From this article you will learn:
- what are the types of gum diseases in children?
- gingivitis in children - symptoms,
- what to do if a child has an inflamed gum.
The article was written by a dentist with more than 19 years of experience.
Gingivitis in children is one of the most common dental diseases in childhood, which is accompanied by bleeding, swelling and redness of the gums. Inflammation of the gums in children is most often a consequence of insufficient oral hygiene - as a result, soft microbial plaque accumulates on the teeth, which causes inflammation of the gingival margin.
In dentistry, such gingivitis is called “chronic catarrhal gingivitis,” and according to statistics, it is observed in 90% of cases (of all cases of gingivitis in children). In the absence of timely treatment, chronic catarrhal gingivitis can transform into “Vincent ulcerative-necrotizing gingivitis.” This is the most severe form of gingivitis, which occurs with ulcerative-necrotic lesions not only of the gums, but also of the oral mucosa.
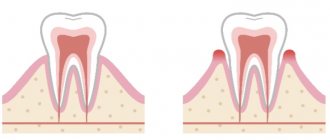
Gingivitis in children: photo
Gum disease in children also includes the concept of “juvenile gingivitis” - this is juvenile gingivitis in adolescents, which is associated with hormonal changes in the body. Its development may be associated, for example, with the accumulation of sex hormones in the gum tissue, or with the reversible process of hyperplasia of the thyroid gland. Symptoms of juvenile gingivitis are bleeding, persistent swelling of the gingival papillae, and sometimes the growth of the gingival margin on the upper or lower jaw.
The hormone-dependent form of gingivitis can develop in the prepubertal period (i.e., at the age of 7-9 years), or in the puberty period (in girls this is from 12 to 16 years old, and in boys from 13 to 18 years old). Clinical studies show that currently from 83 to 99% of fifteen-year-old adolescents necessarily suffer from one of the forms of gingivitis. But in addition to the forms described above, there are other types of gingivitis that can also occur in children.
Mild course of juvenile gingivitis –
Other forms of gingivitis in children –
- acute gingivitis,
- ulcerative gingivitis (against the background of agranulocytosis, acute leukemia, neutropenia),
- hypertrophic gingivitis (due to blood diseases, while taking medications for epilepsy, during puberty),
- desquamative gingivitis,
- plasma cell gingivitis (allergic),
- drug-induced necrotizing ulcerative gingivostomatitis (the diagnosis is made on the basis of laboratory tests, the results of which indicate sensitization of the body).
Important: we hope that all of the above will allow parents to understand that in the treatment of gingivitis in children there is no place for any kind of self-medication. And in some cases, visiting a dentist is only the first step of treatment, because... Gingivitis in a child can only be a symptom of one of the body’s diseases. In the latter case, consultations with specialized specialists, for example, an endocrinologist, hematologist, dermatologist, allergist, and pediatric gynecologist may be required. It may be necessary to conduct a general blood test (with an extended leukocyte formula), a general urine test, a test for glucose tolerance, as well as tests for the concentration of various hormones in the blood, etc.
Chronic gingivitis in children: symptoms
We have already said above that chronic catarrhal gingivitis is the most common form of gingivitis in children. And its reason lies in irregular oral hygiene. When examining a child’s oral cavity, you may find accumulations of soft microbial plaque in the neck area of the teeth. There doesn’t have to be a lot of microbial plaque (as in the photo below); For inflammation of the gingival margin, a small amount is enough.
Symptoms of chronic catarrhal gingivitis –
- bleeding gums,
- swelling of the gingival papillae (look swollen),
- bad breath,
- pain when brushing teeth,
- redness or cyanosis of the gingival margin - (red gum in a child indicates an acute phase of inflammation, but blue gum in a child indicates that the inflammation is long-term, chronic).
With chronic catarrhal gingivitis, children may not show any complaints at all, and only when questioned can they tell you that their gums bleed a little when brushing their teeth (24stoma.ru). In chronic catarrhal gingivitis, gum pain during brushing usually occurs only during periods of exacerbation (for example, against the background of colds and weakened immunity). But it is during the period of exacerbation of gingivitis that the child may develop a low-grade fever of 37.5°C and/or malaise.
Childhood gingivitis: more about the causes
The main factor in the development of catarrhal gingivitis is soft microbial plaque. Therefore, the answer to the question: why do a child’s gums bleed lies in insufficient quality/regular oral hygiene of your child. By the way, constant snacking between main meals (various snacks, candies, cookies, rolls, sweet drinks) also contributes to the growth of microbial plaque and the development of gingivitis. Insufficient hygiene leads to the accumulation of microbial plaque in the neck area of the teeth.
The bacteria that make up the microbial plaque actively produce toxins and inflammatory mediators, which cause the development of an inflammatory reaction in the gums. The latter is manifested by such symptoms as the development of swelling of the gingival margin (gingival papillae), its redness or cyanosis, as well as bleeding and pain when brushing teeth. In addition, there are additional factors that aggravate the effect of microbial plaque, contributing to the development of catarrhal gingivitis.
Local factors contributing to the development of gingivitis:
- the presence of carious cavities in the teeth,
- presence of overhanging edges of fillings,
- malocclusion (crowding of teeth),
- sharp edges of carious cavities (Fig. 1),
- wearing orthodontic appliances,
- mouth breathing,
- anomalies of attachment of the labial frenulum.
General factors contributing to the development of gingivitis: cardiovascular and gastrointestinal diseases, infectious diseases (including chronic tonsillitis). A special role in aggravating the course of chronic catarrhal gingivitis is played by blood diseases, diseases of the endocrine system (including type 1 diabetes mellitus, thyroid diseases), puberty, hereditary diseases, and oncological diseases.
Peculiarities
Gingivitis is extremely common in childhood and adolescence, as children are most susceptible to gingivitis. This is due to the increased susceptibility of periodontal disease in children.
The periodontium is a “structure” of various tissues that holds the tooth and also supplies it with necessary substances through an extensive network of blood vessels.
The incidence of gingivitis reaches its peak with the onset of middle school age, when the accelerated growth of periodontal tissue is superimposed on the “hormonal explosion” characteristic of adolescents.
Gingivitis is not uncommon in very young children, 1 year of age or younger. This is understandable, because one of the main factors in the occurrence of gingivitis is gum trauma, which is what happens during teething. And to these natural injuries is added the underdevelopment of the immune system and the weak saturation of the oral cavity of a small child with beneficial microflora.
Sometimes you can find gingivitis even in infants. Parents are advised to immediately contact a pediatric dentist if they detect any suspicious symptoms at such a tender age.
An additional risk factor may be a short frenulum of the lip, which interferes with proper gum hygiene and contributes to the accumulation of food debris. In most cases, the labial frenulum stretches on its own, but if this does not happen before the child is 2 years old, surgical resection is performed as prescribed by the doctor.
Catarrhal gingivitis in a child: how to treat
Considering that chronic catarrhal gingivitis in children occurs due to the accumulation of microbial plaque on the teeth, the most important step in treatment will be the removal of the causative factor. Therefore, treatment of gingivitis in children should first of all include the removal of dental plaque at the dentist, anti-inflammatory therapy, as well as training in proper oral hygiene.
- Removal of dental plaque –You can remove dental plaque by conducting a session of professional oral hygiene at a dentist’s appointment. Dental plaque is removed using ultrasound, after which the teeth are polished with special brushes (the procedure is painless). In Fig. 2 you can see the ultrasonic tip, which is used to remove dental plaque. Touching the tip of the nozzle to dental plaque causes destruction of the attachment of tartar to the tooth enamel.
Important : to cure gingivitis in children, treatment should primarily consist of removing soft and hard dental plaque using ultrasound. An attempt to use various rinses, gels with antibiotics and antiseptics, toothpastes with herbs (without removing plaque by a dentist) will certainly only lead to a temporary subsidence of inflammation. Drug therapy should be used only after removing tartar and plaque!
- Anti-inflammatory therapy –a course of anti-inflammatory therapy will quickly remove all the symptoms of gingivitis, as well as return loose, swollen gums to their normal state. A child's inflamed gums can be treated with the following dosage forms: antiseptic rinses and applications of anti-inflammatory gel to the gums.
Antiseptic rinses:- 0.05% CHLORHEXIDINE SOLUTION (instructions for the drug) usual course 7-8 days, rinse 2 times a day in the morning and evening - immediately after oral hygiene. It is advisable to rinse your mouth for at least 30-40 seconds, and preferably 1 minute (if the child is old enough). There are no contraindications based on age. The solution has a bitter taste. If the child cannot yet rinse his mouth on his own, then you can use a chlorhexidine solution in the form of spray irrigation.
MIRAMISTIN (instructions for the drug) rinse solution for children from 3 years old. Rinse 4 times a day for 1 minute (for 7-8 days), and for children who are not able to rinse their mouths, irrigate the gums with a spray. Miramistin is somewhat inferior to chlorhexidine in terms of potency, and besides, it is much more expensive (its only advantage in the treatment of gingivitis in a child is that Miramistin solution does not have a bitter taste).
Anti-inflammatory gels, ointments:
Questions are often asked: what to smear on a child’s gums, what gum ointment for children will be best? The best children's ointment for gums, we can probably say, is the drug "Cholisal-gel". Preparations in the form of ointment forms will be a priori less effective on the oral mucosa than gel forms of drugs. The components of ointments do not penetrate the moist mucous membrane, and also do not stay on it (they slide off and are swallowed along with saliva). Therefore, for the oral cavity you need to choose drugs only in the form of gels.
- CHOLISAL (instructions for the drug) Gel for children's gums. Active ingredients: choline salicylate and cetalkonium chloride. It has not only anti-inflammatory and antiseptic, but also analgesic effects. There are no contraindications based on age. It is applied to the gingival margin/gingival papillae – primarily from the front surface of the teeth. The course is usually 7-8 days, but no more than 10 days. Apply 2 times a day (in the morning and in the evening before bed) immediately after the end of the antiseptic rinse. After application, it is advisable not to eat or rinse your mouth for 2-3 hours (you can drink).
If you decide to treat your child yourself , then you need to know that removing dental plaque before starting treatment is mandatory. If anti-inflammatory therapy is used without removing soft and hard plaque, it will cause the following:
→ symptoms (bleeding, swelling, etc.) will certainly decrease or disappear. But, as soon as the course of treatment ends, the symptoms will arise again. This is because the cause of gingivitis (microbial plaque) was not removed and treatment was only given for symptoms.
→ transition of gingivitis from an acute form with severe symptoms to a chronic form with scanty symptoms.
In carious cavities there is a lot of infection, which causes not only tooth decay, but also inflammation of the gums. In young children, the so-called bottle form of caries often occurs, which is associated not only with poor hygiene, but also with improper feeding of the child. When treating caries in children under 3 years of age, as a rule, dental clinics use the method of silvering teeth. Despite the fact that this method does not require drilling of teeth, it has major disadvantages, and is also inferior in effectiveness to other more effective methods of treating caries in children (read more in the link above).
Prevention of catarrhal gingivitis –
WHO (World Health Organization) experts have identified the following main measures for the prevention of gingivitis:
- Proper oral hygiene –
firstly, it includes the correct technique for brushing the child’s teeth and gums, depending on the age. After all, many parents simply don’t even know at what age a child’s oral hygiene should begin. And you need to start it even before the first teeth erupt (for more information about the rules of oral hygiene in children, see the link above). - The choice of children's toothpaste - secondly, toothpastes can provide significant assistance to parents in the fight against caries and gingivitis in their children. In this case, baby pastes with special components (aminofluoride, xylitol, hydroxyapatite, a complex of lactic enzymes, etc.) that can compensate for hygiene deficiencies to a certain extent can come to the rescue. For more information about the rating of children's toothpastes, read the article at the link above.
- Balanced nutrition for children - thirdly, it is very important to follow a diet (avoid snacks between main meals), and also limit the intake of easily digestible carbohydrates - flour, sweets, cookies, as well as sweet drinks, for example, sweet soda and juices. Easily digestible carbohydrates should be given to the child only immediately after meals. After which you need to brush your teeth for 5 minutes.
Diagnosis of gingivitis
The diagnosis should be made by a doctor in a dental clinic; only through a visual examination will he be able to determine the status of the disease and differentiate it from many others, which at an early stage may manifest the same symptoms.
The main clinical signs by which a dentist can make a diagnosis are:
- the presence of erythematous formations at the gum edge;
- looseness, separation of soft tissues from the dentition, the appearance of pockets larger than 3 mm;
- when pressed with a dental spatula, exudative and bloody discharge is observed, in some cases with a putrid odor;
- obtaining the result of smears to determine the pathogen.
The last point is one of the most important in making a diagnosis and prescribing adequate procedures. Depending on the type of bacteria that caused the disease, various antibiotics and antiseptics can be used to speed up recovery. Also, after collecting an anamnesis, based on diagnostic results, the doctor needs to identify the root cause in order to further prevent the risk of relapse.
Vincent's ulcerative-necrotizing gingivitis -
This form of gingivitis can occur with severe symptoms of intoxication of the body. Visually, with this form of gum inflammation in children, the gums will be covered with a whitish or yellowish coating, there will be areas of gum ulceration, and some of the gingival papillae will be necrotic. In the acute course of Vincent's gingivitis, patients complain of putrid breath, fever, loss of appetite, headaches, as well as severe bleeding and pain in the gums. In a chronic course, the symptoms are similar, but are less acute.
The causes are ulcerative-necrotizing gingivitis Vincent most often develops against the background of untreated chronic catarrhal gingivitis - against the background of a progressive deterioration in oral hygiene, or against the background of a sharp decrease in immunity as a result of infectious diseases (including against the background of tonsillitis, chronic tonsillitis), or with the presence of severe concomitant chronic diseases (blood diseases, HIV, etc.). You can read more about the symptoms and treatment of this form of gingivitis in the article at the link above.
Hypertrophic gingivitis in children –
Hypertrophic gingivitis in children is a chronic inflammatory process of the gums, occurring with a predominance of proliferation processes (which is accompanied by an increase in tissue volume). This form occurs in 3-5% of all cases of gingivitis in children. There are two forms of hypertrophic gingivitis - 1) edematous, which occurs with persistent swelling of the gingival papillae or the gingival margin as a whole, 2) fibrous, in which fibrous growth of gum tissue occurs.
Hypertrophic gingivitis in adolescents: photo
Predisposing factors for its development:
- The period of puberty - which is associated, on the one hand, with the stimulating effect of sex hormones on the proliferation of the gum epithelium, and on the other hand, with an increase in vascular permeability in the gum tissue and the formation of excessive vascular and cellular reactions (due to which the gums may respond with the development of persistent swelling and hypertrophy even to ordinary stimuli, to which there is no reaction under normal conditions). In this case, ordinary irritants should also be understood as the usual obligate microflora of the oral cavity, which under normal conditions is not pathogenic for humans. We have already said above that such gingivitis is often also called juvenile or juvenile.
- Long-term untreated chronic catarrhal gingivitis - in combination with other provoking factors.
- Drug-induced gingival hyperplasia due to – 1) long-term treatment with anticonvulsants; 2) taking calcium channel blockers - such as nifedipine, amlodipine or verapamil; 3) taking the immunosuppressant cyclosporine-A.
- Vitamin C deficiency.
- Crohn's disease.
- Endocrine diseases, as well as blood diseases (leukemia, myeloid leukemia, thrombocytopathies, etc.).
- Chronic mechanical trauma to the gums, which is always present in patients with a deep bite, crowded teeth, when wearing braces and other orthodontic devices, as well as in the presence of overhanging edges of fillings.
Gum inflammation in children due to somatic pathology:
Important: most often, hypertrophic gingivitis occurs with a combination of predisposing factors. For example, during puberty in children who simultaneously have malocclusion (crowding of teeth, open or deep bite, small vestibule of the oral cavity). Or during puberty - if the child has untreated chronic catarrhal gingivitis, which we described in detail above, etc.
Vulnerability zone
Let's look at gum disease in children. Your child's healthy gums are delicate and very vulnerable tissue of a pale pink color. Unlike adult gums, they can be easily injured, but they are capable of rapid regeneration. Another peculiarity of children's gums is that they often reflect the general condition of the body, being a litmus test for systemic diseases.
The most common diseases of the gums and periodontal tissues: gingivitis is an inflammation of the gums that occurs as a result of the adverse effects of local and general factors, occurring in 80% of children; gum atrophy, which develops in more than half of the child population; various types of childhood stomatitis, which most often occurs in infants and preschoolers; Periodontitis is a disease in which all periodontal tissues become inflamed and affects up to 5% of young patients. Periodontal disease (dystrophic changes in periodontal tissue) and other pathologies practically do not occur in childhood.
Desquamative gingivitis in a child –
Desquamative gingivitis in a child is manifested by soreness of the gums when brushing teeth, swelling and bleeding of the gums (most often this form of gingivitis occurs in the area of the front teeth). Upon examination, you can find that the gums have a bright red color, they are usually sharply painful on palpation, and have a loose consistency. Due to the loss of keratin, the gums become more susceptible to traumatic effects.
Desquamative gingivitis in a child, teenager -
Desquamative gingivitis most often develops against the background of untreated chronic catarrhal gingivitis, i.e. as a result of the long-term influence of bacterial pathogens on the gum mucosa. Factors contributing to the disease are metabolic disorders, infectious diseases, Crohn's disease or other somatic pathologies. In addition, desquamative gingivitis can be a symptom of dermatoses - such as lichen planus, pemphigus vulgaris.
Very often, desquamative gingivitis occurs during puberty (more often in girls). The latter is due to the fact that in girls during puberty the hormone progesterone predominates, and the concentration of estrogen, on the contrary, is reduced. A decrease in estrogen content leads to a decrease in cell keratinization and partial loss of the protective keratinizing membrane of the gum.
Plasma cell gingivitis (allergic) –
With plasma cell gingivitis, we see that the gum has a bright red color, as a rule, it is swollen and increased in size (in the initial stages and a limited volume of the lesion - the volume of the gum may not be increased). The process consists of plasma cell infiltration of the gum, namely its subepithelial layer. Infiltration of the gums by plasma cells occurs as a hypersensitivity reaction to certain antigens - especially often to various flavors or spices.
Plasma cell gingivitis in a child, teenager -
Thus, an allergic reaction can occur to the components of chewing gum, toothpastes, and lollipops. Plasma cell gingivitis often develops in children due to cinnamon and other flavorings contained in baked goods and confectionery products, as well as various drinks. Often the cause can be absolutely any product containing natural herbal ingredients.
Treatment should consist of identifying and eliminating the causative factor (allergen). In case of a generalized, pronounced process and the formation of periodontal pockets, local anti-inflammatory treatment is additionally carried out in combination with systemic antibacterial therapy with azithromycin. Early correct diagnosis is very important, because plasmatic gingivitis has similar clinical manifestations in the oral cavity, which can be observed with leukemia, HIV infection, discoid lupus erythematosus, lichen planus, and desquamative gingivitis.
Prevention
The main means of preventing gingivitis, as well as other dental diseases, is oral hygiene. From a very early age, teach your child to brush their teeth for at least 10-15 minutes, making sure to pay attention to the inside of the teeth. Buy your child a therapeutic toothpaste and make sure he brushes his teeth correctly. To eliminate stubborn plaque, you can use a brush with moderately hard bristles. After brushing, teeth should be rinsed thoroughly.
Teach your child to use dental floss to remove food debris from between the teeth. But keep in mind that dental floss can also injure the gums if used incorrectly, so it is not recommended to use dental floss for a child under 3 years of age.
Modern dentistry does not encourage the use of toothpicks for dental care, since their use risks not only injuring the gums, but also causing infection. Give preference to dental floss.
If tartar has formed in your child’s mouth, then a visit to the dentist is essential. The doctor will remove tartar in the most gentle way possible.
Gingivitis against the background of herpetic stomatitis –
Very often, with viral herpetic stomatitis, concomitant acute gingivitis occurs. In this case, the periodontal papillae and the marginal part of the gums increase due to swelling and become bright red. Read more about gum inflammation due to stomatitis in the article: “Treatment of various forms of stomatitis in children.” We hope that our article on the topic: Gingivitis in children treatment was useful to you!
Sources:
1. Dental education of the author of the article, 2. Based on personal experience as a dentist, periodontist, 3. The European Academy of Paediatric Dentistry (EU), 4. National Library of Medicine (USA), 5. “Pediatric therapeutic dentistry. National leadership" (Leontyev V.K.).