examination, a specialist develops appropriate suspicions or characteristic symptoms occur, the patient will be sent for an x-ray.
Histology helps to conduct a thorough study of the structure and structure of deformed tissues. The sample is placed on a microslide (slide for the object being studied), after which it is carefully examined in a multiply enlarged format, that is, under a microscope. This allows you to accurately determine the specific form of the tumor and make a final diagnosis. Histological examination also makes it possible to differentiate cementoma from other types of tumors, including malignant ones.
Histological examination is also performed for diagnosis
What treatment is required
The choice of direction of therapy directly depends on the form of the pathology. Thus, benign cementoblastoma and cementing fibroma are treated by surgical removal, including partial excision of the affected area of bone tissue. In this case, the causative tooth has to be removed.
In the case of periapical cement dysplasia, the growth of the tumor does not occur as intensively. The surgical method is practically not used, since such an intervention can create a threat of tissue necrosis. If there are no symptoms, therapy is based on regular observation by a specialist, enhanced oral hygiene, and careful monitoring of the periapical lesion area.
In the presence of pronounced symptoms and the development of the inflammatory process, rejection of the sclerotic masses occurs. This process may take an impressive period of time, but upon completion, complete recovery will be achieved. To speed it up, a specialist can create a small depression in the area of the affected bone.
Conservative methods of therapy are also used to treat gigantoform cementoma. The doctor will definitely prescribe anti-inflammatory drugs and put the patient on regular monitoring.
Treatment process
Jaw dysplasia requires a careful approach. Surgical intervention unless absolutely necessary is considered undesirable.
If the pathology is asymptomatic, an observation tactic is chosen with the patient’s scheduled visits to the doctor. This requires high-quality oral hygiene, control of periapical dental diseases, and taking measures to prevent tooth loss.
Watchful waiting is most appropriate for CDD. In case of sclerosis caused by hypovascularization, biopsy or tooth extraction under conditions of CDD provokes necrosis. These provocations should be avoided.
If the disease occurs with clinical manifestations and pain, with the danger of degeneration of benign formations into malignant tumors, surgical intervention is used with excision of newly formed and affected tissues. Most often, the need for this arises in the fibrotic form.
The main method of surgical intervention is curettage of a fibrous or fibro-osseous formation from a healthy bone. It is not difficult to distinguish pathological from healthy tissues.
The modified bone is like sugar soaked in syrup. The bone cavity is filled with soft, slippery gray tissue. All pathological tissues are removed. According to indications, bone replacement materials can be used.
If an inflammatory process occurs in pathologically altered tissues, conservative treatment in the form of antibiotics can be prescribed. However, this is not always effective.
Possible complications
Complications most often arise when cementoma is localized in the anterior part of the upper jaw. As the tumor grows, there is a serious risk of its spreading to the nasal sinuses, which can subsequently lead to the development of nasopharyngeal pathologies.
Another possible complication of cementoma may be a breakthrough of the oral mucosa with the tumor coming to the surface. Perforation leads to the appearance of a hole in the bone tissue and mucous membrane. As a result, the risk of infection of the affected tissues, the development of inflammation and the spread of pathological processes to adjacent areas of the jaw increases.
Preventive measures
To minimize the risk of developing cementoma, it is important to ensure proper and complete oral hygiene, and also, if possible, eliminate the risks of accidental injury to the teeth and jawbone. Experts provide a number of specific recommendations in this regard:
- brush your teeth twice a day, rinse your mouth after every meal, use floss and preventative rinses, visit a dental hygienist twice a year to remove plaque and dental deposits,
- promptly seek dental care for injuries to the teeth and mucous membranes,
- do not postpone a visit to the doctor if there is a traumatic factor in the oral cavity, for example, an incorrectly installed filling, crown or prosthesis.
It is worth having professional teeth cleaning twice a year.
Late detection of cementoma can lead to disruption of the integrity of bone tissue, spread of the tumor to healthy parts of the jaw, and the appearance of perforation in the jaw bone and mucous membrane. To avoid all these complications, it is necessary to carefully monitor the condition of your teeth and oral cavity, as well as regularly visit the dentist’s office for preventive maintenance - at least twice a year.
- Trigolos N.N., Makedonova Yu.A., Firsova I.V., Starikova I.V., Piterskaya N.V., Marymova E.B., Poroyskaya A.V. Cement-bone dysplasia of the jaws, 2015.
How to stop abnormalities in the fetus?
To prevent the formation of dysplasia in a newborn child, his parents must follow the right lifestyle. At the time of bearing a child, it is worth preventing possible cases of injury. Do not forget about the prevention of viral diseases.
A woman who is about to give birth should see her doctor promptly if:
- her age is over 35 years;
- she is married to a close relative;
- There have been cases of carrying a child with disabilities.
Despite the fact that dysplasia is a very serious disease, often resulting in death, it certainly can and should be combated if the problem is identified in a timely manner.
During pregnancy, a woman should carefully monitor her health and undergo regular examinations.
Young people who want to have children in the future must carefully and seriously approach the issue of health. Do not neglect medical instructions.