The health of our teeth affects our ability to enjoy food and a beautiful smile. One of the important functions is assigned to the periodontium - the tissue that connects the tooth root to the jaw. Actually, thanks to these tissues, reliable fixation and protection of teeth occurs. Carious processes, injuries and errors in previous treatment can lead to such dangerous inflammation as periodontitis.
Dental treatment in the South-Eastern Administrative District at the Neomed clinic eliminates even the most complex inflammatory processes.
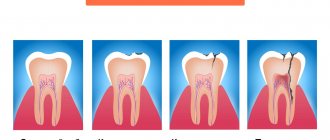
There are acute, chronic and acute periodontitis.
Treatment depends on the clinical nature of the disease.
Thus, acute periodontitis takes the forms:
- serous;
- purulent.
The chronic type includes the following subtypes:
- fibrous;
- granulating;
- granulomatous.
Acute periodontitis is an exacerbation of the chronic form, which forms in the absence of treatment for acute inflammation.
Types of chronic periodontitis
Studies of the clinical picture of the possible course of chronic periodontitis and morphological signs made it possible to identify the following types:
- Granulating
With this form of the disease, under a microscope, a noticeable thickening can be observed in the apical part of the tooth root. There is a change in the surface of the periodontium, it becomes uneven. Over time, granulation tissue grows, which causes resorption of bone tissue in the area of inflammation. This process is often accompanied by the appearance of purulent foci, which provokes the appearance of fistulas. In some cases, soft tissue adjacent to the site of inflammation undergoes granulation. This causes the formation of granulomas of various types (submucosal, subperiosteal, subcutaneous), after opening which, fistulas appear on the face and oral cavity, and unaesthetic scars appear at the site of their healing.
Patients experiencing granulating inflammation report pain when chewing solid food, aggravated by pressure, as well as periodic exacerbations of painful conditions.
- Granulomatous
One of the forms of periapical inflammation, characterized by the formation of granulation tissue in the area of the root apex. The maturation of this tissue along the periphery provokes the appearance of a fibrous capsule that degenerates into a granuloma. Depending on the structural features, simple, epithelial and cystic granulomas are distinguished. Quite often, this form of the disease occurs as a consequence of granulating inflammation.
The course of the disease can occur according to various scenarios. Sometimes the granuloma grows slowly or does not grow at all. In this case, it usually does not cause any discomfort and is discovered by chance during an X-ray examination.
In other patients, the granuloma may enlarge, most often coinciding with exacerbations of chronic periodontitis, provoking changes in the granuloma tissue.
- Fibrous
It is characterized by the formation of a limited focus of inflammation caused by the spread of fibrous tissue. Most often this occurs after treatment of the forms of periodontitis described above, but sometimes the fibrous form occurs independently.
Often, fibrous inflammation is accompanied by excessive formation of cement, and in some cases, sclerosis of adjacent bone tissue.
An X-ray examination allows you to determine the form of chronic periodontitis. It is very important to correctly differentiate different types of disease, since the effectiveness of treatment directly depends on this.
Causes of chronic periodontitis
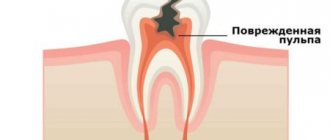
In the vast majority of cases, the cause of chronic periodontal inflammation is untreated acute pulpitis. And it, in turn, arises from neglected caries. It is not difficult to guess that the root of all troubles and complications lies precisely in carious spots, which patients tend to ignore.
It is interesting that, unlike most other diseases, periodontitis does not always have an acute stage; in some cases, pulpitis immediately turns into a chronic form of periodontal inflammation, which, without showing itself for a long time, has a destructive effect on the teeth and gums.
Quite often, the chronic stage is still preceded by an acute period of the disease, but many tend to delay treatment, preferring to relieve the pain with medication. As a result, the tooth stops hurting and the patient calms down, but meanwhile the inflammatory process gains momentum, so that later it can express itself fully.
If you do not want to become a victim of chronic periodontitis, then go for a consultation with a dentist as soon as you notice one of the following signs:
- pain that appears when chewing and biting hard foods, as well as pain of a periodic or pulsating nature;
- a feeling of a tooth protruding, preventing you from closing your jaw;
- swelling of the gums and irritation of the oral mucosa in the area of the diseased tooth;
- tooth mobility caused by periodontal destruction;
- the occurrence of one or more fistulas;
- inflammation of the submandibular lymph nodes, observed from the side of the inflammation.
Do not delay visiting your doctor, even if the symptoms are mild.
Diagnostics
In order to correctly diagnose and differentiate this type of periodontitis from fibrous or granulomatous, the dentist conducts a visual examination of the oral cavity, which allows us to identify:
- severely damaged natural tooth crown/large filling/artificial crown;
- change in color of the affected tooth;
- communication between carious and dental cavities;
- insignificant pain reaction to percussion;
- looseness of the gums, on which, after pressing with a dental instrument, a depression is formed.
During a visual examination, the specialist sees swelling of the gums, severe tooth decay, and a change in the color of the enamel. Granulating periodontitis is often observed on teeth with large fillings that have not been changed in a timely manner. Probing of pathological carious tissues does not lead to pain. When the probe is pressed on the affected mucous membrane, the gums become pale and indented. The recess is preserved for a long time. Electroodontodiagnosis is used to accurately identify granulating periodontitis. An increase in the sensitivity threshold of the pulp to 100-150 μA is detected. An x-ray is taken which shows the destruction of the jawbone.
In addition to a visual examination, dental x-rays are performed, which reveals destruction of the jaw bone, and electroodontodiagnostics, which determines an increase in the threshold of pulp excitability.
Basic principles of treatment of chronic periodontitis
The choice of treatment methods and means depends on what form of the disease is diagnosed. They can be either conservative or surgical.
The first stage of treatment will be tooth sanitation. During the procedure, the doctor thoroughly cleans the dental canals and tooth cavity, ridding them of carious lesions and infected tissues. Then all cleaned cavities are treated with special antiseptic preparations, and after the doctor is convinced that the inflammatory process has stopped, a permanent filling is placed.
In advanced and complex situations, surgical treatment may be recommended. There is no need to be afraid of this, since doctors always strive to save the tooth by removing only the infected tissue. If therapy is powerless, then resection of the root apex, tooth replantation, cystotomy or cystectomy can be performed. In this case, an effective, but most gentle method is always chosen, which allows you to achieve the desired result while minimizing unpleasant sensations for the patient. Tooth extraction, as a surgical method, is used only in the most extreme cases.
First visit
- When a patient comes to the dentist with complaints and the doctor suspects periodontitis, an X-ray examination of the jaw is initially performed to identify the source of pain.
- Then, under anesthesia, the doctor uses a drill to remove carious tissue and open access to the mouths of the tooth tubules. At the same time, the affected pulp is removed and, if necessary, the filling material previously placed there is drilled out of the canals.
- The length of the root canals is certainly measured - using a special device or directly on an x-ray.
- The channels are mechanically expanded and filled with turundums soaked in antiseptic. Without preliminary treatment, it will be difficult for the doctor to properly fill the canal to the very top. Doctors prefer to use Crezofen or its cheaper analogues as a disinfectant. The product does not contain arsenic, does not irritate locally, and is approved for the treatment of pregnant women.
- After all the manipulations, a temporary filling is installed, and the patient goes home. If the dentist deems it necessary, the patient is prescribed anti-inflammatory drugs and medications to prevent the development of allergic reactions. If the form of periodontitis is chronic, antibiotics will not be required.
Exacerbation of periodontitis: symptoms and treatment
Most often, chronic periodontitis is detected during exacerbations. It is even often initially mistaken for an acute form, but additional signs revealed by studying x-rays and the patient’s condition make it possible to establish an accurate diagnosis.
The main symptoms of exacerbation of chronic periodontitis are in many ways similar to those observed in the acute form of the disease, and the treatment regimen in both of these cases is the same. It is carried out in several stages.
At the first visit, the doctor opens the pulp chamber and removes the nerve, after which he thoroughly cleans the canals and cavity of the tooth, creating conditions for the outflow of pus. After this, the exposed tooth must be rinsed for several days with a soda solution in order to wash out the remaining purulent masses.
During the second visit, medications are placed into the canals and the cavity of the tooth, which are closed with a temporary filling. The aching tooth is left in this state for 1-2 weeks.
After this, if the control image does not cause alarm, the temporary filling is replaced with a permanent one.
In some cases, exacerbation of chronic periodontitis makes itself felt after completion of treatment. To relieve its symptoms, anti-inflammatory therapy is prescribed, which can be supplemented with physiotherapeutic procedures.
Second visit
After a couple of days, the doctor at the appointment assesses the patient’s condition - whether there are any swellings, whether the temperature has risen, whether the lymph nodes are inflamed, etc.
If no complaints are received, the doctor removes the temporary filling and turundas with cresophen, and then obturation of the root canals with temporary filling material. Its task is to help the bone tissue partially regenerate in the place where the inflammatory process was noted at the root apex. In addition, the substance sanitizes and disinfects the tubule cavity. Calcium hydroxide-based pastes are mainly used as temporary fillings: Calasept, Metapex.
From above, all this is covered with a new non-permanent filling.
Why is chronic periodontitis dangerous?
The anatomical structure of the teeth ensures in most cases the free outflow of serous and purulent masses from the source of inflammation. As a result, the patient may not be aware of the presence of chronic periodontal inflammation for a long time. All this time it is actively developing, exposing tissues to destruction. Sometimes this leads to the fact that it is no longer possible to save the tooth.
In addition to tooth loss, chronic periodontitis leads to the formation of skin or gingival fistulas and various types of granulomas, which require long-term (several months) complex and expensive treatment.
Granulomatous formations pose an additional danger. They can, under the influence of such unfavorable factors as stress or hypothermia, lead to the development of serious inflammatory processes, including sepsis.
Chronic periodontal inflammation can also accelerate the progression of diseases such as nephritis, arthritis and rheumatism, and provoke other health problems.
Prevention of periodontal inflammation
In order not to encounter chronic periodontitis, avoid complications of dental diseases such as pulpitis and caries. Treatment of caries in all cases is much simpler and faster, and it costs much less than the fight against inflammatory processes in the periodontium.
Remember that regular visits to the dentist once every six months can keep your teeth healthy and protect you from large financial expenses in the future.
In addition, strictly observe oral hygiene, using only high-quality toothpastes to brush your teeth, for example, ASEPTA SENSITIVE, which is specially designed to prevent inflammation of the teeth and gums, as well as provide gentle care for sensitive enamel. The carefully selected ratio of enzymes, thermal mud and herbs in its composition ensures maximum therapeutic and prophylactic effect.
ASEPTA mouthwash will also provide invaluable assistance in creating a healthy microflora that prevents the occurrence of periodontitis. Its regular use can significantly reduce the number of pathogenic microorganisms in the mouth, which most often cause infectious inflammatory processes.
Preventive measures also include a healthy diet. Try to eat as many fresh vegetables and fruits as possible, while simultaneously reducing the amount of sweets and carbohydrates in your diet.
Remember that some medications and orthodontic appliances can also have a destructive effect on teeth. Be sure to use additional oral care products while wearing braces and dentures, as well as in cases when you are forced to take medications that are harmful to tooth enamel.
Take full care of your dental health, and they will not make you experience pain and unpleasant emotions.