09.11.2020 8396
If you look closely at the structure of the jaw, you will notice a groove separating the tooth and gum. Depending on the characteristics of the patient, it has a different structure and depth.
It is this groove that is called the periodontal pocket. The depth in a healthy person usually does not exceed 2 mm.
However, bacteria accumulate inside and severe inflammation gradually develops. Deepening begins, periodontitis or gingivitis develops.
The problem is that the dentist needs to remove the affected tissue to treat the patient. If this is not done, the process will only progress and the inflammation will affect larger and larger areas and begin to threaten the tooth.
The stripping process is called curettage.
About periodontal pockets and causes of inflammation
The problem does not appear by itself; there must be serious prerequisites for it.
The need for curettage is provoked by five potentially dangerous factors:
- Inflammation of the gums or periodontal tissues . Formed where soft tissue touches the tooth.
- Insufficient oral hygiene . If you brush your teeth incorrectly, food debris gets inside the groove. As they decompose, bacteria multiply.
- Serious dental plaque . Formed due to significant fossilization. Problems also begin for people who ignore the formation of tartar.
- Congenital anomalies . This leads to the pocket being deeper or having a non-standard structure. Bacteria will accumulate in it much more intensely.
- Diseases of the body . Patients with hormonal imbalances and digestive disorders are at risk. Their saliva composition changes, which can have a serious negative effect on the oral mucosa.
Curettage will be required if you have orthopedic structures installed and your metabolism is impaired.
Smokers and people who drink a lot of alcohol suffer from such problems - inflammatory processes are very common in them.
There are two types of periodontal pockets - false and true.
In the first case, the gum moves away greatly from the anatomical cell, and no damage to the deep tissues is observed.
In the second case, everything is more complicated, because periodontal tissue begins to collapse. This type of pocket can be either horizontal or vertical.
When to do gum curettage?
Indications for curettage of periodontal pockets are: 1) the presence of chronic generalized periodontitis, 2) local form of periodontitis. In both cases, periodontal pockets will appear along the surface of the tooth roots, the formation of which is associated with the resulting destruction of the dentogingival attachment (i.e., the attachment of the marginal gum to the neck of the tooth).
Destruction of the periodontal attachment in chronic generalized periodontitis occurs against the background of irregular oral hygiene, which contributes to the deposition around the necks of teeth - soft microbial plaque and hard tartar. Microorganisms in the composition of dental plaque trigger an inflammation process in the gums, which at the first stage is manifested by swelling and redness of the gums, bleeding when brushing teeth. Already during this period, gradual destruction of the periodontal attachment begins (with the formation of periodontal pockets).
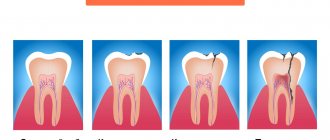
Chronic generalized periodontitis –
1) Formation of periodontal pockets –
As soon as the periodontal attachment is destroyed, so-called “periodontal pockets” are formed between the gum and tooth. At first they are relatively small. Shallow periodontal pockets up to 4.0 mm deep correspond to mild periodontitis, and closed curettage may be indicated for precisely such patients (to prevent the progression of periodontitis).
Periodontal pockets are localized between the gum and the root of the tooth (Fig. 2). One wall of the pocket is the surface of the tooth root, on the surface of which microbial plaque and subgingival tartar are attached. The other wall is the inner surface of the unattached gum, which is covered with pathological epipelium and granulations. Thus, the typical contents of a periodontal pocket are dental deposits, granulations, and pathological epithelium.
Scheme of the structure of the periodontal pocket -
As we said above, in the absence of treatment, the depth of the pockets gradually increases. This occurs due to the destruction of the bone plate around the tooth, as well as periodontal fibers, due to which the tooth root is firmly attached to the bone. This gradual process inevitably leads to the appearance of tooth mobility, the increase in the degree of which in the future will be directly related, among other things, to the continuing increase in the depth of periodontal pockets.
2) Destruction of bone tissue around the tooth –
As was seen above in Fig. 2, the periodontal pocket “grows” deeper due to the destruction of periodontal fibers between the root surface and the bone plate, which also leads to the destruction of the bone graft itself (alveoli). Moreover, it should be noted that bone tissue does not simply disappear without a trace, but is replaced by the so-called inflammatory granulation tissue, which contains a large number of microbial cells, osteoclasts, etc. On an x-ray, the absence of bone around the teeth looks like this (Fig. 3b).
Clinical situation No. 1 –
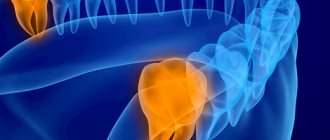
Next, in Figures 4-6, you can see exactly what a deep periodontal pocket looks like under the gum in the interdental space between the canine and premolar in the lower jaw. As we can see from the outside, the gums look quite healthy, and only on an x-ray (Fig. 5) can we see a slight darkening between the roots of the teeth, indicating the presence of destruction of bone tissue. But we have a completely different look after the gums are detached and granulations are cleaned out of the pocket between the teeth (Fig. 6).
In Fig. 6 we see a deep bone defect of a large volume, as well as subgingival calculus on the surface of the tooth root (indicated by an arrow). Such deep periodontal pockets can no longer be sanitized using the closed curettage technique, which is carried out without gum detachment and therefore does not imply visual inspection of bone defects in the depths of the periodontal pocket (i.e., the doctor will simply blindly try to clean out what to clean out from under the gums).
Therefore, for pockets larger than 4.0 mm, only open curettage or flap surgery should be used. For medium and deep periodontal pockets, only these methods allow you to remove all granulations and dental deposits from under the gums, carefully scrape out the pathological epithelium from the inner surface of the gums, and also replant synthetic bone tissue in the area of deep bone defects (with the hope of partially restoring bone levels ).
Why is it impossible to do without curettage when treating periodontitis (in principle) -
With shallow periodontal pockets up to 4.0 mm, provided that you have good equipment (a good scaler, a Vector device) and the painstaking work of a periodontist, it is still possible to stop the progression of chronic periodontitis. The biggest challenge will be removing subgingival deposits from periodontal pockets, which is difficult to do even in shallow pockets, given that the work is carried out almost blindly.
When deep periodontal pockets have formed (more than 4 mm deep) and granulation tissue has formed at their depth, the process essentially becomes irreversible, despite any conservative local and general anti-inflammatory therapy. You can drink antibiotics, rinse your mouth with antiseptics, smear your gums with anti-inflammatory gels, irradiate your gums with a laser, but all this will be ineffective. Why?
- Firstly , it is impossible in principle to completely remove dental plaque from deep periodontal pockets. The fact is that the doctor inserts the ultrasonic attachment under the gum “blindly”, i.e. he makes movements without seeing what exactly is happening in the periodontal pockets. Therefore, some dental plaque necessarily remains in the pockets.
- Secondly , if deep periodontal pockets have formed, then in them, even after removal of dental plaque and anti-inflammatory therapy, conditions are created for the development of infection and further progression of periodontitis. The fact is that the pockets are filled with granulations, without surgical removal of which it is impossible to stop further destruction of the bone tissue around the tooth.
It turns out that you can still try to remove subgingival dental deposits and granulations in shallow pockets using ultrasonic cleaning and closed curettage techniques. It will be possible to do the same thing efficiently in deep pockets only by performing open curettage or patch surgery.
Signs of inflammation
As with many other diseases, the insidiousness of the situation is that the patient may not notice the problem for a long time. At the same time, it will constantly progress and get worse.
The disease can be noticed at an early stage if you regularly visit the dentist. The development of inflammation is indicated by 6 parameters:
- The gums change color - they turn red or darken.
- An unpleasant metallic taste appears in the mouth.
- A noticeable swelling begins to develop near the affected area.
- Severe bad breath.
- Loose teeth.
- Pain when pressing or eating food that requires chewing.
- Bleeding, which occurs, including during brushing your teeth.
Although it is not so easy to understand that there really is a problem at an early stage, it is possible.
And the sooner you can notice this, the sooner treatment can begin. This greatly affects the success of the final result.
Flap surgery on the gums for periodontitis –
Flap surgery on the gums allows not only to remove all subgingival dental plaque, but also to remove inflammatory granulation tissue from under the gums. It allows, in principle, to eliminate periodontal pockets, and also, in some cases, to stimulate partial restoration of bone volume (in vertical bone defects). The difference between flap surgery and open curettage is that the incision during flap surgery is made 1-1.5 mm from the edge of the gum (24stoma.ru).
Then this 1.5 mm strip of gum, which wraps around the necks of the teeth, is simply removed. Firstly, this allows us to reduce the size of the flaps (gum size), because with severe bone resorption and after removing a large number of granulations, excess gum will be observed. We will not have enough underlying tissue volume to stretch the gum back to the necks of the teeth. That is, as a result, we will receive partial exposure of the roots of the teeth, but at the same time, periodontal pockets between the gums and the roots of the teeth will be completely absent. And this is the most important thing if we want to stop the progression of periodontitis.
The decrease in gum level after surgery can be somewhat reduced if synthetic bone tissue preparations are used for grafting into bone defects. The effect will be even better if special bioresorbable membranes are also used. At one time, the operation is performed on a segment of no more than 6-8 teeth, and takes at least 2.5 hours. This is a complex procedure that requires good surgical skills.
Carrying out flap surgery (animation and video) –
Features of curettage
Curettage becomes the last solution resorted to if alternative methods of correcting the situation fail.
This situation occurs when the pocket deepens to 4 mm.
At this stage, attempts to solve the problem with the use of drug treatment become futile.
When performing curettage, tissue is scraped out or deposits and affected areas are removed by other means.
If the procedure is performed by a dentist with extensive experience and a good level of training, no problems will arise. Moreover, the efficiency in this case will also be very high.
Deep curettage
Severe periodontitis is a serious pathology, accompanied by the presence of periodontal pockets deeper than 5 mm, in which bone pockets often appear. With such signs, more extensive interventions are indicated to cleanse subgingival deposits, especially if the lesion has spread to a large number of teeth. The large depth of the gaps between the gums and the tooth root requires visual control to completely remove the pathological contents, so a radical operation is performed with peeling off a flap of tissue in the area of half or the entire jaw to the depth of the lesion.
After exposing the roots, they undergo deep treatment: removal of epithelial growths, any deposits, affected cement, as well as altered bone tissue. The treated area is washed with antiseptics and stitches are applied. In the presence of severe bone loss, osteoplastic materials are used to promote regeneration. Healing of oral tissue continues for a month.
Indications and contraindications
When a patient comes to the clinic with such a problem, they always take an x-ray.
It will show how severely the periodontal tissue is affected, what means are best to use for complex treatment, and whether surgical intervention is necessary.
There are 5 common indications:
- The appearance of severe loosening of teeth.
- Inflammation, accompanied by an increase in tissue temperature, redness, swelling, and pain.
- Large dental stones.
- Developing a deep true pocket.
- Exhaustion of conservative treatment options with antibiotics and other means.
The decision that curettage can be performed is made only after a comprehensive assessment of the situation and weighing of the data obtained. The list of contraindications includes the following:
- Pronounced fibrous changes developing inside the pocket.
- Severe thinning of gum tissue.
- The pocket depth is more than 6 mm.
- Tooth mobility of the third degree.
Most contraindications are temporary. It is not recommended to carry out the procedure if, for some reason, bacteria are actively multiplying in the mouth.
In such a situation, dental intervention simply will not have an effect and you will have to find the cause of the problem and eliminate it.
Vacuum curettage
Vacuum curettage is a combined method; its technique is similar to the closed method of curettage of periodontal pockets, but together with standard curettes, hollow nozzles connected to a vacuum apparatus are used. Using a compressor, a vacuum is created in the device’s container, capable of sucking out mucus, deposits, and granulations from the space between the root and the gum. To improve visual control, the vacuum method can be performed in conjunction with gingivotomy (dissection of the gums).
Stages of the vacuum method:
- injection pain relief;
- scraping out accessible deposits from the tooth root with curettes;
- scraping granulations from the gums;
- bottom treatment with a vacuum nozzle;
- washing the cleaned area with antiseptics;
- applying a protective bandage for two days.
The vacuum method can be used in the area of 2-4 teeth in one session. As a result of the procedure, congestion is reduced, lymph and blood circulation is normalized. During the action of vacuum, microhematomas are formed, which help accelerate regeneration processes and, as a result, more rapid restoration of the periodontal junction.
Is it possible to perform curettage at the site of an extracted tooth?
Curettage of the socket of an extracted tooth - what is it? This process is similar to what is done when the tooth is still intact. After the tooth is removed, the dentist removes the affected tissue.
This process is carried out if suppuration begins at the site of the tooth, crumbs from hard tissue remain, alveolitis begins to form, or there are signs of necrosis of the walls.
The dentist performs a curettage, after which the wound is closed with a tampon. The process may often be required if, after tooth extraction, the patient behaved incorrectly and the wound did not heal as required.
Another common indication is the appearance of dry socket syndrome. It can lead to alveolitis and the fact that the area will not heal for a long time with all the ensuing dangerous consequences.
Typically, patients themselves are rarely able to determine that they have a problem. Therefore, it is important to be sure to come to the doctor on schedule in order to monitor how tissue restoration is progressing after surgery.
The process itself consists of 5 stages:
- The treatment site is anesthetized so that the patient does not feel anything. Both infiltration and conduction anesthesia are used.
- Washing the hole. All foreign matter is removed, including blood, food debris, and pus.
- Cleaning the tissue walls and the hole itself. This is a direct curettage that requires close attention from the dentist.
- Antiseptic treatment. This is necessary to prevent the spread of bacteria.
- Closing the wound. The doctor applies a bandage. This allows you to stimulate wound healing and reduce the likelihood of resumption of the inflammatory process.
Since the area is treated from all potential threats, the tissue begins to heal quite quickly, and the risk of alveolitis recedes.
Symptoms of pathology
Patients do not immediately notice problems with their gums and turn to the dentist in advanced cases of pathology. Periodontitis and other gum diseases are more common in men, as they smoke a lot. In adolescence, as a rule, false pockets form due to hormonal changes in the body.
Note! Periodontal disease can appear at any age with insufficient oral hygiene.
How to determine the initial form of periodontitis, by what signs?
Signs of pathology:
- unpleasant taste in the mouth;
- change in the shape and color of the gums;
- bleeding and sensitivity of the gums;
- discomfort when eating;
- loose teeth;
- exposure of the neck of the teeth.
If you have at least one of these signs, it's time to visit the dentist.
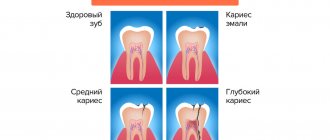
The degree of development of the disease is characterized by the following signs of changes in pocket depth:
- 1st degree - from 3 mm to 3.6 mm;
- 2nd degree - from 3.6 mm to 5.1 mm;
- 3 degree - from 5.1 mm to 7 mm;
- Grade 4 - more than 7.1 mm.
At the very beginning of the development of the disease, patients do not feel any discomfort, so they do not rush to see a doctor. The alarm begins to sound when teeth become loose, when the pathology has gone too far in its development. Pathological forms of periodontitis have the characteristic of rapid development: the patient risks losing completely healthy teeth.
Open curettage technique
Treatment can be performed using various methods. And one of them is open curettage of periodontal pockets.
Dentists perform it to remove all deposits accumulated under the gums. This allows you to prevent the appearance of foci of inflammation, the development of much more serious problems, tooth loss or the need for tooth extraction.
For the procedure to be successful, it is usually accompanied by special restorative therapy.
The doctor prescribes the patient to take medications that reduce inflammatory activity in the body. In parallel, antibacterial treatment is performed.
The technique has proven itself well and allows for quick treatment of even a large number of teeth in one visit – up to seven in a row. At the same time, the use of local anesthesia makes the process much less traumatic for the patient.
It is carried out in several stages:
- Separation of the mucous membrane of the gums . It is important that it does not touch not only the bone, but also the alveolar process. This usually requires making a small, precise incision in the anatomical neck.
- Gum separation . This helps to access the bone pocket directly. The dentist will have a clear view of the affected area and will understand what is being dealt with.
- Curettage . The process uses a scaler. All solid deposits are removed. The tissue is scraped out using a curette – hence the name of the procedure.
- Antiseptic treatment . It is recommended to use special agents with a pronounced hemostatic effect - they prevent the accumulation of blood, the formation of clots and an environment for the proliferation of bacteria.
- Installation of synthetic bone . It is important that the treated fabrics are filled with something. The synthetic product helps reduce the periodontal pocket and prevents the previously eliminated problem from re-developing.
- Stitching . A suture is placed and a gum bandage is installed.
All requirements for the use of special means and antiseptic protection are observed very strictly, so regeneration takes place very quickly.
The standard period for suture removal is ten days. No further intervention will be required.
Despite the fact that the technology is well developed and shows excellent results in dental practice, doctors try to avoid its use.
This is a local surgical intervention that requires a recovery period and strict medical supervision.
Therapy
The basis of periodontitis treatment is to eliminate the infection from the gum tissue. In each case, the dentist selects an individual course of treatment, depending on the severity of the pathology. The patient must carefully follow all the dentist’s recommendations at home in order to help get rid of the pathology as quickly as possible.
Note! Bad habits (smoking) contribute to the exacerbation of pathology and delay the healing process.
How periodontal pockets are treated in the clinic:
- cleansing enamel from soft/hard formation;
- curettage (closed/flap/open);
- vestibuloplasty;
- splinting;
- prosthetics.
The dentist carries out a thorough professional cleaning of the enamel from plaque. It is impossible to do such cleaning at home. The doctor uses curettes and ultrasonic or manual scalers. Cleaning is quite aggressive, however, it does not damage the root part of the tooth.
Important! If there is an increased accumulation of plaque on the teeth, professional teeth cleaning is recommended twice a year.
Next, the dentist polishes the surface of the crown to prevent plaque from accumulating on the tooth. Polishing is carried out using laser equipment or manually. This depends on the equipment available.
After cleaning the teeth from hard deposits, periodontal pockets are cleaned - curettage. The procedure is indicated for second-degree pathology, when the size of the pocket is more than 3.6 mm.
Curettage
Let us consider the procedure for socket curettage in detail. Curettage is a surgical procedure to clean body cavities using a medical instrument - a curette. The dentist removes pathological tissue and cleanses the cavity from waste products of pathogenic microorganisms. Sometimes a curette is used to remove pathological microflora for laboratory analysis.
For example, curettage is performed after removing an affected tooth due to periodontitis. The dentist removes purulent exudate, hardened deposits and fragments of a destroyed molar.
Curettage of a periodontal pocket is prescribed in the following cases:
- inflammatory foci of gingival tissue;
- hard dental deposits;
- formation of a deep pocket.
Closed curettage is carried out when the gum tissue decreases by no more than 4.1 mm; tissue dissection is not performed. Unfortunately, it is impossible to rid teeth of microbial deposits using medicinal methods, so curettage is the only available way to clean periodontal pockets.
Open curettage of periodontal pockets is carried out when the gum tissue decreases by more than 5-6 mm. Pocket cleaning is carried out to prevent the breakdown of jaw tissue. The operation is performed under local anesthesia through an incision in the gum area. After cleaning the tissues from microbial deposits, the gums are sutured and sanitized with antiseptic solutions.
If there is a significant loss of bone (exposure of the root), a flap operation is performed, which differs from open curettage and is performed by detaching the gum tissue along its entire length. In this micro-surgery, bone deficiency is restored using a graft. To restore gum tissue, tissue transplantation is done from the palate. This secures the tooth in the socket and prevents it from falling out.
The use of laser equipment greatly increases the effectiveness of microsurgery on the gums. Firstly, there is no risk of blood loss. Secondly, a high degree of sterility is ensured. Thirdly, the surgeon can adjust and control the tissue processing process.
Pros and cons of curettage
This procedure has its positive and negative sides that you should be aware of. The advantages include the ability to restore the missing part of the bone, get rid of periodontal pockets and strengthen the teeth in the socket. In addition, closed curettage of periodontal pockets is inexpensive.
Minuses:
- relapses are possible after closed curettage;
- open surgery lasts quite a long time - two hours;
- open surgery can damage the teeth and oral mucosa.
Contraindications
The operation is contraindicated in the presence of foci of purulent inflammation: an abscess may appear. Also, curettage is not performed if the pocket has reached the jaw bone. The operation is not prescribed in the following cases:
- severe loss of gum tissue;
- great looseness of teeth;
- pocket size is more than 5.1 mm;
- with fibrous formations.
The operation is not prescribed for existing acute infectious diseases, as well as for pathological disorders of physiological functions.
Vestibuloplasty
This micro operation is performed on the lower jaw to expand/deepen the vestibule of the mouth in case of chronic periodontitis and other pathologies. The operation is indicated for stages 2, 3 and 4 of the disease to stabilize loose teeth in the socket. Vestibuloplasty is also indicated when there is a significant decrease in bone mass: in this case, a biomaterial is transplanted that activates bone growth.
Splinting
This operation is performed to stabilize the teeth in the sockets. Previously, splinting was carried out by installing metal prostheses; modern dentistry has unique methods of combining teeth into a single system using orthodontic equipment. Tire material may vary:
- silk;
- polyethylene;
- fiberglass;
- aramid thread.
Splinting can be either permanent or temporary. Temporary is used for slight tooth mobility at the initial stage of the disease. Permanent splinting is indicated if there is a risk of tooth loss.
Fiberglass holds together the entire dentition - both mobile and stable teeth. First, the orthodontist cuts out a strip on the teeth, then fiberglass tape is placed in it and filled with a bonding solution. The lower teeth are splinted from the back, the upper teeth from the front.
Fiberglass tape looks quite aesthetically pleasing, so it does not cause discomfort during communication. Fiberglass tape also solves the problem of large distances between teeth. If teeth are very unstable, aramid thread, which is highly durable, is used instead of tape.
Closed operation
In addition to open surgery, closed curettage of periodontal pockets can also be used.
Typically, dentists recommend performing it if the pocket itself is shallow and only up to 3 mm .
One of the features of this technique is that the doctor practically does not see the condition of the tissue at the time of the intervention, and against the background of this, some part of the affected tissue remains inside.
When carrying out closed-type exposure, tissues are less injured, and by reducing the affected areas, it is possible to more effectively carry out conservative treatment using a special group of medications.
Most often, this method uses ultrasound. It perfectly removes deposits and is suitable for granulation. The impact itself does not require gum detachment.
By polishing and treating the cleaned areas, plaque no longer accumulates on them, and there is no risk that the problem will manifest itself again.
Bottom line
The formation of gum pockets leads to unsteadiness of molars and a decrease in their ability to grind food efficiently. Periodontitis is a dangerous disease that can lead to the loss of healthy teeth due to pathological destruction of the periodontium. The loss of several molars leads to atrophy (decrease) of the jaw bone mass, which is an obstacle to prosthetics.
Curettage in modern dentistry is done using the latest equipment, so pain and discomfort are reduced to a minimum. You should not be afraid of visiting a doctor and letting your gums become irreversible. For example, laser and ultrasound equipment provides not only painless surgery, but also high quality curettage. Polishing the root zone and treating periodontal pockets prevents the re-formation of tartar in the root zone.
Periodontitis leads to irreversible changes in the jawbone tissue, the treatment of which is expensive. Therefore, a timely visit to the dentist will help to get rid of not only the beginning of the disease, but also save money on expensive operations and implants when teeth are lost. As a preventive measure, you can undergo a course of treatment with antiseptic drugs prescribed by your doctor.
Sources used:
- American Academy of Periodontology (USA)
- "Therapeutic dentistry. Textbook" (Borovsky E. V.)
- Lemetskaya T.I., Periodontal diseases (periodontopathies), M., 1972
Alternative Methods
In addition to closed and open exposure, other types of operations can be used to clean out pockets. These include:
Laser curettage of periodontal pockets
This is one of the main techniques used in advanced dentistry today.
The advantage of the laser beam is that it heats up to high temperatures. In this case, the deposits are simply burned out and the vessels are sealed. This reduces the recovery period and eliminates the risk of re-deposition.
Another advantage is the complete elimination of the need for sutures. During the recovery period, the patient will not experience increased sensitivity due to food intake, and there will be significantly fewer restrictions.
The main thing is not to overheat or lift heavy objects on the first day after surgery. It is best to maintain a rest regime or go to bed so that the body can devote all its strength to regeneration.
Vacuum curettage
Belongs to the closed subtype. The process also uses special curettes, but they are connected to a device that can apply very low pressure.
The tissue is scraped out and immediately sucked out of the hole. The duration of the rehabilitation process is greatly reduced, and the likelihood of complications becomes significantly lower.
Chemical curettage
In this case, citric acid is actively used. It is created on the basis of various types of solutions and allows you to make deposits soft.
A balanced mixture of active substances is pumped into the pocket and actively cleanses it, gives a pronounced antiseptic effect and destroys most potentially dangerous bacteria.
Cryo method
The method is based on freezing tissue using special nitrogen-based compounds. This effectively removes deposits, kills bacteria, and significantly reduces the risk of complications.
This is one of the cowless ways to clean out a pocket.
Which method should I choose from those described?
Despite the fact that some seem to be much preferable to others, in practice everything is not so simple. The fact is that there are individual contraindications that do not allow some patients to use the most bloodless intervention options.
Only after a careful analysis of the patient’s current condition and an assessment of potential risks can one understand which method is best to use. The extensive experience of our doctors allows us to do this without errors.
What to do after the procedure
In most cases, in the first days after surgery, patients develop an inflammatory reaction and swelling. For rehabilitation to be successful, you must strictly follow the doctor’s recommendations. These include:
- Starting from the second day, you need to rinse your mouth with a solution of chlorhexidine, hydrogen peroxide or another antiseptic. Saline solutions can also be used. The frequency of rinsing depends on the chosen antiseptic; in most cases, 2-3 per day is enough.
- It is necessary to follow a special diet until complete healing. It is necessary to exclude solid foods, hot dishes, and avoid excess spices, especially hot ones. It is not recommended to eat sour and salty foods.
- In the first 2-3 days you need to take painkillers and antibiotics prescribed by your doctor.
It is also recommended to replace the toothbrush with a new one, this will serve as additional protection against infection of the postoperative suture.
It is important to consider the type of technique that was used for treatment. After closed curettage, recovery does not take much time, it takes several days. After open cleaning or patchwork, complete normalization of the gum condition can take quite a long time - up to 2-3 months.
If during this period there is a sharp increase in temperature, the general condition worsens, or purulent discharge appears, you must urgently seek medical help. These symptoms may indicate the development of postoperative complications that require specialist intervention.
About the duration of the rehabilitation period
As with any surgical intervention, after curettage there is a recovery phase.
It is important to understand that the procedures themselves are safe and have already been well established in practice. But the patient will be required to follow a number of recommendations in order not to provoke the development of complications.
Among the important requirements at the rehabilitation stage are the following:
- Careful oral hygiene. During the first eight hours, it is better not to brush your teeth at all and not to disturb the operated area; it is not recommended to eat food, mouthwashes - anything that can cause irritation. After this period, you also need to be more careful with cleaning until the stitches are removed.
- If there is severe pain, you can only use medications recommended by your doctor. In most cases, simply applying something cold to the sore area helps.
- The diet is worth reconsidering. In particular, until the tooth heals and stops becoming loose, you should not chew on anything too hard.
- Avoid temperature changes. You should not go into the cold without protecting your cheeks or visit the sauna.
You will also need to comply with other doctor's requirements - use special rinses, change your standard toothbrush to a soft one.
Forecast and preventive measures
The formation of true periodontal pockets indicates the onset of structural deformations in the periodontium. In an advanced stage, the pathological process leads to irreversible consequences. To minimize the risk of encountering such problems, it is important to pay increased attention to oral hygiene and promptly respond to the appearance of any suspicious symptoms.
At the first suspicious symptoms, you should consult a specialist
Remember to brush your teeth twice a day, rinse your mouth, and floss after every meal. It would be a good idea to get an irrigator for better cleaning of hard-to-reach places. Remember that the diet should contain enough fresh fruits and vegetables, when biting on them, a natural mechanical cleansing of plaque from the enamel occurs. Add more healthy foods to your food, rich in vitamins and important microelements. Try to limit your consumption of sweets, flour and carbonated drinks. And it is better, of course, to completely give up smoking and alcohol.
An important condition for proper prevention is systematic visits to the dentist for prevention. You need to visit a specialist for this purpose at least once every six months. And with the same frequency you need to undergo the procedure of the prof. hygiene – cleaning teeth from plaque and hardened deposits.
1According to WHO.
Are there complications?
The procedure is safe and is carried out in strict compliance with all technology requirements.
But there are several potential problems that may arise as a result of personal characteristics of the body or non-compliance with requirements during the rehabilitation period.
These include the following:
- Sensitivity to food temperature . It occurs in almost everyone, but goes away over time. The maximum duration of hyperesthesia is up to two months. To cope with the problem, you can use special gels, ointments, toothpastes and rinses - the dentist will advise which ones.
- Swelling and hematoma . They may not go away for up to two weeks, but do not pose a serious danger.
- Problems in the functioning of the facial muscles . You should not be afraid of such a manifestation, because it will pass in about 10 days. Some patients complain of difficulty opening the mouth, but this also resolves in no more than 12 days, more often earlier.
- Increased tooth mobility . Observed for up to three weeks. For this reason, you need to pay attention again to your diet and remove foods that are too hard.
The patient's condition is constantly monitored by an experienced dentist, so that any serious complications can be avoided.
Adviсe
To avoid pathological formation of tartar, you must adhere to the following recommendations:
do not get carried away with carbohydrate consumption;
- Use a moderately hard toothbrush morning and evening;
- use specialized toothpastes during an exacerbation of the disease;
- clean your teeth using irrigators - they efficiently remove plaque from hard-to-reach places.
For additional sanitation of the oral cavity, use decoctions of medicinal herbs and rinses with antiseptic solutions. If inflammation worsens, rinse your mouth after every snack and meal.
To generally strengthen the immune status, it is necessary to take microelements and vitamins. This will help eliminate the infection from the entire body.
Measuring the depth of periodontal pockets
Normally, the space between the neck of the tooth and the gingival margin should not exceed 1-2 mm. With mild periodontitis, a gum pocket with a depth of 3.5 mm is formed.
The average severity of the inflammatory process is characterized by pockets 4 mm deep. In this case, the x-ray image already shows a bone defect and destruction of the interdental septa. At a late stage, the depth of the fossa exceeds 5 mm.
Measuring the depth of periodontal pockets