What can inflammation of the salivary gland ?
Read the answer to this question in this article. The human body is a complex mechanism consisting of a huge number of organs and systems. Several structures are responsible for performing the same function, constantly complementing each other. For example, different organs take part in the digestion process.
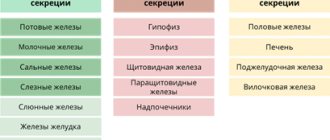
In the human body during normal development there are three pairs of salivary glands
The parotid gland is most often affected by various diseases. There are a number of diseases in which the sublingual and submandibular salivary glands become inflamed. If you do not start treatment on time or undergo inappropriate therapy, then serious complications may occur after such diseases, such as encephalitis, orchitis, meningitis, nephritis, neuritis and pancreatitis. However, do not worry, treatment often gives positive results. To avoid inflammation of the salivary glands, you just need to follow a few recommendations.
Etiology of the disease
The disease most often affects children, but sometimes adults also get it. The latter have a severe course of sialadenitis, especially in men.
Inflammation of the salivary gland occurs for various reasons under the influence of many factors, so the disease is classified as polyetiological. But one condition always precedes the pathological process - the presence of a pathogen, an infectious agent. In most cases, these are either viruses or bacteria.
The most common prerequisites for inflammation of the salivary glands:
any source of infection located in the mouth and ear; carriage of pathogenic or conditionally pathogenic microorganisms; tuberculosis, syphilis, HIV; metabolic disorders; any immunodeficiency conditions; scarlet fever, rubella, measles and other infectious pathologies; viral diseases such as influenza, cytomegalovirus; mycoses; pneumonia, bronchopneumonia; oncological diseases; benign lymphoreticulosis.
The most common mechanisms of transmission of this infectious disease are: airborne, contact, blood-contact, and single-gene.
Three types of inflammation of the salivary gland
Depending on the disease, there are three types of inflammation, namely catarrhal, purulent and gangrenous. First of all, a swelling forms in the area of the salivary gland, which is often accompanied by pain. The inflamed area becomes red, and the skin there is tense and shiny. The exit site of the gland duct has a limited area of edema and inflammation.
In most cases, a specific liquid is released from it, similar to saliva or pus. Body temperature rises sharply to 39 degrees. Opening your mouth becomes more and more difficult and painful. If treatment is not started on time, the disease will develop into a more severe form with serious consequences.
How does salivary gland cancer develop?
Oncology begins with the appearance in the body of just one altered cell, different from healthy ones. It becomes like this due to various diseases and exposure to certain chemicals, multiplies, creates many copies of itself and creates a tumor. Most of these cells detect and destroy the immune system, but some manage to evade or resist our natural defenses. In addition, they have special properties - they are able to move throughout the body using the circulatory and lymphatic systems. The lymphatic system complements the cardiovascular system. The lymph circulating in it - the intercellular fluid - washes all the cells of the body and delivers the necessary substances to them, taking away waste. In the lymph nodes, which act as “filters,” dangerous substances are neutralized and removed from the body. systems Blood and lymph transport them to other organs, where they take hold and create metastases - additional foci of the disease. Such neoplasms gradually increase in size, destroy all tissues located next to them and disrupt their functioning.
What are salivary glands and how do they get affected by cancer?
These important organs produce saliva - a liquid that not only moisturizes our mucous membranes, but also contains enzymes - proteins that start the process of digesting food. In addition, they contain special substances that help prevent the development of infections in the mouth and throat. There are 3 sets of large glands on each side of our face:
- The largest: parotid
- located in front of the ears. Up to 7 out of 10 tumors develop in them, most of which are benign, that is, not cancerous - they do not grow into nearby tissues and do not create metastases - additional foci of the disease in other tissues. - Submandibular
- located under the lower jaw. They secrete saliva under the tongue. Approximately 1-2 out of 10 neoplasms arise in them, about half of which are malignant. Malignant tumors are called tumors whose cells multiply uncontrollably, destroy surrounding tissues and create metastases - additional neoplasms in other organs located far from the main focus of the disease. - The smallest: sublingual
- located under the oral cavity on both sides of the tongue. In them, oncology begins quite rarely. - In addition to the above, there are several hundred small salivary glands, which can only be seen under a microscope. They are located under the mucous membrane of the lips and tongue, in the palate, inside the cheeks, nose and larynx. Tumors in them are not common, but the vast majority of them are cancerous.
It is very difficult to diagnose this disease in the early stages.
In most cases, patients notice that something is wrong when the stone prevents the complete drainage of fluid. All this is accompanied by sharp pain, similar to salivary colic. At the site of inflammation, the tissues swell and become swollen. These symptoms are not constant, the pain either increases or disappears. During treatment, the stone is removed; if the situation is too advanced, sometimes the entire gland is removed.
The salivary glands under the tongue extremely rarely. But at the same time, the disease develops at a rapid pace and can have adverse consequences.
In order to maintain your health, first of all, you must adhere to the rules of hygiene and if you experience the slightest discomfort, immediately consult a doctor.
Inflammation of the salivary gland under the tongue
Types of salivary gland tumors
Almost all neoplasms arising in these organs are benign
, that is, they are not related to oncology and do not spread to other parts of the body. Most of them are treated surgically and are extremely rarely life-threatening - as a rule, their degeneration occurs with prolonged absence of therapy or re-growth after partial removal. The mechanism and principles of this transformation are not known to doctors today.
A minority of tumors are malignant
, capable of destroying tissues into which they grow and creating metastases - additional foci of disease in other organs:
- Their most common type is mucoepidermoid cancer
, most often starting in the parotid glands. It is generally slow growing and responds well to treatment. - Adenoid cystic carcinoma
: usually does not develop quickly, but can recur - appear again after therapy, including many years later. Recovery prognosis largely depends on the size of the tumor - the smaller it is, the better the prospects. - Many subtypes of adenocarcinoma
: formed in gland cells that secrete various substances. They grow slowly, but appear at a younger age than other types of cancer.
Rare types of malignant tumors:
- Squamous cell carcinoma
: occurs mainly in older men. The prognosis for its owners is unfavorable. - Epithelial-myoepithelial carcinoma
: usually grows slowly, but can recur - come back after treatment, and spread to other parts of the body. - Anaplastic small cell carcinoma
: Most often develops in the minor salivary glands, grows rapidly, and its cells are similar to those that make up nerves. - Undifferentiated carcinomas
: often spread quickly and are difficult to treat, and the outlook for patients with this diagnosis is generally poor.
In addition to the above, other types of oncology can develop in these organs:
- Non-Hodgkin's lymphomas
: formed in the cells of the immune system of the glands, behave and are treated differently from other types of tumors. - Sarcomas
: Occur in cells of blood vessels, muscles and connective tissue. - Secondary cancer
: begins in other organs and spreads to the salivary glands.
Treatment
Therapy for sialadenitis is carried out in a hospital. Most often, signs of pathology are eliminated with the help of medications and physiotherapeutic procedures. Less commonly, doctors resort to surgery to cleanse or remove the gland. The operation is indicated for purulent or gangrenous type of problem.
For mumps, patients are prescribed antiviral drugs. Symptomatic treatment is also carried out, aimed at reducing the temperature and relieving pain in the affected area.
Acute blockage of the salivary gland requires complex therapy. To normalize the function of the gland, patients are prescribed a special salivary diet. The diet includes crackers, sour fruits and vegetables, and berries. Drink a 1% solution of pilocarpine hydrochloride orally. The substance promotes contraction of the muscles located next to the salivary gland. All measures are aimed at accelerating the removal of foreign objects and pathogenic particles by enhancing the secretory function of the gland.
If the disease is infectious, the use of antibacterial agents is required. Penicillin antibiotics and antiseptic solutions are injected into the ducts to disinfect the affected area (Miramistin, Dioxidin)
To relieve swelling and inflammation, compresses with Dimexide are applied to the problem area. The procedure is carried out twice a day for 30 minutes. The drug also reduces the intensity of pain.
Additionally, the inflamed glands are heated using UHF. If the situation worsens, a novocaine-penicillin blockade is performed. The procedure is necessary to prevent infection of neighboring tissues.
Chronic sialadenitis is treated according to a different scheme:
- The inflamed ducts are massaged daily with the introduction of antibacterial drugs. The procedure acts as a prevention of purulent complications of sialadenitis.
- Injections with novocaine are made into the subcutaneous fat to improve the secretory function of the glands.
- For 10 days they undergo daily treatment with electric currents.
- To prevent exacerbation of the pathology, iodolipol is injected into the problem area once every 3 months.
Prevention of violation
There are no vaccines or specially developed drugs against sialadenitis. The only exception is mumps. To prevent the development of the disease, the child is offered an inactivated vaccine against measles, mumps and rubella. All children over 1 year of age are vaccinated against the disease. After the vaccine, stable immunity to the pathogen remains in 96% of vaccinated people.
There are also nonspecific measures to protect against sialoadenitis, including:
- regular oral hygiene;
- timely treatment of wounds and mouth ulcers;
- elimination of chronic foci of infection;
- prevention of saliva stagnation in infectious diseases.
Treatment of salivary gland blockage should be carried out promptly. Otherwise, the disease threatens infection of the soft tissues of the face and further infection of the body. The consequences of sialadenitis require resuscitation measures to preserve the life and health of the patient. The list of dangerous consequences of pathology also includes: rapid destruction of enamel, disruption of oral microflora, chronic inflammation of the gums. For this reason, it is important not to bring your health condition to a critical level.
Causes of salivary gland cancer
Doctors and scientists do not know the exact causes of this disease - they only know about the factors that can lead to the occurrence of this event.
- These include exposure to radiation
, including that received in the workplace or as a result of radiation therapy in the treatment of other types of tumors. - Age
: The older a person is, the higher their risks. - Gender
: this type of dangerous neoplasm occurs more often in men than in women. - Family history
: blood relatives of those who already have a similar diagnosis are more likely to become a patient of an oncologist.
Some studies have shown that frequent contact with silica and asbestos, bad habits such as alcohol and smoking, and a diet low in vegetables and high in animal fats can trigger the development of cancer. In addition, according to incompletely confirmed data, workers in woodworking and rubber industries, as well as people interacting with certain metals, including nickel alloy dust, are more likely to get sick. This information cannot be called absolutely accurate, since dangerous tumors of the salivary glands are quite rare, which makes them difficult to study.
Theory and practical experience in ultrasound diagnosis of salivary gland pathology
Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.
In domestic and foreign literature there are many works devoted to sialogy (from the Greek Sialon - saliva and logos - study) - the science of diseases and injuries of the salivary glands, methods of their diagnosis and treatment. According to various authors, diseases of the salivary glands account for up to 24% of all dental pathologies. Currently, in clinical practice, the most common are dystrophic, inflammatory diseases of the salivary glands (sialoadenoses, sialadenitis), as well as tumors and congenital malformations of the salivary glands. In addition, pathological changes in the salivary glands often accompany other diseases (diabetes mellitus, bronchiectasis, sarcoidosis, liver cirrhosis, hypertriglyceridemia, lymphogranulomatosis, etc.).
Various instrumental methods are used to diagnose diseases of the salivary glands [1]:
- radiography (if the formation of stones in the ducts of the salivary glands is suspected, but in 20% of the stones of the submandibular salivary glands and 80% of the parotid salivary glands are non-radiographically opaque);
- sialography (examination of the ducts of the salivary glands with a radiopaque substance, is rarely useful in differentiating tumors from inflammatory processes, but it can help differentiate the mass formation of the salivary glands from formations in neighboring tissues. In patients with suspected autoimmune disease of the salivary glands, a characteristic pattern of saccular expansion may be detected ductal system. In case of acute infection of the salivary glands, sialography should not be performed [2]);
- computed tomography together with sialography;
- ultrasound method (is the most accessible, safe and informative in the process of differential diagnosis of the pathological condition of the salivary glands).
Anatomy of the salivary glands [3]
There are three pairs of major salivary glands (SG) and many small ones. The large ones include paired parotid, submandibular and sublingual SGs. The parotid salivary gland (PSG) is located on the outer surface of the branch of the lower jaw at the anterior edge of the sternocleidomastoid muscle, as well as in the retromandibular fossa. Dimensions vary widely: length 48-86 mm, width 42-74 mm, thickness 22-45 mm. The OSJ is covered by the parotid fascia, which is its capsule and is tightly fused with it. Sometimes, at the anterior edge of the parotid duct, there is an additional lobule measuring 10-20 mm, which has its own duct flowing into the parotid. The parotid duct emerges from the gland at the border of its upper and middle thirds, then it passes along the outer surface of the masticatory muscle parallel to the zygomatic arch and turns 90° inward, penetrating the fatty tissue and buccal muscle. The projection of the parotid duct onto the skin of the cheek is determined on the line connecting the tragus of the auricle and the corner of the mouth. The parotid duct opens in the vestibule of the oral cavity at the level of 1-2 large molars. The diameter of the duct is on average 1.5-3.0 mm, its length is 15-40 mm. The thickness of the gland contains the branches of the external carotid artery, the facial nerve and its branches, and the auriculotemporal nerve. There are many lymph nodes around the OUSG and in its parenchyma (Fig. 1), which can serve as a primary or secondary collector for draining lymph from teeth and oral tissues.
Rice. 1.
Lymph nodes in the thickness of the parotid salivary gland.
The submandibular salivary gland (MSG) is located in the submandibular triangle between the body of the mandible and the anterior and posterior bellies of the digastric muscle. The dimensions of the gland are: anteroposterior 20-40 mm, lateral 8-23 mm, superior-inferior 13-37 mm. Posteriorly, the PNJ is separated from the OSJ by a process of the fascia propria of the neck. The medial surface of the gland in the anterior section lies on the mylohyoid muscle. The submandibular duct, bending over the posterior edge of this muscle, is located on the lateral surface of the hyoglossus muscle. Then it goes between the medial surface of the hyoid gland and the genioglossus muscle to the point of its exit in the area of the hyoid papilla. The facial artery and its branches, the lingual artery and the veins of the same name pass through the gland.
The sublingual salivary gland (SSG) is located on the floor of the mouth in the sublingual region parallel to the body of the lower jaw. The dimensions of the gland are: longitudinal 15-30 mm, transverse 4-10 mm and vertical 8-12 mm. The duct of the parathyroid gland passes along its inner surface and opens in the region of the anterior section of the sublingual ridge independently or together with the submandibular duct. Sometimes the PJS duct flows into the middle section of the PJS duct.
The minor salivary glands - labial, buccal, lingual, palatine, incisive - are located in the corresponding areas of the mucous membrane. They can be a source of development of adenocarcinomas of the oral cavity.
Pathology of the salivary glands
SG malformations are rare. The most common are anomalies in the size of the glands (agenesis and aplasia, congenital hyperplasia (Fig. 2) and hypoplasia), their location (heterotopia, accessory glands), and anomalies of the excretory ducts (atresia, stenosis, ectasia, cystic transformation, ductal dystopia).
Rice. 2.
Hyperplasia of the left sublingual salivary gland.
Sialadenitis is a large group of polyetiological inflammatory diseases of the gastrointestinal tract (Fig. 3). Primary sialadenitis - sialadenitis considered as an independent disease (for example, mumps). Secondary sialadenitis is sialadenitis that is a complication or manifestation of other diseases (for example, sialadenitis with influenza). The echographic picture for different etiologies is not very specific. Etiology has clinical significance in determining treatment tactics.
Rice. 3.
Sialadenitis of the right submandibular salivary gland.
According to the etiological factor, sialadenitis is classified [4] into:
- sialadenitis developing under the influence of physical factors (traumatic sialadenitis, radiation sialadenitis (Fig. 4) occurs during radiation therapy of malignant tumors of the head and neck);
- sialadenitis developing under the influence of chemical factors (toxic sialadenitis);
- infectious sialadenitis (routes of infection penetration into the fluid: stomatogenic (through ducts), contact, hematogenous and lymphogenous);
- allergic and autoimmune sialadenitis (recurrent allergic, Sjogren's disease and syndrome, etc.);
- myoepithelial sialadenitis caused by a pathological process, previously designated as a benign lymphoepithelial lesion. The term benign lymphoepithelial lesion was first used by JT Godwin in 1952, replacing the concept of Mikulicz disease;
- obstructive sialadenitis, which develops when there is difficulty in the outflow of saliva due to obstruction of the excretory duct with a stone (Fig. 5-7) or thickened secretion, as well as due to cicatricial stenosis of the duct. According to the prevalence of the process, they distinguish between focal, diffuse sialadenitis and sialodochitis - inflammation of the excretory duct. The course of the process can be acute or chronic;
- pneumosialadenitis, which develops when there is air in the gastric tissue in the absence of a bacterial gas-forming infection. Air enters the gland from the oral cavity when the pressure there increases through the duct. Pneumosialadenitis is typical for a number of professions, primarily for glassblowers and musicians playing wind instruments.
Rice. 4.
Post-radiation sialadenitis.
Rice. 5.
Stone of the duct of the submandibular salivary gland.
Rice. 6.
Stone in the parenchyma of the submandibular salivary gland.
Rice. 7.
Stone in the duct of the submandibular salivary gland.
Tumors of the salivary glands
Tumors of the salivary glands are divided into two groups: epithelial and non-epithelial. Epithelial tumors predominate in adults (95%). In children with SG, epithelial and non-epithelial tumors are equally common. In addition to true tumors, processes resembling tumors (tumor-like lesions) develop in the GS.
Among epithelial tumors of the gastrointestinal tract, benign neoplasms are distinguished, as well as malignant ones - carcinomas.
Benign epithelial neoplasms of the stomach include ductal papillomas, adenomas and benign sialoblastoma. SG adenomas are divided into two groups: polymorphic (the most common SG adenoma) and monomorphic (all other) adenomas. Tumors of different structure, origin and prognosis were artificially included in the group of monomorphic adenomas.
Pleomorphic (polymorphic) adenoma (mixed tumor of the gland) is a adenoma of the gland, built from two types of cells: ductal epithelium and myoepithelial cells. Macromorphological picture. The tumor is usually an elastic or firm nodule of lobulated grayish-white tissue, usually partially encapsulated. Typical of a pleomorphic adenoma is the so-called chondroid stroma, resembling hyaline cartilage. Variants of the echographic image of pleomorphic adenomas are presented in Figure 8.
Rice. 8.
Pleomorphic adenoma of the gastrointestinal tract.
Warthin's tumor is an adenolymphoma in which multiple cystic cavities are formed, covered with double-layered epithelium. The papillae protrude into the lumen of the cysts. A pronounced proliferation of lymphoid tissue occurs in the tumor stroma. This tumor almost exclusively develops in the parotid gland.
Other types of benign tumors are less common. These are benign oncocytoma (oxyphilic adenoma), basal cell adenoma, tubular adenoma, benign cystadenoma sialoblastoma.
Among benign primary non-epithelial tumors, the most common are hemangioma, lymphangioma, neurofibroma and lipoma.
Among malignant non-epithelial tumors, malignant lymphomas are more often found (they arise, as a rule, against the background of myoepithelial sialadenitis, Sjögren's disease and syndrome).
Tumor-like lesions of the salivary glands
Rice. 9.
Salivary gland cysts.
- Salivary gland cysts (mucoceles). There are two types of mucocele of the gland: the retention type (retention cyst of the small gland, formed when saliva is retained in the excretory duct) and the type of interstitial secretion, when, when the wall of the duct is injured, saliva enters directly into the fibrous tissue surrounding the gland. Mucoceles in the floor of the mouth are also called ranulae.
- Cysts of the excretory ducts of large SGs are pronounced dilatation of the excretory duct due to retention of secretions in it. Blockage of salivary outflow can be caused by various reasons: tumor, stone, thickened mucus, post-inflammatory stenosis, even cicatricial obliteration of the lumen.
- Sialoadenosis (sialosis) is a non-tumor and non-inflammatory symmetrical increase in SF due to hyperplasia and hypertrophy of secretory cells. The outcome of sialosis is often SG lipomatosis. The process has a chronic relapsing course. Sialosis occurs in a number of diseases and conditions: diabetes mellitus, hypothyroidism, malnutrition, alcoholism, liver cirrhosis, hormonal disorders (hypoestrogenemia), reactions to medications (most often antihypertensive), neurological disorders.
Adenomatoid hyperplasia of small SGs leads to their increase to 0.5-3.0 cm in diameter. The causes of adenomatoid hyperplasia are trauma and prolonged exposure to ionizing radiation.
Oncocytosis is age-related changes in secretory cells and epithelium of the ducts of the gastrointestinal tract. In this case, the SF may slightly increase, but usually their value does not change.
To summarize, I would like to note that ultrasound using Doppler sonography in many of our observations helped to accurately determine the nature of the pathological process in the gastrointestinal tract. However, this diagnostic method does not allow one to unambiguously confirm or refute the malignant nature of the formation of the salivary glands.
Literature
- Benign and malignant tumors of soft tissues and bones of the face. A.G. Shargorodsky, N.F. Rutsky. M.: GOU VUNMTs, 1999.
- Topographic anatomy and operative surgery. I.I. Kagan, S.V. Chemezov. M.: GEOTAR-Media, 2011.
- Salivary glands. Diseases and injuries. V.V. Afanasiev. M.: GEOTAR-Media, 2012.
- Inflammatory diseases of the tissues of the maxillofacial area and neck. A.G. Shargorodsky. M.: GOU VUNMTs, 2001.
Ultrasound scanner HS50
Affordable efficiency.
A versatile ultrasound scanner with compact design and innovative capabilities.