Dr. Chad Duplantis
Clinical dentistry is a series of processes and decisions that affect the quality of care provided. Cementation of indirect restorations is no exception, since there are several options in this area. This article will help doctors make the right decision when choosing a method of fixation of indirect restorations.
| Modified GICs | Self-adhesive composite cements | Adhesive composite cements |
| Meron Plus, Voco | Bifix SE, Voco | Bifix QM, Voco |
| RelyX Luting Plus, 3M | RelyX Unicem, 3M | RelyX Ultimate, 3M |
| Nexus RMGI, Kerr | SpeedCem Plus, Ivoclar Vivadent | Multilink Automix, Ivoclar Vivadent |
| GC FujiCem 2 | Maxcem Elite, Kerr | NX3 Nexus, Kerr |
Introduction
Dental cementation has undergone significant changes since zinc oxide eugenol cement was introduced in 1850. Manufacturers are constantly making minor changes to the composition, which leads to a huge variety of cements and complicates the process of choosing a material. With each generation comes new indications, recommendations, performance characteristics and technologies.
Just like fixation materials, indirect restorations themselves have also achieved significant development and diversity. Prosthetic dentistry has reached heights that the field's pioneers could never have imagined. However, failures can occur if the restoration is not properly worked or cemented. Even the type of restoration - inlay, crown, veneer - can have a significant impact on the choice of luting cement.
This article examines the most commonly used cements from the perspective of cementing the most popular restorations. The main goal is to simplify the process of choosing a fixation method and fixation material for practitioners. Conscious choice of materials allows you to achieve predictably good results.
| Restoration | Cement | Tooth preparation | Preparation of the restoration |
| Zirconium | Cement: good retention only | Ensure the stump is clean (pumice stone or brush) | Sandblast the restoration (50-60 µm aluminum oxide, |
| Bond: self-adhesive composite cement | Ensure stump cleanliness | Sandblast the restoration (50-60 µm aluminum oxide, | |
| Bond: adhesive composite cement | Ensure the stump is clean, etch and/or apply bonding in accordance with the manufacturer's recommendations | Sandblast the restoration (50-60 µm aluminum oxide, | |
| Lithium silicate or disilicate | Bond: self-adhesive composite cement | Ensure stump cleanliness | Etch the restoration with 5% hydrofluoric acid for 20 seconds, apply primer, apply self-adhesive composite cement |
| Bond: adhesive composite cement | Ensure the stump is clean, etch and/or apply Bond in accordance with the manufacturer's recommendations | Etch the restoration with 5% hydrofluoric acid for 20 seconds, apply primer, apply bonding agent, apply adhesive composite cement | |
| Leucite reinforced ceramics | Bond: adhesive composite cement | Ensure the stump is clean, etch and/or apply Bond in accordance with the manufacturer's recommendations | Etch the restoration with 9.6% hydrofluoric acid for 1 minute, apply primer, apply bond, apply adhesive composite cement |
| Hybrid ceramics | Bond: adhesive composite cement | Ensure the stump is clean, etch and/or apply Bond in accordance with the manufacturer's recommendations | Sandblast the restoration (25-50 µm aluminum oxide, 1.5-2 bar), apply primer for 60 seconds, apply bonding agent and adhesive composite cement (follow manufacturer's instructions) |
Cements
In the huge variety of nomenclature, there are three main types of cements, the most widely used in practice and recognized among dentists: chemical, adhesive and self-adhesive cements. Each of these types has not only its own indications, but also an individual protocol for achieving success.
It should be especially emphasized that there is no universal cement that satisfies all the requirements of any clinical situation, therefore knowledge in the field of materials science is necessary.
Chemical cements
Chemical cements simply create a bonding layer between the tooth and the restoration. The bond is ensured by physical factors; chemical bonds (bonding) are not formed.
Modified GICs
Traditional GICs have been used in dentistry for over 40 years. But in 1990, composite-modified GICs were introduced for the first time. Modified GIC showed better properties in comparison with traditional ones due to the addition of methacrylate monomers. They have better bending strength, biocompatibility, and, being chemical cements, provide stronger fixation.
Modified GICs have a number of attractive properties for doctors: they release fluoride ion, do not require the application of an adhesive, and prevent the occurrence of postoperative sensitivity. They are indicated for many types of restorations, although there are reports of fractures in leucite and feldspathic porcelain cemented with MSIC. For successful fixation of prostheses using MSIC, it is necessary to ensure correct retention and stability.
Composite cements
Composite cements are a large group of materials, including many subcategories. The classification below is the most common in modern dentistry. The two main categories of composite cements are adhesive and self-adhesive composite cements.
Adhesive composite cements
Adhesive composite cements appeared earlier than self-adhesive ones. They have many indications for use and should be carefully studied before use. There are chemical, dual and light curing options. To ensure success, there is a detailed bonding protocol that includes pre-treatment of the tooth and the internal surface of the restoration.
Additionally, depending on the type of adhesive, an additional silane coupling agent may be required to bond to the restorative surface. Many shades are available, as well as samples (depending on the manufacturer).
Self-adhesive composite cements
SACCs are often called “universal cements.” Having an initial pH level of 2.1-2.3, they are able to etch the tooth, while the monomers included in their composition provide a bond to the tooth without applying a separate primer or bond (not recommended by most manufacturers). Most of these materials are dual-cured, and although the bond strength is not the same as that of adhesive cements, the bond strength is improved when light activated. Indications for use are extensive: crowns, bridges, inlays made of any materials. However, veneers are not recommended to be fixed using SACC, as color changes may occur as a result.
Dual-cure composite cements
Author: George Freedman
Many restorations in dentistry are made using the indirect method, and they must be fixed in some way to the dental tissues in the oral cavity. Various types of cement luting have been used over the years. Although the adhesive type of fixation is not universal for all cases, it has gained popularity and is increasingly becoming the choice of both patients and clinicians (Fig. 1).
Figure 1 A, supragingival preparation margin. B, Aesthetic crown fixed adhesively.
Compared to older luting cements, adhesive cements are becoming more effective. They make the restoration stronger, more resistant to chipping along the tooth interface, and less susceptible to fracture. Composite cements can be produced in different shades and, thus, more accurately match the color of the tooth. In aesthetic dentistry, the matching of the color of the intermediate material between the tooth and the prosthetic structure is of paramount importance (Fig. 2).
Figure 2. Esthetic restoration demonstrating the matching of the shade of the material at the interface of the tooth and the prosthetic structure.
Generally, cements can be divided into two categories: adhesive and non-adhesive (Box 1).
Non-adhesive cements
Adhesive cements
|
Box 1. Two categories of cements.
When using non-adhesive cements, fixation is carried out due to mechanical retention; they cannot adhesively attach to any fillers; they usually consist of water and reactive fillers. In contrast, adhesive cements form a chemical bond with both the tooth and the prosthetic structure. Their chemical composition does not contain water and consists of a silanized inert filler.
Establishing the mechanical retention required for non-adhesive luting requires considerable manual skill on the part of the clinician (Box 2).
Fixation is achieved through mechanical retention
|
Box 2. Non-adhesive cements.
The tooth stump should have long axial walls. The preparation taper, ideally, should be small, about 6 degrees, and the orthopedic design should have a high precision fit to the tooth (about 30-100 microns). Traditional luting cement fills the space between the restoration and the tooth. For the most part, mechanical retention depends on mechanical features: the outer surface of the tooth core and the inner surface of the restoration must correspond exactly to each other. If this condition is not properly met, it is likely that the structure will soon decement.
The adhesive cement bonds to both the tooth and the structure (Box 3).
Bonds adhesively to both the restoration and the tooth
|
Restorations
According to the Glidewell laboratory, zirconia restorations (solid or layered) are in first place in popularity. In second place by a large margin are restorations made of lithium silicate or lithium disilicate. In third place are crowns based on precious and semi-precious metals. Each type has individual cementation characteristics.
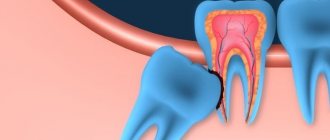
Ceramics and glass ceramics
Many doctors mistakenly believe that ceramics and glass ceramics are the same thing. It is important to understand that ceramics are divided into three main categories: glass ceramics, partially filled glass ceramics, and polycrystalline ceramics. All these materials have specific properties and require an individual approach.
Glass ceramics itself
This type of ceramic is composed of feldspathic minerals and aluminum oxide. Typically, such ceramics are called feldspathic ceramics. Glass ceramics are highly aesthetic and can be used for crowns, veneers, inlays, etc.
Due to increased fragility, glass-ceramic restorations are recommended to be fixed using adhesive composite cements. For successful bonding, it is recommended to etch the inner surface of the restoration with 9.6% hydrofluoric acid for a minimum of 1 minute (maximum 2.5 minutes), then apply MDF primer for one minute and blow with air.
Partially filled glass ceramics
The CNS consists of different types and quantities of particles filling a glass matrix. The strength of these materials is due to the large number of particles embedded in the matrix and the smaller amount of glass matrix. There are three most well-known types: leucite-enhanced, lithium disilicate, and glass-infiltrated alumina. The strength of these types of ceramics increases from the first to the third, and depends on the filler of the glass matrix. These materials are indicated for the manufacture of crowns, veneers, and inlays.
All three types of materials are fixed differently:
- For leucite ceramics – etching with 5% hydrofluoric acid for one minute, adhesive cementation
- For lithium disilicate – etch with 5% hydrofluoric acid for 20 seconds
- For ceramics based on aluminum oxide – sandblasting with aluminum oxide or silicon oxide.
In my opinion, lithium disilicate and glass-infiltrated aluminum are ideal options for adhesive cementation (adhesive and self-adhesive cements). It is possible to cement such restorations with modified GIC; the use of a silane primer is not indicated.
Polycrystalline ceramics
Polycrystalline ceramics are densely sintered aluminum oxide or zirconium oxide. Zirconium oxide is the most popular material among dentists, according to Glidewell Laboratory. Restorations made from this material have many indications in dentistry, including full crowns. Both aluminum oxide and zirconium oxide are silicon-free and metal-free materials and therefore require different handling from conventional ceramics.
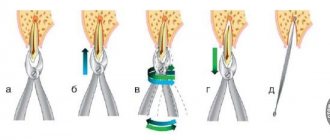
The retention elements of the stump play an important role in the choice of cement. Restorations can be cemented with conventional cement (modified GIC) if the core has good retention characteristics. Bonding is possible if the technology is followed. Dr. Marcus Blatz proposed a uniform concept for bonding zirconium restorations. The internal surface must be sandblasted using 50-60 micron aluminum oxide, under a pressure of 2 bar. The surface is then treated with a primer for zirconium or aluminum. The final stage is the application of dual- or chemical-curing composite cement. It is important not to use light-curing cement as it does not cure completely.
Hybrid ceramics
Hybrid ceramic, first introduced in 2012, is the newest material for the fabrication of indirect restorations. There are several materials of this type. All of them consist of ceramic particles embedded in a composite matrix, up to 80% full. Each manufacturer lists different indications, but all materials in this group are suitable for making crowns, veneers, inlays and implant crowns.
These materials are attractive to CAD/CAM users because they are quickly produced and do not require firing. Each material has a unique bonding protocol. Compliance with this is extremely important for reliable adhesion. Due to variations in composition, it is necessary to strictly follow all manufacturer's recommendations to achieve excellent results.
For luting, I recommend using a dual-curing adhesive composite cement, as these cements work well with hybrid ceramics. Sandblasting is necessary, but hydrofluoric acid is contraindicated for most restorations of this type.
Metal-based restorations
Metal-based restorations have fallen out of favor in modern dentistry (Glidewell Dental Laboratories, 2018). Although there are some variations in metal restorations, they can be cemented in a manner similar to aluminum or zirconium-based restorations. Modified GIC or dual- or chemical-curing composite cements can be used with equal success. When using composite cement, the need to use a primer for the metal is controversial, but no adverse effect has been observed from its use.
Clinical case
It was decided to replace the old metal-ceramic crown of tooth 25 with a restoration made of IPS E.max press – a partially filled glass-ceramic based on lithium disilicate.
The restoration can be cemented using MSIC, self-adhesive or adhesive composite cement. I prefer to cement lithium disilicate restorations using adhesive cements as opposed to zirconium oxide restorations. This is due to the lower strength of these restorations.
The restoration was etched with 5% hydrofluoric acid for 20 seconds as this was not done in the laboratory. Then the inner surface of the restoration was treated with alcohol. Ceramic bond from Voco was applied, exposure 60 seconds. Before applying the cement, the bond was inflated with a blower for uniformity (Fig. 1).
The tooth was anesthetized to reduce sensitivity during the cementation process. After the onset of anesthesia, the tooth stump was treated with 2% chlorhexidine from Ultradent (Fig. 2). This step is optional, but chlorhexidine is a good antiseptic and does not reduce bond strength. Futurabond U from Voco was then applied for 20 seconds and gently inflated for 5 seconds (Figure 3).
Once the restoration and tooth were prepared, Voco's Bifix QM cement was applied and the restoration was carefully secured to the tooth under slight pressure (Figure 4). After installation, the restoration was illuminated for 2 seconds (Fig. 5). Excess cement can be easily removed using a float (Fig. 6), and the restoration is finally polished (Fig. 7-8).
Fixation cements
RelyX ARC Dual Curing Adhesive Composite Cement
Highly esthetic adhesive cement for maximum durability in the Clicker dispensing system
Purpose:
Permanent fixation
• Crowns, inlays and onlays, bridges made of ceramics, metals, metal-ceramics and composite materials
• Ceramic systems based on zirconium/aluminum oxide
• Maryland Bridges
• Endodontic pins
• Stump inlays
Advantages:
• Very high adhesion force to tooth tissue and a wide range of materials
• Aesthetics: choice of shades, excellent optical properties
• 2 curing mechanisms – light and chemical
• The minimum thickness of the adhesive film (12 microns) ensures the most accurate fit of the structure
• Zero solubility in oral fluid – long service life of the structure
• Radiopacity
• Easy-to-work consistency
• Easy to remove excess: cement forms an intermediate gel phase, which makes it easy to remove excess from the 3rd to the 5th minute from the start of mixing
• Clicker™ dosing system – simple, precise and hygienic mixing, no dust
• If necessary, cement can be applied with a brush or applicator
Instructions for use:
• Remove the temporary restoration, prepare the bonding surface of the indirect restoration and the superstructure, if present.
• Silane treatment of ceramic or metal-ceramic indirect restorations: Apply RelyX™ ceramic primer to the bonding surface of the indirect restoration. Dry for 5 seconds
• Using a water/pumice slurry, clean prepared teeth and crown/bridge for placement and bonding. Rinse thoroughly and dry, isolate from moisture and adjacent teeth.
• Use Adper™ Single Bond 2 or Adper™ Easy One as directed.
• Mix the cement for 10 seconds, apply it in a thin layer inside the structure
• Fix the structure, remove excess cement 3-5 minutes after fixation
• After removing excess, light-cure each surface for 40 seconds, or wait until it hardens on its own within 10 minutes from the start of mixing.
Working time including mixing: 2:00 min
Final curing time in the mouth: 8:00 min