When is it necessary to remove an impacted tooth?
Despite millions of years of evolution, humans still continue to develop and improve. Our ancestors had massive jaws, and therefore they accommodated more teeth, which were adapted for biting and tearing food, as well as for chewing it. Now, due to changes in diet, the jaws have begun to shrink, and therefore sometimes there is simply not enough space for all the teeth. This is how impacted teeth appear, i.e. teeth, the rudiments of which formed in the jaw, but there was not enough space for them to erupt, and therefore they remained in the bone, never growing into the dentition.
Diagnostics
Diagnosis of dystopic teeth consists of examining the oral cavity, assessing the bite and obtaining x-ray data. To accurately determine the condition of teeth and jaws, use:
- Teleradiography - X-ray examination is carried out from a large focal length, which reduces the radiation dose to the patient and reduces distortions in the image. Teleradiography is needed not only for diagnostics, but also for predicting the results of treatment and monitoring its process.
- Computed tomography is a layer-by-layer study of tissue. The images are combined into a 3D image, which allows you to more accurately study the position of the tooth in the jaw and develop a treatment plan.
- Orthopantomography - provides a detailed image of the jaw and all teeth, allows you to evaluate the inclination of erupted and impacted teeth, and detect anomalies of tooth germs and hard tissues.
Impacted and dystopic teeth – is there a difference?
The standard assumption is that a person should have 32 teeth, but it is now common for people to have fewer teeth. The most common example is the absence of two or more eights in the dentition. At the same time, the computed tomogram shows that they are, in principle, there, but they are located deep in the jaw. There are other situations: individual units have partially grown, but not enough to be considered full-fledged teeth. Such teeth are called incompletely erupted or partially impacted.
In dental practice, there is another type of anomalies of eruption and position - dystopia. This is when the tooth has grown “to its full height”, but in the wrong direction - towards the brothers in front; to the right, towards the cheek, or to the left, towards the palate or tongue. In some cases, this state of affairs interferes with neighboring teeth and can cause various diseases in them, in others it harms the person himself, worsening the quality of chewing food, making it impossible to properly close the jaws, curving the entire dentition and causing pain.
In addition, incomplete eruption and dystopia are often combined with each other, and then the situation worsens so much that it leaves the dentist practically no choice - such an abnormal tooth must inevitably be removed.
Anomalies of teeth position
In case of anomalies in the position of the teeth, the task of the orthodontist is to preliminary normalize the shape and size of the dentition and occlusion. For this purpose, various orthodontic structures are used - both removable and non-removable. In the distal position, the teeth are moved mesially if there is space in the dentition. The need for mesial tooth movement arises when the first molar is removed (for therapeutic indications), and in this case the second molar moves mesially.
Since this anomaly relates to the lateral teeth, in devices of any design the fulcrum is formed in the anterior or lateral part of the corresponding side, and the point of application of force is the tooth being moved. If a rubber rod is used to move a tooth in an inclined distal position, the point of application of force is the coronal part of the tooth; in the case of a corpus tooth, it is the coronal and root parts, for which a rod with a hook is used in the area of the transitional fold.
In plate devices and mouth guard plastic structures, the fulcrum is hooks welded into the base. In metal structures, hooks are also soldered in the front section on the corresponding structural elements. Primary and permanent teeth at the appropriate stage of formation can be moved in the mesial direction using hand-shaped springs (according to Kalvelis). Permanent teeth in the final stage of root formation are moved using a brace system both obliquely-rotational and corpusally. To move lateral teeth in the mesial direction, the use of a positioner is ineffective.
Treatment of mesial position of teeth is carried out individually. With early removal of the second primary molar or primary edentia of the second premolar of the upper jaw, mesial movement of the first molar is observed. In this regard, the closure of one pair of antagonist teeth is disrupted, namely the mesial-buccal cusp of the first molar of the upper jaw is located in front of the intercuspal fissure of the first molar of the lower jaw. In this case, it is possible to maintain the mesial position of the first molar and then it is advisable to move the second molar forward.
If the doctor decides to move the first molar in the distal direction in order to achieve good closure with the antagonist teeth, you can use a plate on the upper jaw with a sectoral cut, a Kalamkarov apparatus, or an Angle arch. The use of a facebow with cervical traction is especially effective. For the first molars, rings with facebow tubes are made. On the side of the distally moved first molar, a bend is made on the arch, which rests against the tube, and on the opposite side, the end of the arch does not have a stop and is freely located in the tube. In the anterior section, the facial bow is separated from the front teeth. When applying a cervical traction, the entire force of the facebow is directed toward the first molar, which should be moved distally. To move both first molars distally, the facebow has stops in front of the tubes on both sides and both teeth will move distally.
After moving the first molars in the distal direction, the integrity of the dentition is restored at the level of the second premolar using only prosthetics or with preliminary implantation. In the clinic, the mesial position of the lateral teeth is often encountered. This may be due to early removal of the primary canine, high position of the permanent canine bud, the presence of a supernumerary tooth bud, macrodentia of the lateral teeth, a change in the order of eruption of the canine and second premolar (the second premolar erupts first). In this case, the type of closure of the lateral teeth corresponds to Angle class II. To create space for the canine, the lateral teeth must be moved distally. For this you can use plate devices.
Devices 1 and 2 allow you to move the lateral group of teeth on both sides in the distal direction. In this case, the front teeth are moved in the labial direction. Plate apparatus 3 (a plate for the upper jaw with a sectoral cut) moves the lateral teeth in the distal direction, and apparatus 4 allows, using a vestibular arch with an M-shaped bend, to move the canine in the same direction (the end of the arch is welded into the distal part of the cut). Apparatuses 5 and 7 move molars in the distal direction, and apparatus 6 moves one molar.
The main problem encountered when moving a canine distally is its initial position. The choice of orthodontic apparatus and the direction of the acting force depend on the position of the crown and root parts of the tooth.
Treatment of lateral position of teeth . The most typical clinical sign of such an anomaly is the appearance of a gap between the central incisors - diastema .
The following types of diastema are distinguished: 1) symmetrical diastema, in which there is a lateral displacement of the central incisors; 2) diastema with preferential movement of the crowns of the central teeth in the lateral direction from the midline. The roots of the central incisors retain their position or move slightly in the lateral direction; 3) diastema, in which the crowns of the central teeth have shifted slightly in the lateral direction from the midline, and the roots of the central incisors have shifted significantly; 4) asymmetrical diastema, which occurs when one central incisor has moved significantly in the lateral direction, while the other central incisor has maintained its normal position.
It should be noted that the lateral displacement of the central incisors can be combined with their rotation along the axis of the tooth (tortoanomaly) and vertical displacement of the teeth (dental alveolar lengthening or shortening).
Treatment depends on the clinical picture and causes of the anomaly. If there is a supernumerary tooth germ between the roots of the central incisors, it should be removed. In case of microdentia of the central incisors, the diastema is eliminated only by prosthetics of the central incisors with solid cast or metal-ceramic structures. Such prosthetics are performed in adolescents after 14-15 years of age. In case of diastema caused by microdentia of the lateral incisors, the diastema should be eliminated, and then prosthetics of the lateral incisors should be performed with artificial crowns.
If the upper jaw develops excessively in the anterior region and a diastema occurs, one should try to delay the growth of the upper jaw using a plate with a loop for the treatment of diastema and a vestibular arch. At the same time, the loop and U-shaped bends of the vestibular arch are activated. The canine is removed and installed in place of the missing lateral incisor or moved distally. In the first option, this can be done when the root of the canine is located significantly ahead of its proper place in case of normal eruption. If the mesiodistal size of the canine allows filling the gap formed behind the central incisor, then the cusp of the canine crown can be ground down and given the shape of a lateral incisor. Moving the canine mesially is only possible if the antagonist teeth allow the canine to create normal occlusion with them; otherwise, contact with antagonist teeth (regardless of retention) will result in lateral movement of the canine.
When distal movement of the canine occurs, the gap formed in the area of the missing lateral incisor is eliminated by prosthetics. To do this, you can make a metal-ceramic structure with support on the canine and select the central incisor as the second point of support by making a cusp located on the palatal surface
If the diastema has developed due to the low attachment of the frenulum of the upper lip, they resort to plastic surgery of the low-attached frenulum. Surgical treatment should begin after the eruption of not only the central incisors, but also the lateral ones, i.e. at the age of 8-9 years. There are cases when, after the eruption of the lateral incisors, the diastema disappears on its own.
If there is a diastema caused by bad habits, it is necessary to wean children from them, and hypnosis therapy is also effective.
With a diastema formed as a result of the abnormal position of the primordia of the incisors and canines, the eruption of not only the incisors, but also the canines is required, after which the diastema may self-remove.
Treatment of symmetrical diastema is carried out with orthodontic appliances, taking into account the size of the gap between the incisors. If the diastema is 3 mm or less, a plate on the upper jaw with a loop for treating diastema or with arm-shaped springs can be used. Activation of the loop is carried out 2 times a week by squeezing the loop with crampon tongs or pliers. You can also use a plate on the upper jaw with two arm-shaped springs covering the incisors from the lateral side, and hooks open to the rear, between which a rubber ring is placed. To prevent rotation of the incisors as they move toward the midline, bend the wire along the palatal surface of the incisors.
When a diastema is combined with deep incisal occlusion or disocclusion, it is necessary to make a bite pad on top of the loop. When treating more pronounced diastema, devices are used that would facilitate the body movement of the incisors and would prevent their rotation during movement. To do this, orthodontic crowns (rings) are used on the incisors with rods soldered to their vestibular surface with hooks open to the rear, between which a rubber ring is placed. To prevent rotation of the incisors when moving them, you can solder a horizontal tube to the ring of one of the teeth, and a wire to the other, one end of which will be soldered horizontally to the crown on the vestibular side, and the other should fit into the tube. Thus, the problem of rotation is removed and tension is created for the teeth to move.
When treating diastema with predominant movement of the crowns of the central incisors, the main load of the orthodontic apparatus should be in the area of the coronal part of the incisors. To do this, use a plate on the upper jaw with a loop for the treatment of diastema, arm-shaped springs with hooks open to the back, with a rubber rod placed between them. You can make orthodontic crowns or rings for the central incisors, solder vertically directed rods with hooks open to the rear to them, and put a rubber rod between them.
In case of diastema, when the crowns of the central incisors have shifted slightly in the lateral direction from the midline, and their roots are more significant, it is necessary to create conditions for a more significant movement of the root part of the teeth compared to their crown part. In these cases, a rotational moment is created between the crown and root parts of the tooth for the correct vertical position of the incisors, and only then the diastema is eliminated. For this purpose, crowns or rings are made for the central incisors, and rods are soldered vertically on the vestibular side. The upper end of the rod should be extended and end with a hook, open back at the level of 2 tooth roots or K from the top of the tooth root. Then a stable Angle arch is applied to the dentition, to which a hook open to the rear is soldered in the canine area on the opposite side of the dentition. When an oblique rubber rod is applied, the tooth root experiences a load in the mesial direction, but the tooth does not rotate, since there is no second rod in the opposite direction. To do this, the lower hook from the bar is open forward, from it a rubber rod will go to the hook, open back, which is soldered to the Angle arch in the canine area on the same side of the dentition.
Instead of an arch, a plate on the upper jaw with Adams clasps on the first molars and button clasps located between the first and second premolar on both sides of the dentition can be used as a support. The ideal technique to correct this anomaly is braces.
When treating an asymmetrical diastema, which occurs when one central incisor is displaced laterally, only this tooth should be treated. The choice of orthodontic technique depends on the position of the central incisor, which can be different: parallel with an offset from the midline, when the root and crown of the tooth are displaced the same distance from the midline; the crown of the tooth is displaced more significantly than its root, the root of the tooth - more significantly than its crown. Lateral displacement of the central incisor can be combined with its tortoanomaly, as well as with dentoalveolar lengthening or shortening. With this form of diastema, the central incisor, which is normally located, can serve as a fulcrum when moving the abnormal incisor. To eliminate an asymmetrical diastema, a plate can be made for the upper jaw with a hand-shaped spring covering the moving incisor from the distal side. As a support, Adams clasps are used on the first molars, button clasps and a round clasp on the central incisor, located correctly. You can make an arm-shaped spring with hooks open back, and put a rubber rod between it and the second hook located on a round clasp and also open back.
For a more pronounced diastema, a crown or ring is made for the tooth being moved with a guide tube, as described above.
Very often, diastema is accompanied by protrusion of the upper front teeth. In this case, along with treatment of the diastema, the anterior portion of the upper dentition should be flattened. For this purpose, it is more correct to make a plate for the upper jaw with arm-shaped springs on 1|1 to correct the diastema and a vestibular blowout with U-shaped bends with a vinyl chloride coating.
In recent years, orthodontic devices - positioners - have been used to eliminate diastema in dental practice.
Treatment of vestibular position of teeth . Permanent teeth with formed roots are moved from the vestibular position with an Angle arch, and depending on the combination with anomalies in the size and shape of the dentition, both a stationary and a sliding arch are used. Since the bracket system is universal, it is intended to use its design features to normalize the position of permanent teeth in the vestibular position. At the appropriate stage of formation of the roots and periodontium of permanent teeth, it is possible to use a positioner.
Normalization of the position of the anterior teeth located vestibularly is carried out, as is the normalization of the position of the lateral teeth. However, the morphological, functional and topographical features of the anterior teeth determine the possibility of using devices of specific designs and different combinations of their structural elements. Thus, vestibular retracting arches are widely used in children with baby teeth and during their replacement period. Naturally, the design of the device is determined by a complex of clinical manifestations.
One of the features of normalization of labially located upper teeth is also the use of a face bow. It should be said that the use of positioners to eliminate the labial position of the anterior teeth is more effective than when moving other teeth.
Treatment of the vestibular (labial) position of the lower front teeth is carried out with a retracting arch with vinyl chloride coating in the presence of three and diastema between the teeth.
If there is protrusion of the lower front teeth and the absence of three and diastema between them, one should take the path of removing complete teeth (usually the first premolars). The choice of treatment method depends on the size of the teeth and the type of closure of the first molars and canines. The canine often occupies a vestibular position, which is called dystopia, and it is necessary to determine whether there is a place for it in the dentition. Canine dystopia can occur as a result of disturbances in the eruption of teeth and the sequence of their eruption. Thus, very often after the eruption of the first premolar of the upper jaw, the eruption of the second premolar, and not the canine, follows. In this regard, and taking into account the mesial position of the teeth when they erupt, the canine has no place in the dentition and it erupts either in the vestibular or oral direction.
Dystopia of the canine occurs with macrodentia of the upper front teeth, which take the place of the canine. It can also occur in the presence of supernumerary teeth, narrowing of the dentition, early removal of the primary canine (in this case, mesial displacement of the lateral teeth occurs). Clinically, the mesial shift of the lateral teeth can be determined by the closure of these teeth with the antagonist teeth. On this side of the dentition, the closure of the lateral teeth occurs according to Engle’s class II, and on the opposite side - according to class I.
In case of canine dystopia, it is necessary to find out whether there is a place for it in the dentition. If there is one, then there is only one task: to place the canine in the dentition. To do this, you can use a plate on the upper jaw with a vestibular arch and an M-shaped bend on the canine. When the M-shaped bend is activated (plastic is first cut out from under the canine on the palatal side), the canine experiences increased load and moves in the oral direction.
Teeth are moved from the vestibular position using a rubber rod and springs, arches, even screws. Moving with a screw involves placing it in activated form on a plate with a sectoral cut, which has clasps or a multi-link clasp on the moving teeth, as well as additional Adams or round support clasps on the opposite side. By activating the screw, i.e. returning it to its original position, the necessary movement of the teeth is achieved. When moving teeth using a rubber rod, a ring or crown with a hook, or a bracket is fixed on the tooth, which is the point of application of force, and the fulcrum is the hook in the base of the device.
If there is dystopia of the canine and there is no place for it in the dentition, a place should be created for it. If there is no space for a canine due to mesial displacement of the lateral teeth, they should be moved distally. Distal movement of teeth is possible in the absence of a wisdom tooth germ. For distal movement of teeth, a plate apparatus with a sectoral cut, a face bow, a Kalamkarov apparatus, and arm-shaped springs are used.
If there is a rudiment of a wisdom tooth, macrodentia of teeth, one should follow the path of removing a complete tooth in order to create a place for a canine. Most often, for orthodontic reasons, the first premolar is removed; in the presence of caries and destruction of the crown of the tooth, the second premolar and even the first molar can be removed. When removing a tooth, attention should be paid to the passage of the midline between the incisors, and the choice of the tooth to be removed should be such as not to aggravate the asymmetry of the position of the incisors of the upper and lower jaws.
Treatment of oral position of teeth should include normalization of the position of the tooth and its placement in the dentition. It is necessary to find out whether there is room for this tooth. If there is space, the tooth or group of teeth is moved using orthodontic appliances.
If the upper anterior teeth are in a palatal position, a plate is made for the upper jaw with a sectoral cut or protracting springs. A stable Angle arch can be made and by activating the ligatures or nuts the teeth will be moved in the labial direction. When the upper incisors are in a palatal position, Bynin and Schwartz mouthguards and a Reichenbach-Brückle plate with an inclined plane are used. The use of a positioner with a preliminary setup system is also shown.
In case of crowded position of the lower front teeth and their lingual position, which arose as a result of macrodentia, it is advisable to take the path of removing complete teeth. First you should pay attention to the passage of the midline. The tooth to be removed can be a central or lateral incisor, as well as a first or second premolar. It all depends on the lack of space in the dentition and the location of the lower incisors in relation to the midline. If the space deficit is greater than the size of the incisor, and the midline is not displaced, then the abnormally located tooth is removed. If the midline is displaced to one side or the other, then the tooth on the opposite side of the midline displacement is removed.
The question of removing the first or second premolars is decided depending on the lack of space, taking into account the violation of the closure of the lateral teeth.
It must be remembered that the removal of any incisor on the lower jaw leads to aggravation of the depth of the incisal overlap.
When the upper or lower teeth are in an oral position, the closure of the dentition is disrupted. Thus, with a palatal inclination of the upper anterior teeth, a deep incisal occlusion is formed. This is typical for class II of the 2nd subclass of Angle. Otherwise, it is distal occlusion of the dentition in combination with palatal inclination of the upper incisors. With a significant palatal position of the upper incisors, reverse incisal occlusion, or disocclusion, is formed.
In this case, it is necessary to take into account the separation of the dentition in order to eliminate blocking of the upper and lower incisors. For this purpose, plate devices are made with occlusal linings in the lateral areas of the dentition. To eliminate the pressure of the orbicularis oris muscle on the upper incisors, it is necessary to make a labial plastic bandage. You can separate the dentition using mouthguards or orthodontic crowns.
If the upper lateral teeth are in a palatal position, it is advisable to use a plate on the upper jaw with a sectoral cut and occlusal overlays on the opposite side of the dentition. When a palatal position of the upper incisors is combined with a mesial position of the lateral teeth, it is necessary to either move the lateral teeth distally or remove complete teeth (usually the first premolar - one or both sides). Thus, a place is created in the dentition for the frontal teeth, after which they are moved in the labial direction.
Very good results are achieved when treating crowded lower anterior teeth with a lip bumper. This device allows you to change the myodynamic balance between the orbicularis oris muscle and the tongue muscles. Treatment of anomalies in the vertical position of teeth involves reducing or increasing the dento-alveolar height in the corresponding section. Reducing the dento-alveolar height is achieved by creating vertical loads on the corresponding teeth to induce the process of bone resorption.
Dental alveolar elongation in the area of one tooth or a group of teeth may be associated with the absence of antagonist teeth or the presence of bad habits. Dentoalveolar elongation of the lateral teeth of the upper jaw is often observed, which leads to vertical incisal disocclusion. Dentoalveolar elongation of the lower anterior teeth leads to deep incisal disocclusion or occlusion. When dentoalveolar lengthening of the lateral teeth occurs, they should be introduced.
Treatment is carried out with a plate on the lower jaw with occlusal pads, and dentoalveolar lengthening of the lower anterior teeth is carried out with a plate on the upper jaw with a bite pad. An Andresen-Goipl monoblock and positioner are used.
When dentoalveolar lengthening of one tooth is carried out, it is implanted and then an apparatus is necessarily made for the opposite dentition with an artificial antagonist tooth.
When the tooth is suprapositioned, another task is to increase the dentoalveolar height in the corresponding section as a result of bone building. This is achieved by physiological irritation by applying a rubber ring and creating traction that transfers the load through the periodontium to the bone structures. The point of application of force is a hook on a ring fixed to the tooth being moved (crowns or braces are possible), the fulcrum is a hook on a mouthguard blocking antagonist teeth, or a hook in the design of an apparatus used in complex treatment. At the end of the change of teeth and after it, you can use a bracket system, as well as a stationary Angle arch. It should be noted that after eliminating such an anomaly, a long retention period is usually required.
Treatment of tortoanomalies involves creating a pair of forces directed in the directions opposite to the rotation of the tooth. This is achieved by creating two points of force application on the crown of the tooth being moved. The points of application of force can be hooks on rings, crowns or braces, and the points of support can be hooks on aligners blocking groups of teeth, or fixed in basic appliances. When elastic rings are applied, a pair of multidirectional forces is created, which leads to normalization of the tooth position. It is extremely important to maintain constant optimal traction. Tortoanomaly is also eliminated with the help of positioners.
At the end of the change of teeth and after it, the tortoanomaly can be eliminated using a brace system or an Angle arc, if there are other indications for their use. Treatment of tooth transposition. If such an anomaly is present in the area of the front teeth, the cosmetic and functional effect is often achieved by grinding (for example, when there is a canine in place of the incisor). Depending on the combination of clinical factors, it may be preferable to restore the optimal shape of the tooth using an orthopedic crown. In the area of the lateral teeth, grinding is usually sufficient.
Problems arise when there is transposition of the teeth and these teeth are abnormally positioned. For example, in the place of the canine there is a first premolar, the canine is vestibular at the level of the first premolar, and in the dentition there is a second premolar (in place of the first premolar), then the first and second molars. If there is a rudiment of a wisdom tooth, it is necessary to remove the vestibular canine. In the absence of a wisdom tooth rudiment, distal displacement of premolars and molars and movement of the canine in the dentition to its place are possible.
Distal movement of teeth is carried out using a plate with a sectoral cut, arm-shaped springs, a Kalamkarov apparatus, a face bow, and a positioner. It should be noted that dental anomalies lead to anomalies of the dentition and anomalies of occlusion.
Is an impacted tooth always subject to extraction?
No not always. There are a number of indications for the removal of impacted teeth in which surgical intervention cannot be avoided. These include cases:
- development of pulpitis or periodontitis in an impacted tooth. This applies to teeth that have not fully erupted. Due to the fact that they are difficult to clean and are often covered with a gingival hood, such teeth are more susceptible to caries and inflammatory processes. Considering their special position in the mouth and the extremely difficult access to them, there is no point in sanitizing impacted units, because In any case, treatment will be unsuccessful.
- swelling of the cheek due to the formation of pericoronitis - inflammation of the gingival fold covering an incompletely erupted tooth. Food often gets clogged under the hood, which is quite difficult to clean out with ordinary hygiene products, so the inflammatory process is quite common in such situations.
- formation of periostitis, or flux, against the background of caries or pulpitis of the impacted unit. If the process had formed around the “correct” tooth, then the doctor would have the opportunity to eliminate the inflammatory process either with the help of pharmaceuticals, or by making an incision in the gum and installing drainage into it. However, when it comes to impacted teeth, such measures are ineffective, so the patient has to say goodbye to the “troublemaker.”
- constant discomfort and pain due to the pressure of the unerupted unit on the nerves running along the jaw. In this case, the tooth can be absolutely intact and not interfere with the rest of its brethren.
- the need for orthodontic treatment to correct the bite. If an impacted tooth interferes with its neighbors, for example, moves them and causes them to crowd together, then this is a direct indication of removal. In addition, impacted units must be removed if they impede the movement of the remaining teeth in the dentition.
- preparing the oral cavity for prosthetics. If an impacted tooth cannot be “pulled out” using orthodontic methods and placed in the dentition in order to be used in the future as a support, for example, for a bridge structure, it is removed, because it only worsens the situation and reduces the quality of the treatment provided.
Please note: even if nothing bothers the patient and the impacted figure eight does not affect the general situation in the oral cavity in any way, a consultation with a dental surgeon and a computed tomography scan of both jaws is necessary. The doctor will be able to comprehensively assess the whole picture and draw conclusions about the advisability of removal. He will talk about the immediate and long-term consequences of removing an impacted wisdom tooth, and the prognosis of surgical treatment in relation to the patient’s orthodontic health.
It also happens that a person complains of headaches or clicking in the temporomandibular joint, but it turns out that the problem lies in abnormally erupted or incorrectly positioned third molars. Naturally, in such cases, the best solution would be to remove the problem teeth.
Removing the root of a decayed tooth
Cases where a root remains after tooth extraction are not uncommon. Its removal is a difficult and unpleasant procedure for the patient, even despite the effectiveness of modern anesthesia. Fortunately, the need to remove tooth roots does not always arise. If the root is healthy enough, it is treated and prosthetics are performed. However, removing a rotten tooth root is simply necessary, since its preservation will entail a number of problems:
- Halitosis (bad breath);
- A breeding ground for infection in the oral cavity, possible damage to neighboring teeth;
- The appearance of subgingival stone;
- Spread of infection to the maxillary sinuses, development of osteomyelitis;
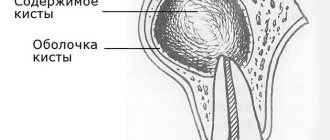
- The appearance of cysts and granulomas at its apex ( removing a tooth with a cyst on the root
is a complex procedure); - A decrease in the body’s overall immunity due to the fact that it is forced to constantly fight the source of inflammation.
In order to properly plan the operation, our dentist performs an x-ray examination. The operation itself is performed using local anesthesia, dental forceps or an elevator. Removing the roots of the front teeth
is carried out using rotational movements, and lateral movements using rocking. The most complex cases may require additional manipulations, the use of burs and special microsurgical dental instruments. Removing the roots of the teeth of the lower and upper jaw is a more complex procedure than removing a whole tooth. It requires special training, which consists of examination, diagnosis and sanitation of the oral cavity. The treatment plan is drawn up based on diagnostic studies and the patient’s indications.
In what cases is a dystopic tooth removed?
As we have already figured out, a dystopic tooth is one that has completely erupted, but is located in a non-standard place for itself and thus changes the condition or location of neighboring teeth. Therefore, the following indications for removing a dystopic tooth help the doctor decide whether to leave it or not:
- presence of displacement of adjacent teeth;
- permanent injury to the oral mucosa, lips or tongue;
- stimulation of the development of cysts, inflammation or other pathological processes in surrounding tissues.
It is worth noting that removal is carried out only if it is impossible to correct the situation in any other way (for example, orthodontically) or if the patient does not agree to such measures.
Causes of dystopic wisdom teeth
Most experts agree that the main cause of dystopic teeth is genetic predisposition. This is also true in the case of wisdom teeth: if the structural parameters of the parents’ jaws contributed to the occurrence of such an anomaly, then their children also have a high risk of developing dystopic teeth. In addition to genetics, there are a number of other factors that influence the position of the wisdom tooth during eruption:
- incorrect formation of tooth buds at the stage of intrauterine development;
- malocclusions, including those caused by mechanical damage;
- macrodentia, presence of supernumerary teeth, small jaw;
- early loss of baby teeth.
How can you remove a tooth located deep in the jaw?
The doctor carefully prepares for the operation of removing an impacted tooth, because This is obviously a more complex manipulation. The less of the crown part has come out from under the gums, the more trouble there will be. It is no coincidence that they say: the most difficult thing is removing an impacted dystopic tooth. Not only does it need to be exposed and freed from the bone, but it also needs to be removed in such a way that no small parts remain in the jaw. But first things first.
Before surgery, the patient is always sent for a CT scan. The information from this examination allows the doctor to understand the location and depth of the tooth, whether it has contacts with neighboring units, the location and shape of the roots, proximity to the nerves of the jaw and other important anatomical structures. Only after this can you plan the course of the operation, the type of anesthesia, the required instruments and auxiliary equipment.
A few words about pain relief methods when removing impacted teeth. In general, they are not much different from those with simpler and less labor-intensive removals. It is believed that these operations are somewhat more traumatic and take a long time. Not at the Refformat clinic. With us you will quickly part with your wisdom teeth. Therefore, you should not be scared, but if you are very scared of dentists in general, we can offer the option of treatment in your sleep. You can find out what this method is here and here.
The patient does not require special preparation, however, in cases where the operation will be performed under sedation, he should first undergo a small set of tests and consult with a therapist.
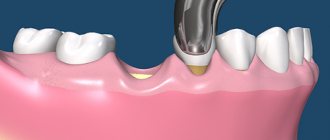
After the onset of anesthesia, an incision is made in the gum exactly above the place where the causative tooth lies, which provides access to the periosteum and jaw bone. The dissected tissues are carefully pulled apart. Then they proceed according to one of the options - either they drill out the bone around the tooth in order to remove it entirely, or the tooth is divided into parts with burs and removed in parts. The method of removing impacted and dystopic teeth in some cases involves filing down the crown part, and then dividing and extracting the roots. If a nerve passes near the coronae, a coronotomy can be performed - removing only the supragingival part of the tooth, while the roots will remain in place.
The operation ends with returning the soft tissue flaps to their place and suturing the wound with nylon or self-absorbing threads. To prevent postoperative complications, the doctor may inject an anti-inflammatory drug into the transitional fold, as well as prescribe antibiotics for up to 5 days.
If the sutures were applied with synthetic threads, they are usually removed after a week and a half. There is no need to remove catgut sutures.
Types of wisdom teeth dystopia
All types of dental dystopia differ in the position of the tooth relative to the dentition. Diagnosis of pathology is carried out by a dentist-therapist or an orthodontist. To determine the type and characteristics of pathology in dentistry, an orthopantomogram is used, as well as targeted x-rays.
| Type of dystopic tooth | Description |
| Medial impacted tooth | The tooth protrudes forward (from the outside of the dentition). |
| Distal impacted tooth | The tooth protrudes backwards (from the inside of the dentition). |
| Angular dystopic tooth | An impacted tooth is located at an angle in relation to neighboring teeth. |
| Tortoposition | The tooth is rotated around its axis |
| Horizontal impacted dystopic tooth | The impacted dystopic tooth is located horizontally relative to the dentition. |
| Reverse dystopic impacted tooth (rare) | The root part is located at the top, and the coronal part at the bottom (in the bone tissue). |
Impacted dystopic wisdom teeth are the most difficult case. The tooth not only has an incorrect position, but also has problems with eruption. Retention can be either partial (part of the tooth is visible on the surface) or complete (the tooth is completely hidden in the soft tissues).
How does the postoperative period proceed?
After removal of an impacted wisdom tooth, minor pain and swelling in the cheek are quite natural. They usually go away 2-3 days after surgery. To reduce these phenomena, the doctor prescribes painkillers, and ice can be applied to the cheek on the extraction side. Incomplete opening of the mouth and discomfort in the throat when swallowing and chewing are also considered normal, which goes away on its own after 3-4 days.
But severe pain after removal of an impacted wisdom tooth is a reason to visit the doctor who performed the operation, because
this may be a sign that the wound needs additional treatment. Another reason that should force you to immediately see a doctor is an increase in body temperature above 37.5°. To the list of posts
Why does retention occur?
Most often, wisdom teeth cannot fully erupt. This is due to the peculiarities of their location. In the process of evolution, eights have lost their meaning. Some people don't have them at all. In others, they often “sit” under the gum and contribute to the displacement of neighboring units, which causes the bite to change.
Retention is caused by:
- heredity;
- premature removal of baby teeth, which leaves little room for constant sweat;
- excessively thick gum walls (very rare);
- malocclusion, severe crowding.
What is the complexity of the operation to remove an atypical wisdom tooth?
Removal of a wisdom tooth in an atypical position is complicated by a number of objective reasons. These are not ordinary tooth extraction operations, when you can use forceps. A third molar located at an angle cannot be removed with forceps, otherwise injury to neighboring teeth and gums cannot be avoided. Such teeth should be removed using special surgical instruments with incisions.
Atypical tooth extraction refers to a number of complex dental operations. Such removal requires appropriate qualifications of a dental surgeon. Often, due to the abnormal position of the tooth, removal is carried out in several stages - the figure eight is removed in parts. The medical literature describes other circumstances that make operations to remove third molars difficult.
Another circumstance that complicates the removal of an atypical wisdom tooth is its proximity to the maxillary sinus or nerve. Sometimes you have to refuse surgery because there is a high risk of hitting a nerve.
Rehabilitation after atypical wisdom tooth extraction
After 10-14 days, the patient's stitches are removed. Until this moment (until the gums heal), the patient should adhere to the following recommendations:
- Avoid overheating your body. Avoid hot baths, saunas and sunbathing for a while. Also avoid strenuous exercise, as this increases the chance of bleeding from the wound.
- Rinse your mouth with solutions prescribed by your doctor.
- Chew food in the area opposite the area being operated on.
- Take medications prescribed by your doctor, such as anti-inflammatory and antibacterial drugs.
How is atypical wisdom tooth extraction performed?
Dental operations require proper preparation and consideration of circumstances that influence the result. Let's take a closer look at the stages of atypical wisdom tooth removal.
- Stage 1
- Stage 2
- Stage 3
- Stage 4
- Stage 5
- Stage 6
- Stage 7
Diagnostics. The doctor carefully examines the patient’s oral cavity and conducts a survey. An X-ray examination is performed to assess the position of the wisdom tooth in the jaw. It is important to understand the placement of the tooth in three projections, which can be determined by computed tomography (three-dimensional radiography).
Preparing for surgery . The day before the operation, the patient undergoes professional teeth cleaning and tartar is removed. In some cases, to provide access to the figure eight, it is necessary to remove the tops of nearby teeth. Therefore, before surgery, it is important to properly prepare the dentition, and the canals of nearby teeth should be filled with cement.
Anesthesia . The patient is given local anesthesia before the operation. If we are talking about removing a wisdom tooth in the upper jaw, then in such cases infiltration anesthesia is often sufficient, which numbs the nearby tissues.
Removal of a wisdom tooth in the lower jaw, in addition to infiltration, also requires conduction anesthesia. This is a type of local anesthesia in which an anesthetic is applied to the nerve fibers. With the help of conduction anesthesia, it is possible to numb not only the operated area, but also other parts of the face.
Gum incision . An incision is made to gain access to the atypical wisdom tooth. Depending on the location of the tooth and a number of other features, this is a trapezoidal, arcuate or angular incision. An incision is made through the thickness of the mucous tissue to the bone. Not only the mucous membrane is opened, but also the periosteum.
Removal of a tooth . Complex wisdom tooth removal is performed in parts. Depending on the situation, the doctor visually divides the tooth into 2 or 3 parts, each of which is removed separately.
Cleaning the tooth socket . After the operation, the doctor cleans the tooth socket of small fragments and other elements. This is done using a curette.
Stitching . The final stage of the operation for atypical wisdom teeth removal is the placement of osteoplastic material (to speed up healing) and suturing.
- Stage 1
- Stage 2
- Stage 3
- Stage 4
- Stage 5
- Stage 6
- Stage 7