Before the invention of anesthesia, about 70% of operations ended in the death of the patient; patient survival depended only on the speed of the surgeon’s work. In 1839, the French surgeon Velpeau stated that “the elimination of pain during operations is a chimera that cannot even be thought about; cutting instrument and pain are two concepts inseparable from each other in the mind of the patient.”
On March 30, 1842, the American doctor Crawford Long first gave a patient to breathe ether before surgery. He published his results only in 1849, and on October 16, 1846, a test of ether anesthesia took place in the USA.
In Russia, the first operation using ether anesthesia was performed by a doctor, doctor of medicine, surgeon Fyodor Inozemtsev . The operation took place on February 7, 1847 on the territory of the First City Hospital in Riga. , Nikolai Pirogov also used ether anesthesia .
Anesthesia today
Today there are three main types of anesthesia - local, general and spinal. For quick interventions and for children, inhalation anesthesia is used - the child inhales an anesthetic inhalation mixture through a mask and falls asleep. Intravenous anesthesia is used for long and difficult operations.
By the way
Epidural anesthesia does not work for 1 in 20 patients, and red-haired people need 20% more anesthetics to stop their pain. In traumatology, regional anesthesia is used - a local anesthetic is injected into the area of the nerve, providing complete anesthesia of the limb. Epidural anesthesia is very popular for facilitating the labor process, since the patient can either remain conscious or doze off under the influence of drugs.
Spinal anesthesia is difficult to control and is rarely used, but the patient is completely switched off and does not feel pain. Anesthesia with preserved consciousness is used only in special cases, most often in neurosurgery, if it is necessary to maintain the patient’s consciousness and communicate with him during the operation. Oral (through the mouth) and rectal (through the anus, using an enema) anesthesia is practically not used today. The intramuscular method of pain relief is also becoming a thing of the past.
What are the types of fillings and fillings?
Many patients are asked: “What fillings do you want to get?” And in order not to get into an awkward position, you need to understand what kind of fillings exist.
Keep in mind! In dentistry, they differ in composition and use:
- Plastic and ceramic. Plastic ones are the most popular because they are considered cheap and quick to install. Ceramic ones are harder and more reliable.
- Amalgam fillings. They contain silver, copper, zinc, mercury or tin. They are considered ductile, have high strength and can last for several years.
- Temporary and permanent. Temporary ones are used for long-term treatment, and permanent ones are used for instant treatment at a time.
Note! Modern medicine provides several types of materials for tooth filling.
Their main goal is to restore all processes. The material must be selected for the appropriate load:
- Filling of front teeth. Most often, teeth are destroyed due to caries in the front row. This procedure has its own indicators. To avoid future problems with chewing food, a specialist installs light-curing material.
- Filling using paste. Doctors quite often use pastes in their work. They are needed to seal the void after the inflamed pulp has been removed.
- Innovative filling. Such methods include canal sterilization, the use of hot or cold gutta-percha, mummification and retrograde filling.
How to prepare for surgery
Before any operation, excluding emergency cases, careful preparation is carried out: doctors, the attending surgeon and an anesthesiologist assess the patient’s health, conduct an examination and prescribe tests, including a general blood test, a blood clotting test, a general urinalysis, and an ECG.
Based on all procedures, the doctor assesses the patient’s readiness for anesthesia. The operation is postponed if the patient has ARVI, high fever, or exacerbation of a concomitant disease.
Article on the topic
7 common myths about anesthesia The absence of complications after anesthesia is determined by several factors - the patient’s health condition and the work of the anesthesiologist. Therefore, before anesthesia, it is important to properly prepare for the operation and take into account all the nuances, in particular:
- Choose a medical institution as carefully as possible, because the risk of side effects from the use of anesthesia is lower, the higher the qualifications of the anesthesiologist.
- Tell your doctor about all the medications you are taking—drugs when combined can change their activity and duration of action. For example, taking regular aspirin affects blood clotting; sleeping pills and sedatives can change the body's reaction to the administration of painkillers.
- Tell your doctor about all concomitant diseases. A contraindication to anesthesia is any acute illness, exacerbation of a chronic disease, or even the onset of menstruation.
- Do not eat or drink (even water) 6 hours before anesthesia. In consultation with your doctor, you can take sedatives at night and in the morning to get enough sleep and not worry too much. It is also necessary to avoid alcohol consumption.
- It is recommended to eliminate cigarette smoking from your life 6 weeks before surgery - this will reduce the risk of respiratory complications after surgery. Under no circumstances should you smoke on the day of surgery.
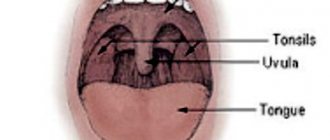
- Before the operation, it is necessary to remove all removable objects (dentures, piercings) from the oral cavity, as well as remove contact lenses and hearing aids.
- Remove nail polish from nails as it may interfere with the patient's breath analysis.
- Check with your doctor about what exactly you need to prepare for surgery. This usually concerns the preparation of the necessary clothing, personal hygiene products and items to fill the time free from treatment.
The doctor decides which type of anesthesia is right for you. Today, anesthesiologists use about a dozen drugs during surgery. Often, even for the same operation, but for different patients, different anesthesia is used. In emergency cases of anesthesia, the best type of “urgent” anesthesia is the one that the anesthesiologist uses daily and is the best at.
How to speed up the recovery process after removal of uterine fibroids
When a woman undergoes fibroid removal, recovery from even minimally invasive surgery can last up to 3 months. A number of procedures allow you to speed up this process, make it more comfortable and quickly return to your normal lifestyle; it is also important to follow the basic recommendations of a specialist. As a rule, the doctor voices them to each patient personally, but there are a number of universal tips:
- Wear a postoperative bandage: it provides the condition necessary to maintain the desired position of the internal organs, which helps prevent vaginal prolapse, etc.
- Observe contraception: pregnancy is not allowed for a year, but this period may last longer, depending on individual health indicators. It is optimal if contraceptive methods are selected by a doctor.
- Refuse thermal procedures: visiting a solarium, bathhouse, beach, seaside holidays, etc. is prohibited.
- Eat right: foods should be easy to digest. You should not eat fixing foods; you should give preference to soups, cereals, etc. After discharge from the hospital, you can add fruits, raw or baked vegetables, fish, and lean meat to your diet. It is recommended to completely avoid fatty, fried, viscous foods, carbohydrates, alcoholic beverages and coffee.
- Maintain a daily routine: it is worth including full sleep, daily walks, moderate physical activity (morning exercises, exercise therapy).
- Get rid of bad habits: smoking, stress, lack of sleep, etc. are prohibited.
And, of course, do not forget about regular examination by a doctor, even if there are no signs of complications.
Recovery after removal of uterine fibroids: methods
- Drug therapy.
Removal of fibroids does not leave its mark on the body. Depending on the patient’s condition, the doctor selects medications. Usually these are drugs that relieve pain, strengthen the immune system, help replenish blood loss, as well as drugs to prevent blood clots. To restore hormonal levels and as a means of preventing relapse, the doctor individually selects hormonal drugs. - Physiotherapy.
A number of procedures, for example, SMT, lymphatic drainage massage, ultrasound and magnetic therapy, improve blood circulation and accelerate tissue regeneration processes, help avoid problems associated with changes in hormonal levels, early menopause, and are a means of preventing adhesions, swelling of the lower extremities, urinary disorders, etc. - Physiotherapy.
Moderate physical activity under the supervision of a specialist can strengthen the immune system and restore muscle tone. The optimal sports are gymnastics and regular walks, but any water sports will have to be abandoned. Kegel exercises help relieve urinary incontinence. Breathing exercises help avoid adhesions and speed up recovery. - Psychotherapy.
Women often experience depression caused by infertility after surgery to remove uterine fibroids. Rehabilitation in this case is impossible without psychotherapy. The doctor helps restore your emotional state and overcome depression.
"Frivolous" anesthesia
Many people associate anesthesia exclusively with serious operations, when a person is euthanized and completely anesthetized. However, everyone experiences anesthesia during less significant interventions, for example, in the dentist's office.
Article on the topic
Dental anesthesia, or what you need to tell your dentist about And despite the fact that there are modern safe drugs for local anesthesia, carpule technology is used, when the medicine is already prepared and packaged in syringes at the factory, not everyone has dental anesthesia without complications.
The anesthetic risk group includes 30% of those who came for dental treatment. These are people with cardiovascular diseases, allergies, and endocrine pathologies. The condition of the liver and kidneys plays an important role - you need to tell your doctor about the presence of any of these diseases, or better yet, provide medical documents.
Also vulnerable are the elderly, pregnant women, children and those who are very afraid of dental treatment.
Is it possible to smoke after treatment and filling of a tooth? Recommendations for different cases
Smoking is a harmful habit that is quite difficult to get rid of. Cigarettes, and especially the substances they contain, have a negative effect on the body as a whole. The vessels narrow, the cells receive little oxygen and nutrients. But the first place nicotine encounters is the oral cavity. All substances begin to be absorbed into the mucous membrane and also affect the tooth enamel. You can harm yourself even more if you start smoking immediately after filling a tooth. Below we will look in more detail at whether it is possible to smoke after filling and dental treatment.
Is it possible not to wake up after anesthesia?
Many patients are afraid that they may not wake up after anesthesia. On the one hand, this is possible, but these cases are extremely rare. According to statistics, this happens in one out of two hundred thousand planned operations, but even then, most often death occurs not due to anesthesia, but in connection with surgical intervention.
But there are complications after anesthesia. For example, smokers are at high risk of developing bronchitis and pneumonia. After surgery, memory, attention and the ability to remember are often reduced, but this lasts from two weeks to several months. Some patients may experience nausea, dizziness, temporary memory loss, sore throat, hoarseness, but these sensations pass quickly and do not cause harm to the body.
What are the side effects of anesthesia?
After spinal or epidural anesthesia:
- numbness for several hours;
- difficulty urinating (the doctor may put a catheter on you, but after a few hours you will be able to urinate on your own);
- in rare cases, a headache may occur (it is called “spinal”), which lasts several days, is removed with painkillers and goes away on its own.
After general anesthesia:
- after waking up, you may feel a little “off” - as if not entirely sober or slightly disoriented;
- Nausea and vomiting may occur; your doctor will give you medicine to help relieve these symptoms;
- sore throat - if you have had a breathing tube inserted. It usually goes away quickly.
After certain conditions and surgeries, patients may experience breathing problems. Usually in these cases they are left on a ventilator for some time and sedated. Before the operation, the anesthesiologist will warn you about possible breathing problems in your case.