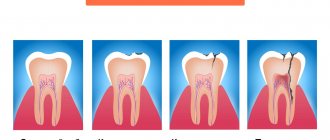
Chronic periodontitis is one of the forms of the disease that occurs due to the fact that pathogenic microorganisms penetrate into the periodontal tissue through the openings of the root canals located at the tops of the dental roots. Chronic periodontitis of the roots is accompanied by a violation of the integrity of the ligaments that provide fixation and stability of the tooth, destructive processes of bone tissue and can lead to the formation of granulomas and large cysts.
Chronic periodontitis is a pathological process in the periodontal tissues. This is associated with the development of inflammation in the periodontium and the formation of fibrous, granulating, granulomatous tissue. In the chronic form of the disease, exacerbations periodically occur, during which swelling of the gums, loosening of teeth, the appearance of fistulas with the release of pus, etc. are observed. Specialists identify this pathology and distinguish it from similar diseases using electroodontometry, X-rays and visual examination. Lack of proper treatment leads to tooth loss due to weakening of the ligamentous apparatus and the growth of large capsules with pus.
Filling made of light-curing material for classes I and V - 2,000 rubles.
Filling made of light-curing material in classes II, III, IV - 3,000 rubles.
Placing a temporary filling - 400 rubles.
Resection of the root apex (frontal group) - 6,500 rubles.
Resection of the root apex (chewing group) - RUB 9,000.
Mechanical and medicinal treatment of canals for periodontitis (1 canal) - 1,100 rubles.
Closing perforations (MTA) - RUB 6,500.
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 1,000
- The cost of an orthodontist consultation is 2,000
Make an appointment
Symptoms of the disease
General symptoms depend on the form of the pathology. When granulomas form, attacks of pain are observed when exposed to hot food. Pressure on the affected tooth and gum is accompanied by pain. The size and density of the mucosa in the affected area changes, and a granuloma forms under the bone or mucosa.
An exacerbation is accompanied by the appearance of fistulas, which grow and gradually release their contents into the oral cavity. In this case, purulent fistulas can appear not only on the gums, but also on the cheekbones, cheeks, neck, and chin. Isolation of pus may be performed along with the isolation of granulosa tissue. Then the fistula goes away, and a scar appears in its place.
The granulomatous form occurs for a long time without pronounced symptoms. Only after the granuloma grows to a large size and cysts form, the main symptoms appear: discoloration and severe pain in the tooth, development of gumboil and swelling of the gums in the affected area. Cysts that are too large can cause a jaw fracture and long-term rehabilitation.
Fibrous periodontitis is the most hidden form of pathology. There is no pain when chewing food or drinking hot drinks. Severe symptoms are observed only during exacerbation. There is general poisoning of the body due to the penetration of pus into the blood, the tooth becomes loose, and the lymph nodes in this area become larger.
Retrograde periodontitis
This form of the disease is quite rare. Periodontitis of this form begins to develop against the background of infection penetration into the periodontium through the blood flow or lymph flow.
Traumatic periodontitis
Periodontitis of traumatic origin appears against the background of trauma, when a person receives a sufficiently severe bruise. Some medical errors made during dental treatment can lead to traumatic periodontitis:
- A small piece of an instrument that was “forgotten” after treatment in the cavity of the dental canals;
- Re-filling of the dental canal, which consists of excessive filling of filling material, which ultimately protrudes beyond the apical part of the tooth root;
- Incorrectly restored natural tooth crown, prosthesis, which constantly injure the tissues of the oral cavity.
Toxic periodontitis
This form of periodontitis usually occurs after poorly treated caries, and can occur due to tissue irritation caused by certain medications.
Each form of periodontitis has its own symptoms, but inflammation in the periodontium can also be determined by some general signs:
- Pulsating and clearly localized pain, the intensity of which gradually increases. The pain impulse intensifies at the slightest attempt to touch the teeth, during the period of their closure, while eating;
- The appearance of elevated body temperature due to toothache;
- Feeling of fullness in the area of the inflammatory process;
- Swelling of soft tissues.
IMPORTANT: Severe symptoms during the development of periodontitis are not present in all cases. Some phases of the disease can occur without the slightest external signs at all, or the person feels slight discomfort, which he mistakes for ordinary caries. Professional dental examinations, which are recommended to be carried out at least once every six months, will help to identify periodontitis in a timely manner for treatment.
Causes of chronic periodontitis
Chronic periodontitis appears in the absence of treatment of the acute form. The disease develops due to traumatic, toxic, infectious, mechanical effects on tissue.
The infectious form develops due to the penetration of pathogenic microorganisms into the oral cavity. This is due to damage to soft tissues by staphylococci, diphtheroids, and streptococci. The penetration of bacteria into tissues occurs through the openings of the root canals or through the hematogenous route. Often the infection progresses against the background of osteomyelitis, sinusitis, periodontitis, and tonsillitis.
The fibrous form often progresses after severe trauma. For example, after tissue destruction with a pin, filling, or crown. Pathology can also develop due to a strong blow.
Drug-induced periodontitis occurs due to the use of drugs that provoke coagulative necrosis of the periodontal ligament. These include resorcinol-formalin and arsenic paste. Tissue poisoning is provoked by local anesthesia, iodine, acids, etc.
Indications
The lack of a positive result after conservative and surgical treatment is the main indication for removal of affected teeth. Extraction is performed for the following symptoms:
- Significant damage to the crown.
- Severe loosening of the tooth.
- Formation of large cysts and granulomas.
- Impossibility of performing the operation due to obstruction of the canals.
- Lack of results with surgical and conservative treatment.
Contraindications
- Oral infections.
- Allergy to anesthesia.
- Intolerance to antibiotics and antimicrobial agents.
- Acute diseases of the cardiovascular system.
- Poor blood clotting.
Treatment of periodontitis
The treatment regimen for the disease is determined by the stage of its progression and the specific clinical picture. The doctor pays special attention to finding out the cause that provoked periodontitis.
The traditional method of treating the disease includes: the use of pastes that promote the resorption of granulomas and cysts, as well as drugs that activate the restoration of bone tissue. Resection of the apex of the tooth root is prescribed only if therapeutic methods do not bring the expected result. In any case, the doctor strives to preserve the integrity of the tooth as much as possible.
The most important thing in treatment is pain relief and elimination of the source of inflammation in order to spread the infection to other areas of the maxillofacial area. In case of mild infectious periodontitis, it is enough to clean the root canals using an antiseptic.
In case of acute periodontitis, it is necessary to drain the exudate from the canal through the root or gingival canal or the hole remaining after tooth extraction. Then the doctor prescribes antibiotics (sulfonamide medications). If the pain is severe, then analgesics are also prescribed.
After the acute inflammation has been relieved, the doctor begins cleaning the root canal and administering medications. If there is no discharge from the root canals and no pain, the canals are sealed. If exudate is released, then drainage of the canal cavity will follow.
If periodontitis has developed as a result of the action of strong drugs, then treatment begins with eliminating the cause that provoked the disease. First, you should reduce the intoxication of periodontitis by reducing exudation and draining the contents from the root canal. This can be done through mechanical treatment or antidotes that reduce the release of exudate.
If periodontitis is caused by injury, then treatment will be aimed at eliminating it. For example, it may be necessary to grind off a filling that injures the gums. If the damage has led to tooth displacement or damage to a bundle of blood vessels, then it is necessary to check the tooth for electrical excitability. This examination will help identify a possible tooth root fracture.
Treatment of chronic periodontitis is similar to treatment of the purulent type. In this case, the canal is drained to drain the exudate. Next, using an X-ray image, the location of the source of inflammation is clarified, in particular, it is clarified which of the canals should be cleaned first. After relief of inflammation, antimicrobial and instrumental treatment of the root canals is carried out, often using impregnation or physical methods of therapy.
It is worth understanding that after periodontitis, a relapse may occur if the patient soon froze in the cold or suffered another injury. The latter will inevitably lead to tooth extraction and implantation.
Types of chronic periodontitis and their clinical manifestations
It is customary to distinguish several forms of the disease, the diagnosis of which is necessary in order to correctly prescribe treatment for chronic periodontitis. To do this, the dentist conducts a visual examination of the oral cavity, prescribes electroodontic diagnostics and x-rays.
Chronic fibrous periodontitis
Self-diagnosis of this type of chronic periodontitis is very difficult due to the almost complete absence of clinical manifestations.
The patient does not experience pain, and there is no reaction to temperature stimuli. During the examination, the dentist notes a change in the color of the tooth, the presence of a reaction to percussion and painful probing. The tooth cavity is filled with dead pulp, which emits a putrid odor. The X-ray image clearly shows the increase in the periodontal fissure at the root apex; there is no destruction of bone tissue and cement.
Chronic granulating periodontitis
The painful sensations characteristic of this type of chronic periodontitis are not significant.
There are sensations of heaviness and fullness, and minor pain may be present when exposed to mechanical stimuli. Exacerbation of chronic granulating periodontitis is accompanied by the formation of a fistula through which pus comes out or granulation tissue grows. With this disease, the gums become loose. When pressing on the inflamed area with the blunt end of a dental instrument, a small depression appears, which disappears only after some time. The x-ray image shows the focus of the destructive processes of bone, dentin and cement.
Chronic granulomatous periodontitis
The symptoms of chronic periodontitis of this type are also practically invisible to the patient. Sometimes minor discomfort and pain may occur when biting on the affected tooth.
An examination by a dentist can reveal a change in the color of the crown of the tooth, but a carious cavity is not necessarily present. Remnants of dead pulp are found in the root canals. If the canals were previously sealed, then the quality of the filling is not good enough.
An X-ray image allows you to determine the destruction of bone tissue, which has a round shape. Often this process can be found on dental tissues or the root apex area.
Diagnostics
Diagnosis of periodontitis is carried out on the basis of a clinical examination, including:
- interviewing the patient,
- visual examination of the oral cavity,
- probing the entrance to the tooth cavity,
- determination of the degree of tooth mobility.
To accurately establish a diagnosis in dentistry, the following is used:
- X-ray examination;
- radiovisiography;
- transillumination;
- electroodontodiagnostics.
In case of acute inflammation, an X-ray image will not yet show any changes in the periodontium, but in the chronic course of the disease, an X-ray is simply necessary. With its help you can determine the form of chronic periodontitis:
– with fibrous periodontitis, the image will show uneven changes in the lumen of the periodontal fissure; sometimes there is thickening of the root in the apical region. In some cases, sclerosis of the alveolar bone tissue is observed around the source of inflammation.
– with granulating periodontitis, more or less extensive granulations (growths) appear in the periodontium, usually round in shape with unclear boundaries. The image also shows a pronounced deformation of the periodontal fissure and reduced bone density.
– with granulomatous periodontitis, it is clear that the growing granuloma (round in shape with clear boundaries) gradually destroys the bone tissue of the alveoli, developing into a cystogranuloma, and then into a cyst, which begins to grow from the apex of the tooth towards the bone tissue. Such a pathological process usually requires surgical intervention.
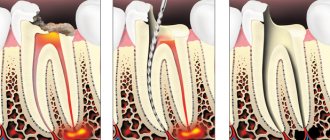
Treatment of the chronic form
Good patency of the canals allows for therapeutic treatment:
- Opening a tooth.
- Antiseptic treatment.
- Cleaning the channels.
- Use of anti-inflammatory drugs.
- Installation of a temporary filling.
After the procedure, antibiotics are prescribed and re-appointed after 3 months. If the x-ray shows a cure for the disease, then the canals are treated with an antiseptic and a permanent filling is installed. Surgical intervention involves cystectomy, resection of the upper part of the root, hemisection, and root removal. Lack of results after treatment is a reason for extraction of the diseased tooth.
Exacerbation of periodontitis: symptoms and treatment
Most often, chronic periodontitis is detected during exacerbations. It is even often initially mistaken for an acute form, but additional signs revealed by studying x-rays and the patient’s condition make it possible to establish an accurate diagnosis.
The main symptoms of exacerbation of chronic periodontitis are in many ways similar to those observed in the acute form of the disease, and the treatment regimen in both of these cases is the same. It is carried out in several stages.
At the first visit, the doctor opens the pulp chamber and removes the nerve, after which he thoroughly cleans the canals and cavity of the tooth, creating conditions for the outflow of pus. After this, the exposed tooth must be rinsed for several days with a soda solution in order to wash out the remaining purulent masses.
During the second visit, medications are placed into the canals and the cavity of the tooth, which are closed with a temporary filling. The aching tooth is left in this state for 1-2 weeks.
After this, if the control image does not cause alarm, the temporary filling is replaced with a permanent one.
In some cases, exacerbation of chronic periodontitis makes itself felt after completion of treatment. To relieve its symptoms, anti-inflammatory therapy is prescribed, which can be supplemented with physiotherapeutic procedures.
Exacerbation of chronic periodontitis
Often patients seek treatment for acute chronic periodontitis, which manifests itself quite clearly. This mainly applies to granulomatous and granulating types, exacerbations of which occur much more often than fibrous types. Clinical manifestations during this period include:
- constant localized pain;
- swelling of soft tissues;
- the presence of a reaction to mechanical stimuli;
- painful reaction of the lymph nodes.
Forms of periodontitis
Depending on the location of the inflammatory process, periodontitis is distinguished:
- apical (or apical) – the source of infection is located between the wall of the dental alveolus and the apex of the dental root;
- marginal (or marginal) - inflammation occurs from the edge of the injured gum.
Based on the nature of the inflammation, serous and purulent periodontitis is distinguished, as well as fibrous, granulomatous and granulating.
Classification of periodontitis
There are several classifications of periodontitis, which have more similarities than differences. However, in our country, the classification of I. G. Lukomsky, which provides for the separation of acute (serous and purulent) and chronic (fibrous, granulating and granulomatous) apical periodontitis, as well as chronic aggravated periodontitis, has become most widespread.
Classification of periodontitis according to I. G. Lukomsky is as follows:
- Acute forms.
- Acute serous apical periodontitis.
- Acute purulent apical periodontitis.
- Chronic forms.
- Chronic apical fibrous periodontitis.
- Chronic apical granulating periodontitis.
- Chronic apical granulomatous periodontitis.
- Aggravated chronic apical periodontitis.
- Root cyst.
Recommendations after treatment
After conservative or surgical treatment, you should not eat food for 2-3 hours due to the effects of anesthesia. Pain may be experienced for 7 days after surgery. It is recommended to rinse your mouth with antiseptics and a decoction of medicinal herbs. For severe pain, it is recommended to take painkillers. If pain persists and severe swelling is observed, contact your doctor immediately.
At the same time, the crown of the tooth changes its color, the presence of a carious cavity and tooth mobility are noted. Dentists at the CELT clinic successfully treat even the most advanced and severe forms of chronic periodontitis!
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Methods for diagnosing periodontitis
Acute periodontitis is usually diagnosed during examination by a dentist based on the clinical picture and patient complaints.
The difficulty of diagnosing chronic periodontitis is due, first of all, to the fact that the patient does not have sufficient motivation to see a doctor. A fairly typical situation is when the tooth initially hurt (in the stage of pulpitis), and then the pain disappeared. But the inflammatory process continues. And the longer treatment is delayed, the less opportunity there is to save the tooth. To avoid negative consequences, Family Doctor dentists recommend undergoing a dental examination at least once a year.
Orthopantomogram
As part of your annual dental examination, your doctor may recommend an orthopantomogram, a panoramic photograph of your teeth taken using a special X-ray machine (orthopantomograph). X-rays will help identify chronic periodontitis and determine the choice of treatment method.
More information about the diagnostic method
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Treatment quality criterion
High-quality, effective treatment of periodontitis requires pinpoint precision when working in tooth canals that have a complex shape and individual anatomical features. Obturation (sealing) of canals is based on the principle of “three pillars”: the canal must be sealed to its entire length, along all micro-branches, without pores and air cavities. This requires high qualifications and extensive experience of the attending physician, as well as the use of modern equipment - endomotors, apex locators, files, dental microscope. Modern endodontic treatment is a high-tech medical procedure and is based on new medical, technological and ergonomic principles, which obliges clinics to be equipped with modern equipment, and doctors to regularly improve their level of professional competence.
Therapeutic treatment
Chronic periodontitis is often successfully treated with therapy. To do this, the carious area is prepared and the old filling is removed. Continuous treatment of the affected area with an antiseptic is mandatory. After removing the old filling, measures will be needed to ensure the unimpeded outflow of exudate and rinsing the cavity with an antiseptic.
The following measures will help enhance the effect:
- Phonophoresis with the introduction of an antiseptic under the influence of ultrasound into microtubules.
- Electrophoresis with potassium iodide and other antiseptics, in which molecules quickly form polarized ions.
- Laser treatment. The laser affects the disease in two ways at once: it sterilizes the root canal, removing bacteria, and releases special oxidizing agents that arise under the influence of radiation from more complex molecules as a result of their breakdown.
Elimination of the disease at the acute stage is carried out, starting with the demobilization of the factors that led to this condition. Antiseptic is not enough for this. Good drainage will be required, as well as antibacterial therapy.
When the root cause of the exacerbation is destroyed, with granulating periodontitis the doctor acts on the tissue using various means (calcium hydroxide). The same measures are taken in the case of the granulation form.
At the end of therapy, the tooth is sealed, as well as the canal is filled, if the patient has no complaints.