- An effective way to preserve the integrity of the tooth and prevent the spread of infection.
- Modern painless methods of performing the procedure.
- The fastest possible return to normal life.
Sign up for a consultation
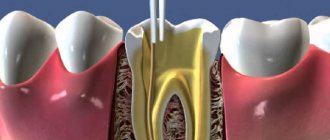
Once the pulp (nerve tissue and blood vessels) is removed, the tooth becomes hollow. If it is not filled with filling material, then the process of spreading caries and other infections will continue. Pathogenic microflora can lead to damage to the periodontium - the tissues surrounding the root of the tooth, in which case there is a high probability of its loss. In addition, the spread of infection can lead to the formation of cysts and fistulas, the appearance of sinusitis and osteomyelitis. In order to prevent this, obturation (filling) of the canal of the pulpless tooth is performed.
Indications and contraindications
|
|
Materials for root fillings
Prices for dental canal filling depend on the chosen procedure method and the consumables used. We, as modern dentistry, use:
- plastic material, gutta-percha, for the main filling of the tooth canal
- and special sealers and pastes to ensure maximum tightness.
Gutta-percha is the most modern material with antibacterial activity. It does not dissolve and does not lose its properties throughout the life of the tooth. The sealer we use (AH plus, Dentsply, USA) is recognized as the “gold standard” for root canal treatment all over the world.
Canal filling techniques
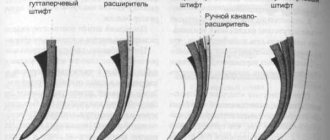
Lateral condensation method
Vertical condensation of gutta-percha
A simple and effective way to fill root canals. The doctor applies a liquid paste to the gutta-percha pin, after which the latter is inserted into the tooth cavity. Using the tool, the cavity is filled with additional pins, which completely seal the canal.
This is a method of filling tooth canals with a complex shape (anatomy). Using a special thermal nozzle, the doctor introduces heated and softened gutta-percha into the canal.
Instrumental treatment of formed dental root canals
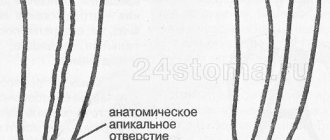
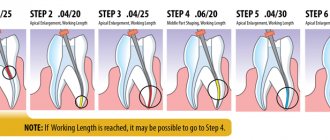
Endodontic treatment of permanent teeth that already have a fully developed root canal system is carried out using methods used for adult patients. During the treatment process, the doctor’s main tasks are to give the cavity a funnel shape with minimal expansion in the area of physiological narrowing and maximum expansion at the entrance. The specialist also needs to ensure that the position of the apical foramen remains unchanged and form a reliable stop for the filling material. During the instrumental treatment of permanent teeth, it is recommended to regularly rinse the cavity. K-reamers, as well as H- and K-files can be used to scrape tissue from the canal walls. The preparation technique can be based on one of the following methods:
- Step-back. Also known as the apical-coronal technique or “step back”. Involves the expansion of root canals from the apical foramen towards the orifices. Requires the use of tools with ever increasing diameter sizes.
- Step-down. This technique is also called “step forward” or coronal-apical. In this case, canal processing is performed in the opposite direction to the previous method: from the root orifices to the apex.
- Combined. This hybrid method involves the use of two techniques at once. As a rule, at the initial stage, the crown is processed using the step-back principle, after which the canals are developed using the step-down method.
Treatment regimen
- Diagnostics Before treatment, an x-ray or computed tomography must be done to determine the number of channels, their location and shape.
- Anesthesia The doctor selects an anesthetic and, if necessary, conducts sensitivity tests to various drugs.
- Installation of a rubber dam An obligatory aspect of modern treatment is the isolation of the tooth from oral fluid using a special latex scarf (rubber dam).
- Instrumental and medicinal canal treatment The essence of root canal treatment is high-quality disinfection of the tooth cavity. To do this, the doctor expands the canal with instruments, gives it the desired shape and rinses it with disinfectant solutions to destroy the infection.
- Preparing the canals The doctor measures the length of the canals using an apex locator, after which they are mechanically expanded and smoothed out the walls.
- Filling canals Cement, a pin, or a combination of both are injected into the prepared cavities, depending on the chosen treatment method.
- Control image The doctor evaluates the quality of canal filling, after which he performs tooth filling and other necessary procedures. In addition, the patient receives recommendations for further oral care.
Instrumental treatment of root canals of temporary teeth
In this case, specialists do not need to give the cavity being treated a standard cone shape, since this can lead to dangerous thinning of the very fragile walls. The main task in the canal treatment process is to remove infected predentin and create an apical stop. However, reamers are used only when it is necessary to process very narrow cavities. In most cases, H-files are used during the treatment process. The diameter of the instrument increases as it goes deeper into the root canal. There is no standard for the amount of expansion of the internal root cavity. But in practice, the canals of molars are usually increased to 25-35 sizes, and of the front teeth - to 70-90 or more. The main requirement is that the expansion of the cavity should not exceed 2-3 times the size of the original size of the apical section. It is also recommended to correctly prioritize by preparing the more complex mesial and buccal canals of molars first.
Temporary canal filling
If indicated, the doctor can fill the canals after depulpation not with filling material, but with a medicinal agent (antibacterial, anti-inflammatory). The drug remains in the tooth cavity for a certain time, after which it is removed, and the vacated canal is sealed.
The procedure can be prescribed:
- if there is a need to sanitize the canals if a deep infectious process is suspected;
- if the patient has acute periodontitis;
- for temporary sealing of the canal, if it is necessary to monitor the condition of the tooth cavity after removal of the inflamed pulp.
In addition, the procedure can be prescribed for tooth injuries, for example, a fracture of the crown or root.
Drug treatment
- hydrogen peroxide
Preparations for expanding the root canal.
Root canal enlargement preparations generally contain ethylene diamine tetraacetic acid (EDTA), which dissolves the inorganic components of dentin. Dentin calcium combines with EDTA to form a stable chelate. Also, such preparations often include carbamide peroxide and distilled water.
Endolubricants can be produced in either liquid or gel form. Gels are more convenient, as they “lubricate” the canal walls and prevent jamming of the endodontic instrument.
Preparations for antiseptic treatment of the root canal.
Hydrogen peroxide and chlorine-containing products.
- Hydrogen peroxide. A 3% hydrogen peroxide solution is used to flush the canal. Upon contact with tooth tissue, peroxide dissociates with the release of atomic oxygen (bubbles). This has an antiseptic effect (on anaerobic bacteria) and promotes mechanical cleansing of the canal. Has a hemostatic effect.
- Chlorine-containing products. (0.2-1% chlorhexidine, 3-5% sodium hypochlorite, 2% chloramine). Dissolves necrotic tissue, has a bactericidal effect on Gr+ and Gr- bacteria, fungi and viruses.
- sodium hypochlorite – has a pronounced antiseptic effect due to the formation of chlorine gas. Has the ability to penetrate dentinal tubules. Dissolves remaining organic matter in the canal. ATTENTION – do not move beyond the apex.
In case of contact with periapical tissues – sharp pain, profuse bleeding, development of edema (aseptic inflammation)
Currently, the root canal is treated according to the following scheme: sodium hypochlorite - after each change of instrument and after the end of mechanical treatment of the canal, then - hydrogen peroxide, then - distilled water.
Iodine preparations, nitrofurans.
- Iodine preparations –
- 1% iodinol solution (blue) - a compound of iodine with polyvinyl alcohol, has a strong bactericidal and fungicidal effect, stimulates the phagocytic activity of leukocytes, accelerates tissue regeneration. It is an indicator upon contact with tissue decay products, microbes, purulent discharge - it loses its dark blue color and becomes white.
If, when turunda with iodinol is introduced into the root canal, it retains its color, the root canal is clean. Iodine preparations can be used as an antidote to arsenic in acute arsenic periodontitis. A cotton swab or paper point soaked in one of the iodine preparations (5% unithiol solution, 1% iodinol solution, 3–5% iodine tincture) should be inserted into the root canal and left in it for 1–2 days.
ATTENTION! – before using iodine preparations, it is necessary to find out whether the patient is allergic to iodine.
2. Nitrofurans (0.5% furatsilin, 0.1-0.15% furadokin, fursalidone) - These drugs have a strong bactericidal effect, including on those microorganisms that are resistant to other medications. This is due to the influence of nitrofurans on the enzymes of microbial cells. In addition, nitrofurans enhance the phagocytic activity of leukocytes and have a pronounced anti-exudative effect.
Quaternary ammonium compounds
0.1% decamine solution. It has a bactericidal effect on spore-forming microorganisms and yeast-like fungi.
Dimexide, dimethyl sulfoxide
It has antiseptic, anti-inflammatory, analgesic, bacteriostatic, fungicidal effects.
Proteolytic enzymes (trypsin, chymotrypsin, lysozyme):
– selectively break down necrotic masses;
– thins exudates, viscous secretions, blood clots;
– accelerate the outflow of exudate from the source of inflammation without causing harm to living periodontal tissues;
– stimulate phagocytosis;
– destroy bacterial toxins;
– have anti-inflammatory and anti-edematous effects;
– enhance the effect of antibiotics and other medications on the microflora of the root canal.
Widely used for washing root canals in the treatment of acute and chronic periodontitis.
Enzymes can be used either alone or in combination with antibiotics and sulfonamides under a bandage that is left in the root canals for the period between visits, but not more than 1–2 days.
It is important to know
that when treating the root canal with proteolytic enzymes,
you cannot
simultaneously use other antiseptics, alcohol and ether, which inactivate both enzymes and antibiotics.
Methods of medicinal treatment of root canals.
- on Turunda:
A cotton turunda is wrapped around the endodontic instrument, moistened with an antiseptic, and inserted into the root canal.
- Using a paper pin
. A dry paper pin is inserted into the root canal, after which an antiseptic is dripped onto it (with tweezers), then the pin is removed from the canal.
- Using an endodontic syringe.
Special needles for the endodontic syringe are used (hole on the side) so that the antiseptic is not discharged into the periodontium.
RULES FOR WASHING THE CHANNEL FROM A SYRINGE:
- Always use only endodontic needles
- never push the needle deeper than ½ channel
- never inject antiseptic under pressure
- make sure that the needle does not “jam” in the canal
— With sound or ultrasonic treatment
– antiseptic is used as a coolant. It is advisable not to use strong antiseptics, as there is a risk of their penetration into the periodontium.
Preparations for antiseptic dressings.
Phenol derivatives.
Antiseptic dressings are medications that are placed in the tooth cavity, hermetically sealed with temporary filling material and left between visits. Used for:
- destruction or reduction of bacterial flora remaining in the root canal after its instrumental and medicinal treatment, especially with destructive changes in periodontal tissues;
- preventing or reducing pain;
- reducing the inflammatory process in the periodontium
- stimulating bone tissue regeneration during destructive processes in the periodontium.
Application rules: the root canals are treated mechanically and medicinally, dried, a cotton swab is moistened with an antiseptic, wrung out well, and placed on the bottom of the tooth cavity.
Phenol derivatives have a strong bactericidal effect;
- combine well with other drugs (glucocorticoids, antibiotics, etc.)
- When used correctly, there are no side effects from the periodontium.
- Phenol derivatives:
1) Eugenol – essential oil.
Eugenol is a chemical derivative of clove oil, related to phenol.
It has a mild antiseptic and pronounced analgesic effect. At the same time, eugenol has an irritating effect on living periodontal tissue. Used as a therapeutic dressing, which is left in the root canal for 72 hours. During this period, the released antiseptic vapors provide the greatest bactericidal effect.
2) Camphorophenol
It is an oily liquid consisting of 5 parts camphor, 3 parts phenol and 2 parts liquid petroleum jelly.
Has a weak disinfectant effect. Used as an antiseptic dressing. Before inserting into the tooth cavity, a cotton ball moistened with camphorophenol is squeezed out well so that excess drug does not penetrate into the periapical tissues.
It can be used in conjunction with arsenic paste, covering it with a wrung-out swab on top, which promotes better diffusion of arsenic into the tissue.
An analogue of camphorophenol is “Cresoden”, produced domestically, which contains camphor and parachlorophenol.
Contains a corticosteroid hormone - declamethasone and strong bactericidal substances - parachlorophenol, thymol.
It has a pronounced anti-inflammatory and antiallergic effect. Used for treating root canals before filling in the treatment of pulpitis and periodontitis.
Shown
as an antiseptic dressing for 2–3 days:
- in the treatment of difficult-to-pass canals;
- impossibility of complete pulp excision;
- with a pronounced inflammatory reaction of periodontal tissues.
3) Preparations "Rockle"
The composition includes phenol, formaldehyde, guaiacol, dexamethasone.
They differ from each other in the amount of formalin included in each drug
Aldehydes and antibiotics.
Aldehydes.
1) Formaldehyde
– the most popular antiseptic in domestic endodontics. Formalin is the main substance of the resorcinol-formalin method.
Formaldehyde, penetrating into the dentinal tubules of the root, converts the albumins located there into insoluble and aseptic mixtures, resulting in deep sterilization of the dentinal tubules.
2) “Abscess remedy liquid”
(PD Germany). The drug contains 40% formaldehyde, creosote, thymol and alcohol, and has a strong antiseptic and bactericidal effect.
3. Antibiotics.
Of greatest interest for endodontics are antibiotics with a pronounced local antimicrobial effect (chloramphenicol, erythromycin, gentamicin, neomycin), as well as their combination with corticosteroids and enzymes.
However, the widespread use of antibiotics contributes to the emergence of new forms of microorganisms that are resistant to antibiotics. When treating periodontitis, it is recommended to use a combination of two or more antibiotics and only taking into account the sensitivity of the microflora isolated from the root canals before starting treatment
.
Hemostatic agents.
- 3% hydrogen peroxide solution (H 2 O 2 )
- "Katalyugem" (Moscow)
Stops bleeding due to the content of aluminum chloride, and also has powerful antiseptic properties due to the presence of catamine AB. The drug is a clear liquid that does not irritate the tissues in contact with it.
To achieve hemostasis, it is introduced into the root canal on a turunda or paper pin for 40 seconds - 1 minute. If bleeding is not stopped completely, repeat the procedure.
- Racestyptine
It has a hemostatic effect due to the presence of aluminum chloride in it. Used to stop apical bleeding and bleeding from the perforation area.
- Solutio
Adrenalini hydrochloridi 0.1%
Stops bleeding due to local vasoconstrictor action. A turunda or a paper pin moistened with an adrenaline solution is inserted into the root canal.
6