Facial injuries are quite common. A jaw bruise is an injury without violating the integrity of the skin and bone tissue.
The main difference between it and a fracture is that the victim is able to close and open his mouth, although this causes serious pain. Only an experienced specialist can identify the problem and carry out differential diagnostics.
Most often, such injuries have a favorable prognosis, but it is necessary to undergo a comprehensive study to exclude possible complications. In addition, you should strictly follow medical recommendations and appear in a timely manner for preventive examinations if necessary.
Pain is the main symptom of injury
Causes of bruises in the maxillofacial area
Most injuries occur unexpectedly and to varying degrees of severity.
Most often they are observed in the following cases:
- falling onto a hard surface;
- due to collision with objects;
- various impacts (road traffic accidents, domestic fights, contact sports).
Falls are the most common causes of injuries to the maxillofacial area
The severity of such injuries largely depends on the affected area, the type of object that affected the bone tissue and age-related changes in facial tissue.
Damage to the lower jaw
This injury is the most common. It occurs in both children, adults and the elderly. The important point is to identify the type of damage as soon as possible and provide first aid. The further prognosis and duration of treatment will depend on this.
A mandibular contusion is a soft tissue injury in the lower parts of the face. As a result, an internal hematoma is formed due to the rupture of small blood vessels.
In the event of a bruise, the bone tissue remains intact and the teeth and gums are not injured. Usually occurs as a result of impact on the maxillofacial area with a blunt object.
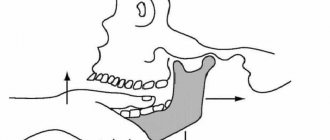
Bruise of the jaw after a blow to the lower parts of the face on the left side
The severity of the injury is largely influenced by the moment of impact. Severe consequences are observed with highly tense muscles. In this case, they rupture, forming an extensive hematoma with a pronounced pain reaction.
Main symptoms
Any disease has its own fundamental signs. Symptoms of a bruise of the lower jaw are usually quite striking. The main sign is sharp pain, abrasions, damage to the cheek or lip.
If the blow falls on the area of the dental arch, then gaping wounds form on the soft tissues on the side of the oral cavity. The lower lip looks swollen, sagging and hyperemic.
To make a correct diagnosis, differential diagnosis is necessary. It is important to exclude fractures of the bone areas of the jaw, eye socket and nose.
After a strong blow, the victim should not be left unattended. It is imperative to monitor his general condition. Together with complaints and external examination, a preliminary diagnosis can be established.
In addition to local signs, general manifestations should also be taken into account:
- damage in the form of scratches and hyperemia in the jaw area;
- swelling in the lower part of the face;
- the presence or absence of hematoma of varying volume;
- malaise and swollen lymph nodes;
- sharp or constant pain even at rest;
- impairment in mouth opening, eating and speaking;
- increased pain response from touching the damaged area, as well as movement of the jaw to the left or right side.
Attention!!! The main differential diagnostic sign of a bruise from a fracture is that the jaw bones do not change their anatomical structure. In addition, the line of bone integrity violation can be determined by palpation.
If the injury is severe, the victim must in any case be taken to a doctor for examination to clarify the condition. It is important to carry out rapid transportation with preliminary first aid.
Types of zygomatic bone fractures
In accordance with the accepted classification, there are several types of fractures, for differentiation of which various criteria are used:
- The presence or absence of displacement, which determines the severity of the damage;
- The area of localization of the injury;
- The period that has passed since the damage occurred;
- Single or multiple, as well as one- or two-sided nature of the injury;
- The specificity of the line along which the fracture runs (straight or oblique).
Characteristic signs of pathology include:
- Limitation of jaw mobility;
- Pain that occurs when trying to open your mouth;
- Distortion of the facial contour and deformation of the bone structure;
- Hemorrhage into mucous tissue, eyelid structure, or conjunctiva;
- Bleeding from the nose from the side of the injured cheekbone;
- Visual disturbances, swelling of the areas around the eyes, severe headache.
At the first suspicion of a fracture of the zygomatic bone, you should consult a doctor and undergo a comprehensive diagnosis.
Damage to the upper jaw
The nature of injury in this area is more complex. Its danger lies in the fact that serious complications may occur. It is quite easy to distinguish a bruise of the upper jaw from the lower one.
This is determined by the location of the pain and the consequences of trauma. However, it should be taken into account that unpleasant sensations can radiate to the lower part of the face. But the main difference here will be the absence of impaired mobility of the lower jaw.
The symptoms of a bruise of the upper bone tissues are very similar to the previous problem. There is an inflammatory process and pain, swelling, and sometimes enlargement of regional lymph nodes. Even if there are no obvious signs of bruises, you need to go to the clinic.
The photo shows fractures of the upper jaw with severe bruises
The doctor must first rule out a fracture. In the upper jaw, such injuries are dangerous for brain damage.
For example, a Le Fort 3 fracture is a separation of the bones of the skull and face. Without professional medical care, death can occur in this case.
Diagnostic measures
If minor injuries to the maxillofacial area occur, they do not require contact with a dentist or surgeon, or urgent hospitalization. If there is severe and prolonged pain, the area of damage should be examined by a specialist.
The following are used as diagnostics:
- taking anamnesis;
- general examination by a surgeon, orthopedic dentist, traumatologist;
- special examination by an otolaryngologist, neurologist and other specialized specialists as necessary;
- X-ray examination of the maxillofacial area;
- CT scan;
- analysis of blood, urine, saliva.
Based on the data obtained, a general picture of the victim’s health is formed and a specific treatment is recommended.
The main therapeutic direction will be the following:
- taking painkillers;
- applying a pressure bandage;
- ensuring maximum peace for the victim;
- prescription of physiotherapeutic procedures;
- local and general anesthesia;
- elimination of hematoma and infiltrate.
Diagnostic methods
To determine a fracture of the zygomatic bone, methods such as visual inspection and palpation are used. In difficult cases, an X-ray examination is prescribed to clarify the severity of the damage, as well as determine the optimal recovery tactics. The resulting image reflects a violation of tissue integrity, as well as a likely decrease in the transparency of the axillary areas and the continuity of the outer radius of the orbit near the affected area.
Features of treatment
The treatment plan is determined by the symptoms of the pathology, the results obtained during the X-ray examination, as well as the assessment based on the results of the medical examination. The priority task is to restore the intact bone structure. In situations where the anomaly is characterized by a displacement of the cheekbone, surgical intervention is prescribed, the purpose of which is to correct the position of the separated elements.
If the injury is not associated with displacement, it is possible to limit oneself to conservative therapy, which involves taking medications selected based on the indications of the clinical picture. The agents used include anti-inflammatory, analgesic, antibacterial substances, and neuroprotectors. In situations where there is a possibility of contact between the wound and a dirty surface, administration of tetanus serum is also recommended. Standard conservative treatment tactics include:
- Ensuring a calm state for a period of 10-14 days, with partial fixation of the jaw;
- Use of low-temperature compresses in the first 48 hours;
- Eating liquid foods and prescribing physiotherapeutic procedures.
In case of severe pain, analgesics are also prescribed. In the future, magnetic therapy, electrophoresis and UHF, as well as other procedural measures, can be used to relieve swelling and pain.
Surgical intervention involves the use of one of the author’s techniques, which include the Keene, Duchant, Dubov and Limberg protocols. Within each operation, the preparatory stage is important, during which the risk to the patient’s health is assessed, the appropriate type of anesthesia is determined, and an action plan is drawn up. The rehabilitation period involves the use of painkillers and antibiotics, as well as a course of physical therapy.
First aid and treatment of bruises
Ice pack on problem area
Once the location of the damage has been identified, it is necessary to begin simple manipulations. Of course, they will depend on the nature of the damage. If there are open wounds, first of all they must be washed and treated with antiseptic.
Suitable products for this include hydrogen peroxide, Chlorhexidine, Miramistin, Bepanten. Before applying the antiseptic, the wound can be washed with soapy water. The bleeding area must be covered with a clean cloth or, if available, a sterile bandage.
Then apply cold to the affected area through the cloth. This can be an ice pack or a regular towel soaked in cold water, which is applied through a waterproof film.
Elements of treatment and means used
Immediately after injury, first aid must be provided. Usually, all bruises of the upper and lower jaw can be treated quite well without medical intervention. However, in case of severe lesions, it is still worth contacting specialists for examination.
Table No. 1. Painkillers:
Name of the drug Active substance Additional action Directions for use
Ketonal
Ketoprofen. Anti-inflammatory and decongestant. Apply a thin layer to the skin 2-3 times a day.
Fastum gel
Ketoprofen. Anti-inflammatory, improves blood circulation. Rub in the gel until completely dry 2 times a day.
Dolgit
Ibuprofen. Relieves swelling and inflammation. Apply with gentle massage movements, 3 times a day, up to 3 weeks.
Finalgon
Nonivamide, Nicoboxil. Improves blood circulation, recommended on the 3rd day after injury. After application, it is recommended to cover the affected area with a warm cloth.
Indomethacin
Indomethacin. Anti-inflammatory. Children apply no more than 1 cm of gel, adults no more than 15 cm, 2 times a day.
First of all, cold is applied to the lesion. Low temperatures will help not only relieve swelling and stop bruising, but also provide partial pain relief.
For the most effective elimination of unpleasant sensations, it is necessary to take analgesics internally or apply special ointments externally. Modern drugs are available in the form of gels. They are easy to use, absorb quickly and do not stain clothes.
It is good to use products that contain Heparin. It helps to quickly get rid of infiltration and eliminate the phenomenon of swelling. Heparin-based drugs should not be used by persons with bleeding disorders.
If the gel contains horse chestnut extract, it is contraindicated for people suffering from kidney disease and pregnant women. To prevent side effects from using the gel or ointment, the attached instructions should be studied in any case.
Table No. 2. Coolants:
Name of the drug Active substance Additional action Directions for use
Ben-Gay
Menthol, methyl salicylate. Painkillers, anti-inflammatory Apply in large quantities 3-4 times a day.
Flexall
Aloe vera extract, menthol, camphor, vitamin E. Quickly relieves pain and has an anti-inflammatory effect. Apply in a thin layer without rubbing.
Bystrum gel
Ketoprofen, Trometamol, essential oils. Decongestant and painkillers. Rub in with smooth movements until completely dry.
Reparil gel
Escin, salicylic acid. Decongestant, anticonvulsant, painkillers. Apply with light massage movements, 3-4 times a day, no more than 14 days.
The price of medications in the form of gels and ointments ranges from 220 rubles to 350 rubles. One package is completely enough for a course of treatment.
It is difficult to predict when a particular injury will occur. To reduce the risk of bruises and other injuries, precautions should be taken. In winter, move carefully on slippery sidewalks; in summer, when engaging in active sports, think through the possible consequences.
Introduction
Damage to soft tissues accompanies human life.
A bruise is a closed mechanical damage to soft tissues caused by short-term exposure to a damaging factor, which is not accompanied by the formation of wounds. When a bruise occurs, small vessels always rupture, followed by hemorrhage, the severity of which can vary. Damage to soft tissues, regardless of the cause that caused them, constitutes the majority of visits to primary health care institutions. Bruises usually occur when falling or hitting hard objects. In children of the first years of life, household and play injuries, bruises of the soft tissues of the face and neck predominate. At older ages, the main types of injuries are transport, sports, and street injuries [1]. Damage to superficial soft tissues is always accompanied by swelling of the injury site as a result of the skin being soaked in lymph, blood and local aseptic inflammation. The amount of swelling depends on the area of damage to the subcutaneous tissue at the site of the injury. For example, in the area of the cranial vault, due to the thin layer of subcutaneous fat, edema is insignificant, while even mild bruises of the face are accompanied by the development of pronounced edema [2]. Bleeding that continues deep into the tissue often leads to additional trauma to adjacent tissues as a result of their compression, which is accompanied by a gradual increase in pain and dysfunction. A bruise sometimes accompanies other injuries (fracture, etc.), so you should always exclude more complex injuries and evaluate the consequences of injuries [2, 3]. Soft tissue injuries are accompanied by pain of varying intensity. Thus, with bruises of large nerves and their endings, the pain is always sharp, shooting. With bruises of the torso and limbs (shoulder, thigh), tense hematomas can form, with bursting pain, sometimes with superficial numbness.
Treatment of soft tissue bruises is traditionally aimed at eliminating the above symptoms and excluding more severe pathology [4]. Currently, there are treatment standards - clinical guidelines for the provision of emergency medical care for soft tissue injuries, where a special place is given to the issues of immobilization, wound care and pain relief [5]. The administration of opioid and non-opioid analgesics is recommended in combination with antihistamines (metamizole sodium, trimeperidine, diphenhydramine). It is necessary to perform immobilization as soon as possible. Even with minor injuries, it is better to apply a tight bandage to the bruised area or immobilize with an orthosis. This will ensure peace of the bruised segment, normalize microcirculation, and reduce motor activity. Some orthotic products have a micromassage effect, which also has a beneficial effect on reparative processes. Along with this, analgesic therapy is carried out. These activities must be performed within the first 3 days. Then it is possible to use warming procedures and physiotherapeutic measures. Local therapy with ointments and gels can be used from the 1st day if they do not have a warming effect and do not increase vascular permeability.
Soft tissue bruises, and therefore pain, are inherently interconnected. Pain is a unique psychophysiological state of a person that occurs as a result of exposure to super-strong or destructive stimuli and causes functional or organic disorders in the body. Moreover, pain is subjective in nature, its perception is based on personal experience associated with damage in the early period of life. Its perception is determined not only by the source of pain, but also by such, at first glance, non-obvious factors as the psychophysical and emotional characteristics of the individual, his cultural level, family training and many others. Most often it is characterized as a psychophysical state of a person, which is a characteristic reaction to various organic and functional disorders caused by the action of various stimuli. Pain is both a physical sensation and an emotional reaction to it. Pain expert Margot McCaffrey's pithy definition is "anything that a patient says hurts them."
The functioning of the nociceptive system is mediated by neurochemical mechanisms realized by endogenous peptides and mediators, including histamine, substance P, kinins, prostaglandins, leukotrienes, potassium and hydrogen ions [4–6]. When pain occurs, the processes of hypercoagulation and lipid peroxidation are activated, the content of proteolytic enzymes increases, which causes tissue destruction. Pain contributes to the development of tissue hypoxia, degenerative processes and disruption of microcirculation in tissues. This, in turn, increases the alteration of injured tissues [7].
Thus, pain is a complex psychophysiological phenomenon, which, both from an ethical and legal standpoint, requires treatment aimed at relieving pain [8]. Understanding the complexity of its nature, mechanisms of development and regulation allows us to take a differentiated approach to the issue of choosing analgesic therapy.
One of the most effective means of protecting peripheral nociceptors that does not cause depression of vital functions are non-steroidal anti-inflammatory drugs (NSAIDs). The modern concept of effective pain relief for bruises and other types of injuries involves a multimodal approach - influencing various parts of the pain impulse. In this regard, it is advisable to combine the administration of NSAIDs with opiates or opioids for severe pain syndrome, for example, in case of shockogenic traumatic injuries.
Nonsteroidal anti-inflammatory drugs are the drugs of choice for the treatment of mild to moderate pain. Their anti-inflammatory effect is based on inhibition of cyclooxygenase (COX). One of the representatives of NSAIDs is ketoprofen, produced in various forms (tablets, injections, external ones). The triple effect - anti-inflammatory, analgesic and antipyretic - is due to blocking the enzymes COX-1 and COX-2 and, partially, lipoxygenase, which leads to suppression of the synthesis of prostaglandins (including in the central nervous system, most likely in the hypothalamus) and thromboxanes. Ketoprofen stabilizes in vitro
and
in vivo
liposomal membranes, at high concentrations
in vitro
suppresses the synthesis of bradykinin and leukotrienes. It does not have a negative effect on the condition of articular cartilage [9].
From the point of view of the ratio of anti-inflammatory and analgesic activity, ketoprofen seems to be the optimal molecule. Thus, according to an experimental study using a model of toothache, ketoprofen has the most pronounced anti-inflammatory effect compared to many NSAIDs, while the clinical effectiveness indicator (total reduction in pain after 4 hours) is the greatest for ketoprofen [10]. It is important to note that these experimental data were confirmed by data from a meta-analysis of 13 RCTs: with regard to the relief of moderate and severe pain, ketoprofen is significantly superior to diclofenac and ibuprofen [11].
Despite the fact that ketoprofen is a “traditional” non-selective NSAID, it is less capable of causing NSAID-associated gastrointestinal and cardiovascular complications - data from a Finnish population-based study assessing the causes of 9191 events in the upper gastrointestinal tract ( including cases of bleeding, ulcers and perforation). According to the results obtained, the likelihood of developing serious gastrointestinal complications when using ketoprofen was lower compared to other NSAIDs, such as diclofenac. Ketoprofen demonstrated a similar or even lower risk of developing gastrointestinal pathology than a number of selective NSAIDs [9–11]. The minimal negative effect of ketoprofen on the cardiovascular system has been demonstrated in a number of large-scale epidemiological studies.
In a study of the analgesic effect of ketoprofen in the acute period of injury in victims with various skeletal injuries, the onset of analgesic effect was noted within 12.2 ± 2.6 minutes after intramuscular application of 100 mg of ketoprofen. The use of 200 mg reduced the wait for the development of analgesia to 8.2±2.2 minutes. At the same time, in patients with severe musculoskeletal injury, ketonal was used at a dose of 200 mg in combination with intravenous tramadol (100 mg), and the analgesic effect was realized in 5.8 ± 0.9 minutes, which was faster compared to tramadol monotherapy at the same dosage (6.0±1.2 min) [12].
Purpose of the study:
determine the effectiveness of analgesic therapy for bruises of the upper and lower extremities.
Folk remedies
There are several proven, simple and at the same time effective ways to have the positive effects of alternative medicine. They are indispensable products for pregnant women, children, as well as people who have a severe allergic reaction to medications. You can make a choice based on personal preferences or doctor’s recommendations.
Treatment at home for bruises can be carried out using the following means:
- Table salt solution. Compresses are prepared from it, which are used for any complexity of bruises. To prepare, a tablespoon of salt is dissolved in 150 ml of boiled water. Then take a sterile bandage, soak it in the solution and apply it to the problem area. The compress is covered with a thick cloth on top. The gauze pad with salt can be left overnight.
- Grated potatoes. The tubers should be washed and cleaned first. Grate one tuber on a coarse grater, place in linen cloth and wrap several times. After applying the bruise, cover the top with a thick towel. Compressor exposure time is 30-40 minutes. For best results, make 3-4 applications in a row.
- Cabbage leaf. Before applying it, you should knead it a little or make cuts on it to let the juice out. The sheet is applied to the sore spot 2-4 times a day until it dries completely.
- Onion and garlic. The two ingredients are ground and mixed together. The resulting slurry is added with half a tablespoon of salt; it is recommended to wrap the mixture in gauze and place it in the area of the bruise.
- Beetroot and liquid honey. Finely grated root vegetables are mixed with a tablespoon of natural honey. The procedure is carried out 1-2 times a day for 2 hours.
- Laundry soap. This remedy helps reduce the pain response. The soap is grated and mixed with raw chicken yolk. I apply a compress every half hour up to 6-8 times a day. You can also rub a damp cloth with laundry soap and apply an application to the bruised area.
- Apple vinegar. This is one of the most effective remedies. To prepare the solution, you need to take 2 teaspoons of vinegar and dilute it in 1 liter. water. Soak a clean cloth in the solution and apply 3-4 times a day for half an hour.
Popular folk remedies for bruises
The video in this article shows how to properly apply a warm and cold compress for bruises.
Results and discussion
The average age of the patients was 44.7 years. The ratio of men to women was 1:1.
As can be seen in Figure 1, with bruises of the upper limb, ketoprofen tablets began to show its activity already at the 10th minute, with bruises of the lower limb - somewhat later, at the 20th minute. The use of the injection form (Fig. 2) provided a pronounced analgesic effect already at the 5th minute. Both tablet and injection forms of ketoprofen demonstrated an advantage over diclofenac. By 3–4 days, in all cases it was possible to achieve complete pain relief. The duration of the analgesic effect of the drugs was not studied due to the large psycho-emotional component and the small sample of patients. A peculiarity of the assessment of pain syndrome at the initial visit was that patients with a shoulder injury rated pain 2–3 points higher than patients with a hip injury (6–8 points).
I would like to note that, despite the effectiveness of the injection form of the drug, the tablet form remained the form of choice for patients with arm injuries, according to the survey. In patients with leg injuries, the injection form was preferred. Here we have to state a paradox: with a more severe pain syndrome due to a bruise of the upper limb, a more effective injection form is used much less frequently than in patients with damage to the lower limb.