Classification of jaw atrophy and bone tissue phenotypes
Depending on the position of the jaw, there are two groups that characterize the atrophic state of the upper and lower jaws:
- According to Schroeder for the top row. There are three types of upper jaws with missing teeth, resulting in thinning bone tissue:
- The jaw tubercles are very noticeable. These gaps can be filled with prosthetic implants because the physical abnormalities are not noticeable. The palate is deep, and the bend of the mucosa is quite large.
- The alveolar processes are not clearly defined. The depth of the sky is average. Prosthetics are possible, but their fixation may deteriorate after muscle tissue overstrain.
- The bone at the base of the jaw is seriously destroyed. The ridges and tubercles of the alveoli are smooth, and the palate is transformed into a flat shape. The fold of the mucous membrane becomes at the level of the palate and does not hold its shape well. As a result of pathology, prosthetic structures cannot be secured.
- According to Keller for the bottom row:
- The alveolar elements are slightly smoothed, but are visible throughout the entire jaw. At the beginning of the alveolar ridge, muscle tissue and a fold of mucous membrane are attached. Installation of the prosthesis is not difficult.
- The ridge becomes noticeable and takes on a sharper shape. The muscles are attached to the crest. In most cases, the implant causes discomfort and pain.
- It is often observed in people who have undergone early removal of lateral teeth. The alveoli around the molars and premolars become thinner. In the central part, the bone tissue does not lose volume. Creating artificial teeth is possible, but there is a possibility of the implant slipping when chewing.
- In the area of the frontal incisors, a pronounced atrophic process is observed, while the lateral dentition remains preserved. Fixation of the prosthesis cannot be done, because the likelihood of its displacement increases.
Examples of work “Before” and “After”
Basal implantology with immediate loading
Case: The patient complained of an uncomfortable removable denture.
Restoration of all teeth on the upper and lower jaw - basal implantation
Case: partial absence of teeth on the upper and lower jaws, complicated by a severe form of periodontitis (tooth mobility).
Restoration of all teeth in 4 days - basal implantation
Case: Absence of all healthy teeth on both jaws.
Restoration of all teeth using basal implantation method (March 2012)
Case: partial adentia, exposed roots of natural teeth, periodontitis, increased tooth mobility, severe atrophy of bone tissue in some places beyond the possible norms for classical dental implantation.
Implantation for jaw bone atrophy
Several techniques are used to quickly restore the dentition. For example, installation of bridges or removable dentures. However, these methods cannot restore the required load on the bone, since the gums or healthy teeth are loaded.
Implantation helps relieve pressure on the bone and prevent further thinning.
In advanced cases, when the atrophy of the jaw bone tissue is significant, restoration of the bone structure is used before implantation. Various techniques are used, for example, sinus lifting, separation of the alveolar process, and the introduction of artificial tissue. Six months after the operation, implants are inserted. As a result, bone density and volume are preserved.
Implantation with immediate loading is considered a new technique. Special materials are installed not in the alveolar process, but in the basal part of the jaw. Thanks to this, the bone is immediately loaded, and the metabolism is not disrupted. Suitable only if three or more teeth in a row are missing.
Implantation with immediate loading: advantages
- no bone tissue augmentation is required: the size of basal implants is selected individually, they can also be installed at a certain angle, thanks to which they can be securely fixed in any volume of bone tissue
- individual approach: to restore teeth, the doctor selects various structures in length, shape and design - in this way the doctor is able to evenly distribute the load between the implants and reduce the time of their healing
- rapid restoration of teeth: ROOTT basal implants, developed by the Swiss company TRATE AG, allow you to proceed to prosthetics within 3-5 days after their fixation; as a result, the entire treatment process takes no more than a week. This type of implant has the shape of a root, but with a wider thread and a special smooth coating that prevents the accumulation of microbes. ROOTT basal implants are installed vertically either into the socket of a newly extracted tooth, or are screwed in in a minimally invasive manner with compression of the bone tissue during installation. Thus, the operation is performed without incisions and stitches, as well as loss of the patient’s own tissue when forming a bed for the implant;
- restoration of bone tissue: thanks to the immediate chewing load, implants allow you to restore blood circulation in bone tissue and improve the regeneration process
- minimal number of contraindications: patients are rarely denied installation of basal implants for medical reasons; in addition, in many cases, basal implantation is possible even if contraindications have been identified for the classical method
- resistance to infections: implants are installed in the bicortical, that is, deep layers of bone, due to which the likelihood of penetration by bacteria and microbes is minimal, and therefore the risk of implant rejection is reduced
- guaranteed result: rapid restoration of bone tissue ensures implant healing in a short time and, as a result, excellent aesthetic, functional results and complete restoration of teeth within a couple of months after surgery.
In order to prevent bone tissue atrophy, it is necessary to attend to the issue of prosthetics immediately after tooth extraction. However, preference should be given to dental implantation, as the most natural way to restore lost teeth.
Types and degrees of jaw bone atrophy
Deformation of the jaw bone develops with different intensity:
- I degree. At the beginning of the disease, it is eliminated by prosthetics. The implant performs its function, the blood supply is not disrupted.
- II degree. The clinical picture is intensifying. The mucous membrane of the jaw begins to shrink. Dental prosthetics are possible, but additional treatment is required before this can be done.
- III degree. The contour of the bone tissue is smoothed both on the inside of the mouth and on the side of the chin.
When selecting a treatment method, this characteristic of the development of pathology should be taken into account. Bone tissue decreases not only in height, but also in width. The bone becomes short and thin.
Common methods of osteoplastic surgery
As we have already found out, there will be a need to build up bone only in cases where the patient is indicated for a two-stage implantation technique, that is, you are missing one or more teeth that were lost more than a year ago. In all other cases, approaches are applicable that allow one to abandon procedures that are so traumatic and require long-term rehabilitation.
So, if before implantation you were informed about the need to build up the bone due to atrophy, then the options may be as follows.
Sinus lift
Suitable only when it is necessary to restore the teeth of the upper jaw. Doctors distinguish open sinus lifting in dentistry and closed one. What it is? These are procedures that involve changing the height of the jaw bone, so as not to subsequently injure the maxillary sinuses and have the necessary volume of tissue for reliable fixation of the implant.
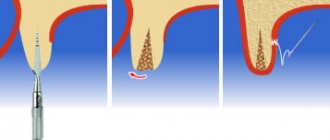
The photo shows a diagram of the sinus lift operation
What is a closed sinus lift in dentistry? A closed procedure is performed if it is necessary to increase a small amount of tissue. In some clinical cases, it allows the simultaneous installation of an implant, which 4-6 months after surgery (after complete engraftment) can be loaded with a fixed prosthesis.
Open surgery is required if the bone has lost significant height. The operation is quite traumatic, so it is impossible to install an implant at the same time. First you will have to undergo rehabilitation, which will take up to 6-8 months. And only after this, if there are no complications, you can begin installing artificial roots.
The photo shows a diagram of an open sinus lift
Autotransplantation
Expensive and traumatic procedure. It involves not one, but several surgical interventions at once. First, donor material is taken from the patient himself (for example, from the chin area), which is then planted in the place where atrophy is present. Why so many complex manipulations? It is believed that one’s own material takes root better and faster and is not rejected by the body. However, after the procedure there will be a long rehabilitation period, and it will be possible to begin installing implants only after complete engraftment of the tissues.
In this operation, the patient's own tissue is transplanted
Guided bone regeneration
The best option among those presented, as it is less traumatic and allows for the simultaneous installation of implants. The operation uses artificial bone chips and synthetic materials, as well as self-absorbing membranes that do not cause allergic reactions.
Artificial bone chips are used for the operation.
Jaw bone atrophy with age
One of the factors influencing the defect is age-related changes. As a rule, in patients over 60 years of age, atrophy is a common process. This is explained by the fact that the lack of minerals and cell nutrition affects metabolism and teeth fall out. The blood supply to bone tissue is disrupted and the required amount of oxygen is not supplied. This causes a change in pressure on the bone.
Comments
Can I take any vitamins to prevent bone atrophy?
Marianna (04.10.2020 at 14:36) Reply to comment
- Dear Marianna, taking vitamins as an independent measure will not solve the problem. However, vitamins, in particular vit. D, help improve the quality and structure of bone tissue. This vitamin is often prescribed in postoperative periods, for example, after tooth extraction or after installation of implants, also after bone tissue augmentation.
Editorial staff of the portal UltraSmile.ru (07.10.2020 at 09:24) Reply to comment
I want to install mini-implants, because... they have a very good price. Will they save you from atrophy?
Makarchenko (10/29/2020 at 6:27 pm) Reply to comment
- No, mini-implants are smaller in size and diameter, they are not able to properly distribute the chewing load from the prosthesis, and accordingly, the bone under them will still atrophy. Due to the design features of mini-implants, only removable dentures can be installed on them.
Editorial staff of the portal UltraSmile.ru (03.11.2020 at 09:07) Reply to comment
Write your comment Cancel reply
Jaw bone atrophy after tooth extraction
The most common cause of the disease is the loss of a tooth or dentition. A few months after extraction, if prosthetics are untimely, the process of reducing the jawbone begins due to pressure on the alveolar process. Within a year, the deformation can reach its maximum.
The consequences of bone tissue deficiency are expressed in the deterioration of speech, changes in the proportions of the face and its shape, and the appearance of severe wrinkles in the mouth area. At an advanced stage, patients experience displacement of the dentition, loss of opposite and/or adjacent teeth. Because of this, the likelihood of implantation failure increases.
How does the violation occur?
Again, I wrote about this. I recommend reading it>>.
The body perceives any surgical operation, including tooth extraction, as an injury and reacts to it with an appropriate reaction, inflammation.
Inflammation is a complex pathophysiological process consisting of several smoothly flowing stages:
During inflammation, a number of biologically active substances (BAS) are released, triggering phagocytosis, in which osteoclasts and other macrophages participate. They destroy everything that they consider damaged (and everything damaged is marked in advance with special compounds, antibodies).
Thus, the process of osteolysis - osteoclasts eat bone tissue, it decreases in volume. And everything would be very sad if osteoclasts did not die from their gluttony - when they die, they secrete a whole series of mediators, the so-called. Bone Morphogenetic Proteins (BMP) or, in foreign languages, BMP (Bone Morphogenetic Proteins), which activate the reproduction and differentiation of fibroblasts and osteoblasts. In other words, they trigger osteogenesis, the growth of new bone:
And here we need to make a couple of important notes:
– the main biologically active substances that trigger phagocytosis (cytokine proteins, etc.) are released during the alterative stage of inflammation, which is known for its violent symptoms. Yes, friends, swelling, pain, increased temperature of the injured area - all this happens in the alteration phase.
– yes, we are all afraid of pronounced post-operative (read, “inflammatory”) symptoms and do a lot to ensure that they are as mild as possible. But an interesting fact is that a weakly expressed alteration stage will not provide the required amount of biologically active substances to trigger osteoclasts, and they, in turn, to regenerate bone tissue. Thus, there is a direct positive relationship between the symptoms of the postoperative inflammatory process and subsequent regeneration: the more pronounced the alterative stage of inflammation, the more factors that control osteogenesis are released.
In fact, the post-traumatic inflammatory process throws our osteolysis-osteogenesis equation out of balance - due to the increased activity of bone-eating cells, osteolysis outweighs:
Fortunately, this process does not last long. Gradually, all processes are balanced again, the rate and degree of osteolysis is almost equal to the degree and rate of osteogenesis.
And the process of atrophy slows down. If we tie it to time and draw a graph, we get the following:
Simply put, the greatest amount of bone loss occurs in the first 4-8 weeks after tooth extraction. Then, the process slows down - and, taking a period of time from 18 to 24 months after removal, we are surprised to note that the linear dimensions of the bone practically do not change:
But let’s return to bone tissue biotypes.
If there is a relationship between the biotype of the alveolar bone and its regenerative capabilities (osteogenesis), then, obviously, there is a relationship between the biotype and the rate of bone atrophy. And you have observed this many times - let’s say, if we see a very strongly atrophied alveolar ridge, then, as a rule, it is of the D1-D2 biotype, and if the shape and volume of the jaw bone after the loss of teeth practically does not decrease over a long period of time, then by 146% D3-D4.
And this is easy to explain, knowing that the bone tissue of the D3-D4 biotype is better supplied with blood, there are more osteoblasts in it, and metabolic processes in it are more intense. Significant atrophy of such an alveolar ridge that requires osteoplasty occurs rarely and, as a rule, only in cases of very, very, very traumatic tooth extraction, or against the background of a chronic inflammatory process, when osteoclasts and other macrophages are active for a very, very, very long period of time .
General overview
Atrophy is a pathological process characterized by a reduction in volume and a decrease in bone density. Such situations arise for various reasons, but the final result is identical - the insufficiency of the structure causes changes in the structure of the jaw region, and limits the possibility of its restoration by implanting artificial roots.