What are furcation lesions?
Furcation damage is the process of loss of bone tissue in the area of branching of the roots of the tooth. Typically, bone loss is a consequence of periodontal disease. Periodontium is a complex of tissues that surround and hold the tooth in the bone.
Almost all periodontal diseases are caused by the accumulation of plaque (plaque). Thus, high-quality and regular removal of plaque and stones is a mandatory, integral part of the course of treatment of periodontal diseases. As periodontal disease progresses, plaque and tartar begin to form on the root surface. In this case, the patient will no longer be able to independently remove microbial contamination. When the lesion reaches the furcation, self-cleaning becomes impossible.
Assessing furcation involvement The first step is to determine the presence and extent of furcation involvement. For this purpose, special (periodontal) curved probes are used, which are inserted by the doctor into the furcation area. The second step is to conduct an x-ray examination, which will help to visualize the existing defect.
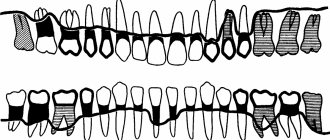
Classification of furcations depending on the severity of the lesion
Normal state of tooth furcation
Class 1 (initial changes) - on an x-ray, the affected area can be visualized as a groove
Class 2 (moderate damage) – the depth of the bone defect is 1-2 mm
Grade 3 - significant bone loss in the furcation area
Treatment Treatment of furcation lesions is a complex and painstaking task for both the doctor and the patient. Cleansing the furcation area is usually carried out using special scalers and currets. Drug therapy consists of taking or topical application of antimicrobial and antibacterial drugs. There are also surgical techniques for the treatment of furcation defects, which have two main goals: to make the furcation area more accessible for cleansing or to regenerate lost bone and soft tissue. The possibility of regeneration largely depends on the severity of the lesion; with significant defects, this procedure may not give positive results.
Prognosis The future of teeth with furcation defects of bone tissue is largely determined by how well the patient maintains oral hygiene and how regularly he visits the hygienist.
based on materials from the site www.deardoctor.com
Furcation defects: modern approaches to treatment
Several studies have assessed the long-term prognosis of multirooted teeth with furcation involvement that were treated according to the principles described in this chapter. In a 5-year study, Hamp et al (1975) observed the outcome of 175 teeth with varying degrees of furcation involvement in 100 patients. Of the 175 teeth, 32 (18%) were treated with SRP alone, 49 (28%) were treated, in addition to SRP, with furcation repair, which included odonto- and/or osteoplasty. Eighty-seven teeth (50%) underwent root resection and 17 teeth (4%) underwent tunnel preparation. Upon completion of the active phase of therapy, patients were included in a maintenance therapy program, which included a follow-up visit every 3-6 months. The results of assessing plaque and gingivitis immediately after treatment and once a year during treatment showed that the patients' oral hygiene was of high quality. None of the treated teeth were removed during the 5-year study period. During the observation period, carious lesions were found on 12 surfaces of 32 teeth treated with SRP, three surfaces of 49 teeth undergoing furcation grafting, five surfaces of 78 root resection teeth, and four surfaces of seven tunnel teeth. The results of this study were largely confirmed in another study (Hamp et al. 1992). In this 7-year study, the authors followed 100 patients with 182 teeth with furcation lesions. Of the 182 teeth with furcation involvement, 57 were treated with SRP alone, 101 were treated with furcation repair, and 24 were treated with root resection or hemisection. Tunnel preparation was not performed. After the active phase of therapy, patients were included in a thorough maintenance program, including follow-up visits every 3-6 months. In the study, >85% of furcations treated with SRP alone or in combination with furcation repair remained stable or showed signs of improvement. Only one tooth and one mesial root of a mandibular molar were removed among the teeth after root resection or hemisection. Carnevale et al (1998), in a 10-year prospective controlled clinical trial, demonstrated a 93% survival rate for resected furcation teeth and a 99% survival rate for non-furcation teeth. More recently, Svärdström (2001) presented the results of a retrospective analysis of factors influencing treatment decision-making for 1313 molars with furcation involvement in 222 patients, and treatment outcome was obtained after 8–12 years (mean 9.5 years) of regular follow-up sick. The treatment options included were tooth extraction, root separation/resection, and tooth maintenance with non-surgical/surgical SRP with or without furcation repair. Of the 13 molars with furcation involvement, 366 (28%) were extracted during the active phase of therapy. The decision to extract a tooth was primarily influenced by factors such as tooth mobility, tooth position, absence of occlusal antagonism, degree of furcation involvement, probing depth, and amount of periodontal support remaining. Of the 685 molars with furcation involvement and 160 patients who were available for follow-up 8 to 12 years after treatment, 47 teeth underwent root resection and 638 teeth were considered suitable for restoration after nonsurgical or conservative surgical therapy. The degree of furcation involvement (classes II and III) has been found to have the greatest influence on the decision to perform root resection. Tooth position, probing depth, and tooth mobility were also factors of statistical significance. The author indicated that other factors such as endodontic conditions, root anatomy, and overall treatment strategy may also influence the choice of treatment modality. The long-term outcome of the treatment plan adopted for molar furcation lesions showed favorable survival for both resective (89%) and non-resective (96%) treatment options in patients enrolled in an appropriate supportive care program. Of the 47 rooted/resected teeth, only five (11%) were extracted during the 9.5-year follow-up period. Of the 638 molars initially considered suitable for nonresective treatment, 21 (3.5%) were extracted and three were resected. Recently, Huynh-Ba et al (2009) published a systematic review of articles reporting the results of various treatments for periodontitis in multirooted teeth with varying degrees of furcation involvement. The authors selected 22 publications that could determine both survival and complication rates in teeth with furcation lesions after a mean follow-up of at least 5 years after active periodontal therapy. Treatment modalities described ranged from nonsurgical and surgical debridement, furcation tunnel preparation, hemisection, root resection, and regenerative procedures. The following dental survival rates were reported: ● Non-surgical furcation therapy: 90.7-100% at the end of a follow-up period of 5-12 years. The survival rate of teeth in molars with class I furcation defects (74% of analyzed teeth at the beginning of the study) was 99-100%, in molars with class II furcation defects - 95%, and in class III furcation defects - 25%. ● Surgical furcation therapy (ie, flap surgery with or without bone resection, gingivectomy/gingivoplasty, but not including furcation odontoplasty): 43.1–96% at follow-up of 5–53 years. ● Tunnel preparation: 42.9-92.9% after 5-8 years of follow-up. Carious lesions were reported as a complication. ● Surgical resection therapy (ie, root resection or root separation): 62-100% after a follow-up period of 5-13 years. Complications were reported to be mainly root fractures and failed endodontic treatment. ● Surgical regenerative therapy (ie, GTR, bone grafts): 62-100% after 5-12 years. However, despite a horizontal decrease in furcation depth in most cases after treatment, complete closure of the furcation was not a consistent finding, especially in severe lesions in the mandibular and maxillary molars.
Classification of furcation defects[edit]
Because of its importance in the assessment of periodontal disease, a number of classification methods have been developed to measure and record the extent of bifurcation involvement; most measures are based on horizontal measurements of attachment loss at the bifurcation.
In 1953, Irving Glickman
divided furcation lesions into the following four classes:[3]
- Grade I
is an initial furcation lesion with an associated periodontal pocket remaining coronal to the alveolar bone. The pocket primarily affects soft tissue. Early bone loss may have occurred, but this is rarely evident radiographically. - Grade II
- There is some horizontal component of bone loss between the roots that results in the area of interest, but there is still enough bone attached to the tooth (at the dome of the furcation) that multiple areas of furcal bone loss, if present, are not associated. - Grade III
- The bone is no longer attached to the fork of the tooth, resulting in a through-tunnel. However, due to the angle in this tunnel, the fork cannot be fully explored; if the combined measurements from different sides are equal to or greater than the width of the tooth, a grade III defect can be assumed. In early grade III lesions, soft tissue may still obstruct the furcation, making detection difficult. - Grade IV
- Essentially a grade III lesion, grade IV describes a penetrating lesion that has undergone sufficient bone loss to make it fully probing.
In 2000, Fedi et al.
modified the Glickman classification to include two grades of grade II furcation defect:[4]
- Grade II, Grade I
- exists when furcal bone loss has a vertical component of >1 to <3. - Grade II, Grade II
—exists when furcal bone loss has a vertical component >3 mm but is still not transmitted through.
In 1975, Sven-Erik Hamp
together with Lind and Sture Nyman classified fork defects according to their depth.
- Class I
- Furcation defect less than 3 mm deep. - Class II
- The furcation defect is at least 3 mm deep (and thus overall greater than half the buccolingual thickness of the tooth) but is not through (i.e. there is still some interradicular bone attached to the corner of the tooth). Thus, the bifurcation defect represents a dead end. - Class III
- Furcation defect spanning the entire width of the tooth such that no bone is attached to the furcation angle. [4]
Root trunk length[edit]
The distance between the cemento-enamel junction (CEJ) and the entrance to the fork is called the root length
. This distance plays an important role in furcation defects because the deeper the entrance to the furcation is within the bone, the more bone loss is required before it becomes exposed.
For mandibular first molars, the average root shaft length is 3 mm on the buccal side and 4 mm on the lingual side. [2] The length of the root shaft of the mandibular second and third molars is the same or slightly longer than that of the first molars, although the roots may be fused.
For maxillary first molars, the average root shaft length is 3-4 mm on the buccal side, 4-5 mm on the mesial side and 5-6 mm on the distal side. [2] As with the mandibular molars, the root shaft length of the maxillary second and third molars is either the same as or slightly longer than that of the first molars, although the roots may be fused.
For maxillary first premolars, bifurcation occurs in 40% of cases, and the average root shaft length is 8 mm both mesially and distally. [2]