How a bite is formed What a correct bite looks like Types Definition of a bite Possible consequences Methods of correction
Teeth bite is the relative arrangement of the dentition when the jaws are completely closed.
The formation of the dental system begins in intrauterine development. By the 11th week, the fetus has jaw stripes. Almost all children are born with malocclusion. The lower jaw is moved back. Dentists call this phenomenon retrognathia. When a baby actively sucks, the muscles are trained. By 6-8 months with breastfeeding, and a little later, with artificial feeding, the lower jaw takes the correct position. For bottle-fed children, it is necessary to monitor the position of the body and the hole in the nipple. If the formula does not flow from the bottle, you have to make an effort to get it, the child’s tongue and jaw muscles receive sufficient stress and malocclusions can be avoided.
Stages of bite formation
The first stage is completed by the time teeth erupt. Then it is formed:
- Temporary bite
Period: from 6 months to 3 years
. Teeth are actively growing, their relationship in the jaw is changing. When all the teeth have erupted, the stage of a formed temporary bite begins. It lasts until the moment when baby teeth begin to be replaced by permanent ones. The number of teeth is 20. Their location is influenced by the child’s habits: thumb sucking, sucking a corner of a bedspread, long-term use of a pacifier. Most causes of pathologies appear at this age.
- Replaceable (mixed)
Period: 6-14 years
. The active growth of permanent teeth increases the bite and promotes changes in the position of the jaw relative to each other. The jaws are in the process of formation. This is the ideal time for orthodontic treatment.
- Constant
Once all the baby teeth have fallen out, the bite becomes permanent. Number of teeth 28-32. With the appearance of fangs, the bite increases again.
The final formation of the jaws is completed by the age of 21, but the movement of teeth continues throughout life. The teeth are worn down by the friction of the side parts, because of this their position in the jaw changes, although we do not notice it. Dentists call this process mesial movement.
How does bite development occur?
The bite develops along with the teeth, so it is very important to monitor the condition of the child’s baby teeth, since already at this stage, under a number of prerequisites, formation disorders may appear. The position of the tongue also affects the bite; if the position is incorrect, distortions in the rotation and inclination of the teeth are possible.
There are five main life stages during which the formation of a normal bite occurs:
- In the first six months of a newborn’s life, the foundations are laid for the correct closure of the dentition, if a natural method of feeding is used: chewing muscles, the activity of the lower jaw arch increases, the foundations for the correct development of the oral cavity are laid, the position of the tongue is focused on the lips and cheeks.
- At six months, the child begins to cut his first milk teeth with thin roots and a roller-shaped crown, which are absorbed by the time the permanent teeth emerge. The tongue rests on the roof of the mouth.
- By the age of three, temporary teeth have been formed, ensuring the full functioning of the dental arches, allowing chewing food and speaking. From the age of four, the primary bite gradually begins to fade - the protruding parts of the teeth are worn away, the incisal overlap becomes smaller.
- At the age of six, the replacement of teeth from milk to permanent ones begins. The overlap of the bottom row is normally no more than one third. If during the formation of baby teeth or after their loss, gaps have formed between the teeth, called tremata and diastemas, at this stage they disappear.
- By the age of fifteen, a teenager completes the full formation of dental arches. The norm is full contact of both dentitions when chewing, excluding the first lower incisors and wisdom teeth that appear later.
Malocclusion problems later in life are most often due to developmental errors at one of these five stages. For example, some children can jokingly push their lower jaw forward - this seemingly harmless movement can affect the distortion of the bite. An experienced dentist is able to help stop incorrect actions at an early stage and teach the child the correct position of the jaw, to facilitate learning - in the same playful way.
Parental attentiveness also plays an important role. After the first six months of a baby's life, when the child's first teeth begin to cut, it is imperative to eliminate prolonged use of a pacifier and prohibit the child from keeping a finger in his mouth. Otherwise, these actions will lead to the appearance of a so-called open bite.
What does a correct teeth bite look like?
Physiological (correct) occlusion in humans is characterized by:
- adequate form of dentition. The top one looks like a semi-ellipse, the bottom one resembles a parabola;
- the upper incisors overlap the lower ones by ⅓ of the height;
- there is contact between all teeth;
- the lower teeth are vertical, the upper teeth are inclined;
- each tooth, except 4, has 2 antagonists (one opposite);
- the correct bite in the diagram is marked by the symmetry of the incisors;
- chewing teeth are in contact with each other.
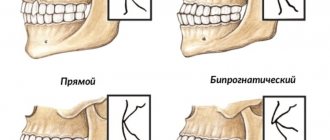
Correct bite in adults has its own variations. All of them are considered a variant of the norm:
- Orthognathic
. The upper teeth slightly overlap the lower teeth, and all molars and premolars occlude. - Straight
. The upper teeth do not overlap the lower ones, but join with them. The lateral teeth meet well. - Physiological progeny
. The lower teeth protrude beyond the upper teeth, but contact is maintained. The lateral teeth close together without gaps. - Biprognathic
. The incisors of both jaws are inclined forward, with intact contact.
When the construction of teeth is considered incorrect
The main signs of malocclusion:
- Complete or partial absence of tooth contact during occlusion.
- Impaired chewing of food.
- Sound pronunciation defects.
- Changes in the shape of the face due to jaw deformations.
Pathological types of bites
Pathological occlusion is diagnosed if there are structural deviations from normal anatomy in the structure of the dentofacial apparatus, and disturbances in the functioning of the masticatory muscles and the temporomandibular joint are also detected.
Mesial
A distinctive feature of this type of abnormal bite is the advancement of the lower dentition in relation to the upper one.
Patients with mesial occlusion have a characteristic appearance - a massive protruding chin, a receding upper lip, and a concave facial profile. There are chewing disorders and speech defects.
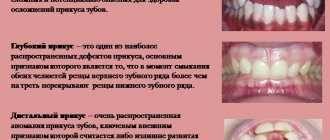
Deep
With a deep bite, the upper incisors cover more than 50% of the lower incisors. In some cases, the upper incisors, when closing the teeth, reach the gums of the lower jaw and injure them.
Although orthognathic, biprognathic, and straight bites are normal, these types of bites can cause the following problems: damage to the enamel, chipped crowns, and injuries to the soft tissues of the oral cavity.
Open
The main sign of pathology is the presence of a vertical gap between the dentition in the area of the frontal or chewing teeth.
An open bite is often formed against the background of narrowing of the alveolar arches, which is why the teeth have an irregular shape and are crowded.
Symptoms: lengthening of the lower third of the face, slightly open mouth, hypertonicity of the facial muscles, impaired diction, difficulty breathing, inadequate chewing of food.
Cross
Due to the displacement of the lower jaw to one side, the dentitions close like scissors crosswise, and underdevelopment of the jaw on one side is noted. Facial asymmetry is pronounced.
Distal
This is a variant of a pathological bite, in which the lower dentition moves back in relation to the upper one. In this case, the frontal (front) group of teeth does not connect, and the chewing teeth contact incorrectly, which creates the preconditions for blocking the normal development and growth of the lower jaw.
Facial signs of distal bite:
- protrusion of the upper jaw;
- shortening of the upper lip and lengthening of the lower lip;
- sloping chin.
Dystopia
A type of abnormal bite when the teeth on the upper or lower jaw are located outside the dentition and not in their place. In addition, with dystopia, the teeth are often turned around an axis.
Other types of occlusion in dentistry
There are 3 large groups of bites.
- Normal
(physiological). These bites have several variations, but the teeth are closed, the jaws are in the correct position, and the teeth are symmetrical along the incisors. - Anomalous
. Congenital defects caused by harmful effects on the fetus during pregnancy or genetic disorders - Pathological
. Defects acquired after teething as a result of disease, missing units, or displacement of teeth.
In life, the last two concepts are often mixed and replace each other. Based on the relationship between teeth and jaws, the following types of bite are distinguished:
Deep
The upper teeth cover the upper ones by more than ⅓. The contact between the teeth is broken. This leads to impaired chewing function, abnormal enlargement of the upper jaw, and disruption of the anatomical structure of the face. The second name for this defect is traumatic. As a result of pathology, the functioning of the temporomandibular joint is often disrupted, the mucous membranes are injured, and the enamel is pathologically erased. This is the most common pathology.
Open
The teeth do not close completely. The defect can be frontal or lateral. This pathology is characterized by impaired diction, chewing, and swallowing. Mouth breathing is observed, hence drying out of the mucous membrane and frequent caries.
Distal
With this defect, the upper jaw is strongly pushed forward. The front teeth do not occlude, and the occlusion of the rear teeth is broken. Characterized by problems with breathing, chewing, and swallowing. Patients complain of joint pain, frequent caries, and periodontal disease.
Mesial
When the lower jaw is pushed forward, they speak of progeny or mesial occlusion. This jaw bite pathology is accompanied by diastemas (large gaps between the front teeth) or trema (gaps between any teeth). Often patients have crooked lower teeth, they are crowded, and there is increased deposit of tartar.
Crossbite
Some units overlap each other. Difficult to treat, surgical intervention is often used. It is characterized by facial deformation, speech defects, disruption of chewing function and the functioning of the TMJ. Patients complain of constant biting of the cheeks and tongue.
All pathological forms of bites in orthodontics are recommended for correction with removable (for baby teeth) and non-removable structures (braces), and aligners.
Distal occlusion (upper macrognathia, prognathia)
Distal bite therapy can be carried out using the following methods and methods:
- orthodontic treatment,
- hardware-surgical,
- surgical,
- prosthetic
- various combined and combined methods.
During treatment, taking into account certain features depending on the clinical form of the anomaly, the age of the patient, the individual characteristics of the structure of the facial skull and the type of its growth, the following tasks must be solved.
- Regulation during jaw growth using a facebow and extraoral traction or a functional apparatus.
- Restriction of growth and shortening of the dentition of the upper jaw due to the distal movement of the upper molars, canines and elimination of protrusion of the anterior teeth
- When treating distal occlusion, it is advisable to transfer form P2 to form II1, which can be achieved by using arches in the traditional sequence, that is, the primary arch, as a rule, is multi-stranded, flexible, allowing the creation of additional bends when teeth are crowded in order to avoid excessive load on them, then a steel one rectangular.
- Distal movement of the upper anterior teeth without or after extraction of individual teeth (most often premolars).
- Stimulation of growth and anterior movement of the lower jaw
- Expansion of the dentition of the upper and/or lower jaw
- Change in interalveolar height and normalization of the Spee curve.
- Normalization of the function of masticatory and facial muscles
- Retention period
It is not always possible to completely correct the anomaly during these manipulations, but a change in position of approximately 45 mm can be achieved. When planning orthodontic treatment of patients with distal occlusion, teleradiological examination data characterizing the type of growth of the maxillofacial complex, the activity of residual growth and their comparison with orthognathic occlusion are very important.
With a distal occlusion, the proportion of the neutral type of growth decreases (from 71% with orthognathic to 50%) in favor of horizontal, namely to 43% versus 15% with orthognathic. This indicates the predominance of development of the facial skeleton in the anteroposterior direction due to intensive growth of the upper jaw, especially in the period of 7-12 years and somewhat less in 12-15 years. That is why the most optimal for modifying jaw growth are the replacement bite and the earliest permanent bite (for 14-15 years, for 12-13).
In patients with a neutral type of growth of the facial skeleton, the main tasks when correcting a distal bite are, first of all, to restrain the growth of the upper jaw and stimulate the growth of the lower jaw. In such patients, mainly removable equipment of functional or combined action should be used.
With the horizontal type, it is necessary, first of all, to restrain the growth of the upper jaw, with simultaneous distal movement of the lateral teeth, using a face bow with a cervical traction. For adult patients, to reduce the upper dentition, treatment is recommended with the removal of the first premolars, followed by distal displacement of the lateral and anterior teeth. This is indicated for prognathia with a reduced or average size of the base of the upper jaw and for prognathia caused by crowding of the upper front teeth, their sharp protrusion, often together with the alveolar process.
In severe forms of distal occlusion with a pronounced horizontal gap, removal of the first premolars is indicated even in a mixed dentition. After this, when treating II1, you can use a flex arch, then a nitinol one, fixing them first on the teeth of the upper jaw. One of the indications for tooth extraction is a reduction in the retromolar space, which enhances the mesial displacement of the lateral teeth and aggravates the close position of the anterior teeth, with insufficient space for the canines of the upper and lower jaw (Zhulev E.N.).
According to WR Proffit (1986), the indication for serial extraction is a discrepancy between the size of the teeth and the dental arch by 10 mm or more, and Ringenberg (1964) believes that the initial value should be smaller, namely 7 mm. According to the point of view of V.P. Norkunaite, with the length of the segment of the dentition “from the distal surfaces of the crowns of the 12th and 22nd teeth to the mesial points of the sixth teeth” equal to 18.5-21.0 mm, and if the sum of the mesiodistal dimensions of the canines and premolars is 22.5-24, 0 mm, then removal of individual permanent teeth is indicated. It should be noted that non-extraction orthodontic treatment is even relatively simpler, since there is no need to move the teeth a significant distance to close the post-extraction gap.
As a last resort, removal of the second molar (sometimes unilateral) is used and distalization of the dentition is performed using a face bow. It is very difficult to move the first molars distally more than 1.5-2.0 mm even after removing the second molars, since distal tooth displacement is much more difficult than mesial displacement. The latter requires more reliable support and stabilization, as E. Engle wrote about. The extraoral thrust should not be low, otherwise extrusion of the molars will occur.
During the period of replacement teeth, when treating distal deep bite, you can use the forgotten but good method of A. Katz, namely, crowns with spikes on the second milk or first permanent molars (the tooth is not prepared) of the lower jaw. When the mandible is advanced forward, the elongated mesial cusps of the artificial crown should fit into the gap between the first and second primary molars of the upper jaw, widened by preparation. In this case, some separation of the bite occurs, which contributes to the dentoalveolar lengthening of the lateral teeth and a decrease in the incisal overlap. Long-term use of such crowns (8-10 months) leads to the formation of an orthognathic bite.
In children with mixed dentition and a clear tendency to develop distal occlusion, McNamara recommends maxillary expansion with overcorrection, usually a rapid maxilla expander. The subsequent use of a retention plate leads to the movement of the lower jaw to a position more convenient for the patient, pushed forward. This eliminates buccal crossbite and, after some time, improves occlusal relationships in the sagittal direction. Somewhat earlier, this phenomenon was explained by H. Taatz and Reichenbach by the fact that the expansion of the upper jaw contributes to the spontaneous displacement of the lower jaw to the anterior position. If such correction does not occur, then RG Alexander recommends the use of a facebow with extraoral traction until the end of the mixed dentition.
In mixed dentition, removable plate devices and a pre-orthodontic trainer are used in the treatment of prognathia.
But in addition to this, when treating anomalies at the dentoalveolar level, especially when combined with a narrowing of the dentition or crowding of teeth, fixed structures can be used. First of all, this is a “2 x 4” device, that is, rings for the first molars and braces for the 4 upper incisors, or utility arches.
Growth can be stimulated using activators, for example Andresen Haüpl or function regulators R.Fränkel. The activator is a removable two-jaw monoblock plastic, functional apparatus, consisting of upper and lower plates connected to each other; a vestibular arch, springs or a screw may be added to them. In addition to the plates adjacent to the inner surface of the alveolar processes, they have a corresponding bed for the oral surfaces of all upper and lower teeth. It is better to fix all types of plates with arrow-shaped clasps and Adams clasps.
The device holds the lower jaw in an extended anterior position (a constructive bite that must be determined by the doctor before treatment), promoting dentoalveolar lengthening in the lateral areas, while the upper anterior teeth are moved posteriorly due to a reciprocal action. On the upper jaw, the plate touches the mesial edges of the surfaces of the teeth, but lags behind the distal ones. On the lower jaw, on the contrary, it fits tightly to the distal edges and lags behind the mesial ones to move the lower jaw.
The clinical laboratory stages of production are as follows.
First clinical impression taking from both jaws; the first laboratory casting of plaster models and making a wax template for the upper jaw with bite ridges to determine the constructive bite, the boundaries of the wax template: in front are the cutting edges of the incisors, behind is a line passing through the middle of the crowns of the last molars, on the side is the chewing surface of the lateral teeth.
The second clinical stage is the determination of a constructive bite: the patient moves the lower jaw forward to a neutral relationship of the first permanent molars (1 class each), and he is asked to close his teeth until they come into contact with the wax. In this case, the separation of the dentition should exceed the “rest height” and it is necessary to monitor the position of the ridge and the coincidence of the midline. If in the position of the constructive bite the neutral closure of the sixth teeth is not achieved and the discrepancy is 45 mm, then this position is fixed. If the sagittal discrepancy exceeds 6 mm, the first activator is first prepared (at 45 mm), and after 6-8 months the second activator is prepared, but with the movement of the lower jaw to the neutral closure of the sixth teeth.
After fixing the constructive bite, plaster models with a wax template are handed over to the dental technician and the doctor gives him instructions:
- make an apparatus with or without a vestibular arch for retrusion of the upper anterior teeth (the shape is being specified),
- install a screw or other additional elements, springs, levers, lingual arches, etc. F.Ya. Khoroshilkina and WR Proffit proposed installing facebow tubes into the activator (bite blocks in the premolar area) in order to be able, along with the functional action of the device, to create additional distal and vertical force using extraoral traction.
Second laboratory stage: the models are plastered in an occluder, the wax template is removed, a plastic base is made, the listed parts or others (as directed by the doctor), the device is polymerized in a special double cuvette or in a regular one, increasing its vertical size
Third clinical stage: fitting the activator in the oral cavity, first to the upper dentition, and then to the lower one; the activator should fit tightly to the teeth, with lips closed; The rules for using and caring for the device are explained to the patient and the next visit is scheduled. During repeated visits, the device is adjusted in the direction of movement of the upper and lower lateral teeth. During the treatment process, the dental bed is polished according to the direction of movement of the teeth, that is, those that need to be moved in the palatal or lingual direction, and vice versa, the plate should fit tightly to those teeth that need to be moved in the vestibular direction. The device can mainly be used while at home or while sleeping. Treatment is especially successful in the early stages of distal and deep bites.
The device helps restore nasal breathing, since the child is forced to breathe more through the nose due to the closure of the oral fissure by the plate. But it is contraindicated if nasal breathing is completely absent. The activator also helps eliminate the habit of sucking fingers, tongue, lips and various objects. The vestibular deviation of the lower teeth can be prevented by the activator hood, which overlaps them by 1/3 of the height of the crowns, so the plastic in it is polished or the hood is completely removed. Similar actions, depending on the progress of treatment, are taken at each visit. You can also stimulate the advancement of the lower jaw using the Balters bionator.
Treatment of distal occlusion (II2) can be carried out in two stages. First, the upper anterior teeth are deviated, eliminating the blocking of the lower jaw, that is, subclass II2 is transferred to II1 using edgewise therapy, rotating the first molar. The latter should be the first step in the treatment of a class II anomaly if there is a tendency for mesial rotation of the molar around the palatal root. If orthodontic treatment II1 is carried out without tooth extraction, then sometimes it is enough to turn the first upper molar with its buccal surface posteriorly, which allows you to create an additional space of 1.5-3.0-4.0 mm and the subclass will move to II1. This can be done with the help of an extraoral yaga, the Gozhgarin palatal clasp, in which the ends of the clasp, curved in two planes, are fixed into the palatal locks on the molars. The device is activated by unbending the loop.
This treatment method can be used when a class II anomaly is combined with an open bite. To illustrate, we give an example from the clinical practice of Dr. P. Ngan et al.: an 8-year-old patient had closure of the molars on both sides according to E. Engle class II, a 5-millimeter sagittal discrepancy in the frontal area, an anterior open bite and lower retrognathia. The main goal of treatment was to delay the anterior growth of the upper jaw, transfer the molar relationship from class II to class I, reduce concomitant skeletal disorders and open bite.
The treatment apparatus consisted of an activator and an extraoral arch attached to it. Because the base plate of the device did not cover the vault of the palate, a connecting arch (diameter 1.2 mm) was used instead, which increased the space for the tongue. For fixation to the extraoral traction activator, a special tube with a diameter of 1.12 mm (0.045 inches) was mounted in the plastic between the upper and lower dentition. The force of extraoral traction was up to 400 grams on each side. Springs for tilting the front teeth were made of elastic steel wire with a diameter of 0.5-0.6 mm, the lower part of which was fixed with horizontal shanks in plastic. The vertical part of the springs had a point contact in the area of the necks of the teeth.
The mandibular part of the apparatus consisted of an incisal platform for advancing the lower jaw. When determining the constructive bite, the lower jaw moved forward until the incisors made direct contact. In patients with hyperactivity of the muscles of the perioral region, to reduce their effect, lip pads in the form of a “tear” according to R. Fränkel were used, which were located in the vestibule of the oral cavity parallel to the alveolar process. The ratio of molars according to class I. was achieved in about a year and at the same time the size of the open bite decreased, which led to an improvement in the lip relationship. The entire treatment lasted about 14 months.
Sometimes symmetrical or unilateral removal of premolars in the upper jaw is performed. At the second stage of treatment, the lower jaw is set in the correct relationship with the upper jaw. To do this, when there is a sharp narrowing of the lower dentition, it is expanded, and then, based on the clinical picture and X-ray data of the temporomandibular joints, sagittal movement of the lower jaw is carried out using plates with an inclined plane. There are a large number of varieties of plates, including those with an inclined plane. Depending on a particular clinical situation, the doctor selects the appropriate design.
A. Katz's bite block is used to treat prognathia in combination with a deep bite. A special feature of its design is an inclined plane and reversible clasps that bend over the cutting edges of the front teeth onto their vestibular surface. The plate does not adhere to the mucous membrane of the anterior part of the palate and the necks of the anterior teeth. When closing with an inclined plane, the lower teeth slide along its surface, trying to return from a forced (constructive) bite to its original position, and the lower jaw moves forward, and the upper teeth tilt towards the palatine side. In the lateral areas, due to the separation of the bite, a vertical restructuring occurs, that is, dentoalveolar elongation.
The fundamental clinical and laboratory stages of making a plate differ little from those described in the manufacture of the activator: obtaining impressions, making a wax composition of the plate with retaining and reversible clasps, determining the constructive bite, polymerization of plastic, fitting and application of the device.
It should be remembered that when treating distal occlusion in patients 15-20 years old, when using bite blocks before stabilization occurs, a double or “wandering” bite may be established, that is, in a position of physiological rest, the lower jaw is fixed in a neutral position, and during function it moves to the former (distal).
The devices proposed by R. Fränkel are called functional regulators, the main parts of which are side shields and pelota, which relieve the dentition from the pressure of the cheeks and lips. As a result, under the influence of the tongue, the growth of the apical base is stimulated in the transversal and sagittal directions. The parts of the apparatus are held together by metal arcs made of elastic wire. This skeletonization made it possible to increase the strength of the regulators, reduce the size of the plastic shields, lighten the apparatus and make it open in the frontal area for better swallowing and speech. Active elements (screws or springs) can be added to the device to accelerate the movement of individual teeth.
R. Fränkel proposed function regulators of three main types: type I (FR I) is used to eliminate protrusion of the anterior teeth and distal occlusion, combined with narrowing of the dentition, fan-shaped arrangement of the upper frontal teeth and with anomalies of 1 class. E. Engla; type II (FR II) for the treatment of distal occlusion of subclass 2 (II2), that is, in combination with deep overlap and retrusion of the upper anterior teeth; type III (FR III) for the treatment of progenia. The principal clinical and laboratory stages of the regulators have been described previously.
The use of this method is effective in early childhood (the period of primary and mixed dentition), that is, when one can count on the growth of the jaw bones and especially the apical base. Treatment with the regulator, especially during the period of its development, is recommended according to the following scheme: for the first two weeks use the device during the day for 1 hour, for the next 2 weeks every day for 2 hours, then during all free time, removing the device only during meals; in 2-3 months around the clock. After correcting the bite with adjusters, retention devices are not required, since already during the active phase of orthodontic treatment, the conditions that contribute to the occurrence of relapse are eliminated.
Sagittal movement of the lower jaw during prognathism should be considered as the last stage of treatment, based on the considerations that the restructuring of muscles, temporomandibular joints, as well as dentoalveolar lengthening in the lateral areas in the vertical direction are not always successful. When treating severe forms of prognathia with deep overlap, the separation between the lateral teeth should be at least 45 mm. With active protraction of the lower jaw, tissue restructuring occurs in the order of activation (stimulation) of functional hypertrophy, mainly of the lateral pterygoid muscle, which is poorly developed during prognathism.
It is necessary to constantly monitor the separation of the bite and, as contact between the lateral teeth is achieved, to re-create the separation of the bite by correcting the inclined plane. It is also necessary to correct the appliance in the area where its base adheres to the palatal surfaces of the anterior teeth. In most cases, a sagittally moved mandible is secured in its new position due to the close contacts of natural teeth or contacts created by dentures.
The use of devices can be combined with active myogymnastics, but they are incompatible with edgewise therapy, although it would be very desirable to correct the dentoalveolar components of the anomaly simultaneously with the correction of jaw growth. This is possible when using non-removable functional devices or when combining braces with a face bow. There is no point in drawing a sharp boundary between the phases of treatment, expecting, for example, leveling of the dentition, because extraoral appliances also contribute to a certain extent to the correction of the dental components of the anomaly.
RG Alexander is a proponent of the use of extraoral traction both for growing jaws (children, adolescents) and for adults. But in the first, with the help of a facial arch, the growth of the upper jaw is suppressed and at the same time its dentition is leveled, the lower jaw is unblocked, providing the opportunity to achieve its genetic potential. In adults, when growth has stopped, the main purpose of extraoral appliances is to hold the upper molars in place, to avoid their displacement forward.
Intermaxillary traction, in the author's opinion, should be used while the dentition of both jaws is aligned and stabilized, rigid end steel archwires are installed (0.17 x 0.25) and torque control is established to prevent incisor tilting. The arches must completely fill the slots of the braces and be in the mouth for at least a month before installing elastic traction according to class II. Having studied the vector of forces in the traditional position of the above-mentioned thrust, that is, from the upper canines to the lower first molars, RG Alexander determined the presence of an undesirable, very significant vertical component of the force. An increase in the horizontal component of the force can be achieved through a different fixation of the traction, namely, from the second lower molar to the spherical hook of the bracket on the upper lateral incisors. This increases the vector of horizontally acting force and reduces the tendency to “open” the bite, for which, by the way, elastics are not used in the “Vari Simplex Discipline” system.
When treating the first subclass (II1) of prognathia, complicated by a deep or open bite, the incorrect position of the teeth and an anomaly in the shape of the dentition are usually eliminated. If it is necessary to expand the lateral areas of the upper dentition, then a rapid palatal expander (rapid maxilla expander) is used in the early stages of treatment, before the installation of fixed appliances. If the teeth have not erupted, then plastic plates with a screw can be used, and only then the lower jaw is moved forward. When treating a distal bite in combination with protrusion of the upper anterior teeth, their close position and narrowing of the dentition or their asymmetry, one should not rush to eliminate the protrusion, since the upper anterior teeth, which have become palatally inclined as a result of treatment, will interfere with the movement of the lower jaw.
According to many clinicians, with early treatment, distal occlusion can be eliminated in approximately 80% of patients with functional devices. The use of edgewise therapy, in particular the direct arch technique, expands the age-related indications for orthodontic correction, but positive dynamics of treatment are observed only at the dentoalveolar level.
In case of distal occlusion (II2), the method of eliminating crowding of teeth must be planned taking into account the structure of the facial skeleton, the age of the patient and the amount of space in the dentition. The correct choice of method allows you to get an optimal result and avoid complications during and after treatment.
Treatment of adult patients is reduced mainly to leveling the position of the teeth and eliminating deep incisal overlap, if any. The process of “detailing” the molars is either prolonged (as a result of the “distalization” of first the second and then the first molars) or is impossible because adults already have erupted second and third molars. In such patients, extraction is more indicated, and a dilemma arises: which tooth should be removed, the first or second premolar? To resolve this issue it is necessary to take into account:
- the magnitude of the space deficit; if, after straightening the teeth, a residual gap of no more than 2.0 mm is predicted, then the first premolar is removed, and if it is more than 2.0 mm, then the second premolar; this choice can be argued by the fact that during the closure of the spaces between the teeth, the tendency for retrusion of the incisors increases, while the removal of the second premolar has a lesser effect on the position of the incisors;
- dental condition, it is preferable to remove the affected teeth (destroyed crown, endodontic treatment, changes in periapical tissues, large filling or severe abrasion);
- after extraction, it is necessary to retract the canines or “first premolar canines”, for which the full arch technique or the segmental arch technique can be used;
- The full-arch technique in its standard implementation is as follows: at the first stage, braces are fixed on all teeth, using for additional support, for example, a Gozhgarin clasp, when indicated in combination with a face bow; the initial arch, as a rule, is nitinol, with simultaneous “distalization” of the canine or first molar using an eight-shaped ligature (within the dentition this can be done using springs, elastic traction, elastomeric power modules); it should, however, be noted that in this case, a protrusive displacement of the incisors occurs, which is very undesirable in adults, since then it is necessary to retract them to eliminate the sagittal discrepancy, therefore it is better to use the segmental arch technique;
- segmental arch technique: braces are fixed only on the teeth of the lateral segment, with additional stabilization of the supporting teeth, as in the previous version; then a steel edge arch with a diameter of 0.40×0.55 mm is passively inserted into the braces; for “distalization” the usual sliding technique; if the canine has an abnormal position initially, then a nitinol arch should first be introduced, fixing it only in braces on the canines and premolars, with simultaneous “distalization” with an 8-shaped ligature; after normalizing the position of the fang, you can move on to a full arch and fixation of braces on the incisors, the leveling of which is carried out according to the traditional method (nitinol arch, steel arches, TMA); This technique allows for canine retraction without side effects on the incisors.
For surgical treatment, write down clear indications:
- justification for the need for such therapy, for example, the magnitude of the sagittal discrepancy of the jaws is 10 mm or more, the angle of the SNSs (SNA) on the teleroentgenogram is greater than normal, which is ~ 82°
- good state of somatic and mental health, the growth of the patient’s facial skeleton must be complete
- pronounced protrusion of the lower incisors (the angle of inclination is less than 70-80°, while the norm is 90-95°); it is well known that the vestibular movement of the lower anterior teeth is very limited and the limit depends on the value of the initial axial angle; the maximum reasonable limit should not be less than 90-95°, therefore, when using equipment for the vestibular movement of the lower front teeth, you need to be very careful; correction of the sagittal position of the lower anterior teeth can be carried out: by changing their vestibular inclination,
- changes in the length of the lower jaw, but this depends on the age and nature of micrognathia, that is, it is of the condylar type (when the articular process, which is the center of longitudinal growth, is affected) or extracondylar,
- changes in the position of the mandibular head, if the anomaly has developed due to distal displacement of the mandible
An approximate set of myogymnastic exercises for the treatment of distal occlusion. Exercises should be selected according to the child’s age and not be too difficult. L.S. Persia recommends first of all determining the level of development of the child and giving the load not to the point of fatigue, but approximately 75% of it. Exercises to correct a specific anomaly should be dosed and performed against the background of general physical exercise, starting 2-3 weeks before orthodontic treatment.
Muscle contractions must be performed with maximum amplitude, their intensity must be within physiological limits, with a gradual increase in speed and duration; between two successive contractions there should be a pause equal to the duration of the contraction itself.
Exercises to normalize breathing function (performed during morning exercises, physical education lessons or while walking); starting position: the state of correct posture: the head and torso are held straight, the shoulders are slightly pulled back and slightly lowered, the chest is turned out, the shoulder blades are adjacent to the back, the stomach is tucked and the knee joints are straightened.
Exercises to normalize lip closure (can be performed during speech development classes). Starting position: sitting in front of a mirror, head held straight, shoulders slightly pulled back and slightly lowered, chest turned out, knee joints bent, legs together, stomach tucked.
Determination of dental occlusion
Often problems with bite are obvious, but it also happens that everything looks normal on the outside, but there is a problem. Therefore, it is better to entrust the determination of the bite to the dentist. They use special methods to determine correct or incorrect bite and prescribe treatment.
Diagnostics include:
- Clinical examination
The orthodontist collects anamnesis, conducts a general examination and examines the oral cavity and nasopharynx. They examine breathing, speech formation, swallowing, chewing, biting.
- X-ray examination
A panoramic X-ray or CT scan allows you to identify skeletal abnormalities, see the exact location of the teeth, the condition of the roots, and bone tissue.
- Biometric test
The doctor examines the jaws, takes and records all measurements.
- Functional test
Examination in a stationary position, while talking, opening the mouth in the lateral and frontal projection.
It is impossible to put the jaw back in place on your own, but the sooner the intervention begins, the better the result. It is very difficult to restore the correct position of teeth after 25 years; it is better to do this while the bite is forming.
Causes of malocclusion
The formation of a bite is a complex and lengthy process that begins at the stage of intrauterine development and ends only when a person reaches puberty.
- Genetic factor. One of the leading reasons for the formation of malocclusion is heredity, which determines the size and shape of the teeth, the width and length of the dentition, the height of the hard palate, as well as the nature of the location of the teeth (sparse or crowded).
- Quality of nutrition and maternal diseases during pregnancy.
- Birth injury. Jaw injuries received during childbirth lead to displacement of the temporomandibular joint, and subsequently to the formation of a pathological bite.
- Incorrect selection of nipples during artificial feeding, when the child does not make enough effort to obtain milk, as when sucking at the breast, which causes underdevelopment of the lower jaw.
- Untimely introduction of solid foods into the diet during teething. In the absence of chewing, the muscles of the dentofacial apparatus, on which the development of the jaws largely depends, are not strengthened.
- Behavioral factors: sucking pacifier, upper lip, fingers; sleep with the head thrown back.
- Irregularities in the timing and sequence of teething.
- ENT pathologies due to which the child is forced to breathe through the mouth for a long time: chronic rhinitis, sinusitis, deviated nasal septum, adenoids.
- Diseases affecting bone growth and development.
All these factors can cause improper closure of the dentition and form a pathological bite.
Consequences
The influence of bite on the condition of the dental system and the entire body is enormous.
Bite pathologies lead to:
- Loss of teeth. Uneven chewing load leads to cracks and chips. Bacteria penetrate through the damaged enamel layer, affecting periodontal tissue. Periodontitis develops. Teeth become loose and fall out. The risk of caries in such cases is higher than in people without defects.
- Disorders of the temporomandibular joint (TMJ). It begins to click, hurt, and in severe cases, dislocation is possible.
- Due to crowded teeth, plaque and tartar quickly form, which provokes gingivitis and periodontitis.
- Insufficient contact between teeth leads to food being poorly chewed. As a result, problems arise with the gastrointestinal tract.
- Oral, impaired breathing causes diseases of the respiratory system.
- The position of the jaws affects posture. An abnormal movement of the jaw forward shifts the center of gravity, the position of the neck changes, the chest collapses, and the person begins to stoop. Muscle tone is impaired and back pain begins.
- An incorrect bite distorts facial features and disrupts its symmetry.
Anomalies of the jaws affect the psychological state. The person withdraws into himself and avoids company. Depressive states are common.
Orthodontic treatment restores physical and emotional balance and helps improve self-esteem.