Periodontal disease is a set of pathological processes that spread to the tissues surrounding the teeth and holding them in the alveoli. According to statistics, pathologies belonging to this group are diagnosed in 90% of the adult population. Moreover, most often diseases of this type are detected in men and women aged 37-45 years.
In the absence of timely and competent treatment, periodontal diseases can cause loosening and premature tooth loss, the appearance of foci of chronic infection in the oral cavity, deterioration of the body’s immune status and the development of other complications. That is why modern dentists pay increased attention to the development of methods and means for treating pathologies belonging to this group.
Structure and functions of periodontium
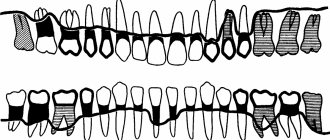
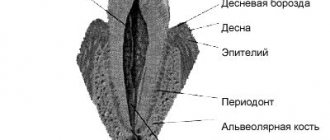
Periodontium is usually called a complex of tissues that includes:
- alveolar processes (areas of the jaw that bear the dentition);
- gums (mucous membranes covering the alveolar processes);
- periodontium (tissues consisting of protein fibers and located in the space between the alveolar plate and the cement of the tooth root);
- cement (special bone tissue covering the roots and necks of teeth).
In the human body, the periodontium performs the following functions:
- shock-absorbing (evenly distributes the load on the jaws);
- supporting-retaining (provides strong fixation of the tooth in the alveolar socket);
- trophic (contains an extensive network of lymphatic and blood vessels, a huge number of nerve receptors);
- barrier (protective) and others.
Preserving periodontal tissue in a healthy state is the key to long-term and proper functioning of the masticatory apparatus.
Causes of periodontal disease development
Factors that increase the likelihood of developing periodontal disease are:
- heredity;
- hypovitaminosis;
- failure to comply with hygiene requirements;
- presence of dental plaque;
- dental anomalies (bite disorders and others);
- somatic diseases (malfunctions of the nervous system, gastrointestinal diseases, diabetes mellitus, cardiac and endocrine disorders);
- smoking;
- weakened immune system;
- non-compliance with drinking regime;
- habit of breathing through the mouth;
- the presence in the oral cavity of low-quality fillings, orthodontic or orthopedic structures incorrectly installed in dentistry.
In addition, the risk of disease directly depends on the place of residence, lifestyle, characteristics of professional activity and dietary habits of patients.
Gingivitis
Gingivitis is an inflammatory disease of the marginal gums, while the supporting structures of the tooth are not affected.
There are several types of gingivitis:
- Catarrhal. It manifests itself as mild bleeding and swelling of the gums, itching.
- Hypertrophic. Characterized by bad breath and severe bleeding.
- Ulcerative-necrotic. Ulcers appear on the gums, and a gray coating appears on the teeth. This pathology is characterized by severe pain and putrid odor from the mouth.
Gingivitis can be acute or chronic, affecting the entire gum or the area of 1 to 3 teeth.
The causes of the disease may be:
- Poor dental hygiene, accumulation of soft plaque, which promotes the growth of bacteria.
- Injury from too hard foods or a hard toothbrush.
- Poorly installed crown or filling.
- Disturbances in the functioning of the heart.
- Hormonal disbalance.
- Diseases of the gastrointestinal tract.
- Avitaminosis.
- Decreased immunity.
- Chronic poisoning with iodine, lead, mercury, aluminum.
- Blood diseases.
For gingivitis, the dentist removes dental deposits, treats the gums with an antiseptic, applies applications with medications, prescribes anti-inflammatory drugs, a vitamin complex, selects a toothpaste, brush, and mouthwash.
Periodontitis
Periodontitis is an inflammation of the periodontal tissue and ligaments, often a consequence of untreated gingivitis. In severe cases, it affects bone tissue.
Symptoms of periodontitis include:
- the formation of hard tartar, they can secrete pus;
- severe pain;
- tooth displacement;
- exposed dental necks;
- pain when pressing on mobile teeth;
- holes between teeth and gums;
- the occurrence of flux when an infection gets into an inflamed tooth pocket.
The development of periodontitis is promoted by hypertonicity of the masticatory muscles, crowded teeth, high frenulum attachment, traumatic bite, blood diseases, diabetes mellitus, chronic pathologies of internal organs, and immunodeficiency.
There are three forms of periodontitis according to the severity of inflammation:
- Easy. There is hyperemia of the edge of the gums - overcrowding of blood vessels, pain, bleeding, slight loss of bone, shallow depth of the bone pocket.
- Average. Bleeding gums can be spontaneous, teeth become loose. Brushing with a toothbrush and eating food are difficult, the pocket increases to 5 mm.
- Heavy. Teeth fall out, severe bleeding, deep bone pockets.
The approach to the treatment of periodontitis is complex and is divided into several stages:
Remove tartar every six months, as it grows quickly.
Oral hygiene. The doctor will select cleansers and rinses. Be sure to use dental floss and brushes if there are large gaps between the teeth. It is recommended to purchase an irrigator for rinsing pockets with water.
Antiseptic treatment using special gels and rinses. In advanced cases, drugs with a long-term disinfecting effect are used. These are gelatin flakes that the dentist places in the periodontal pocket. They swell and prevent bacteria from entering it. At the same time, an antiseptic is released from the scales.
Anti-inflammatory therapy: application of bandages and ointments, physiotherapy.
Prescription of vitamins, antibiotics, immunostimulants.
Surgery may be required. The dentist makes an incision in the gum and, using special instruments, removes tartar and damaged areas, and adds artificial bone tissue.
Periodontal disease
Periodontal disease is a rare pathology in which the periodontal tissue and ligaments are damaged. Teeth begin to loosen and fall out.
The occurrence of this disease is provoked by the following factors:
- alcohol abuse, smoking;
- hereditary predisposition;
- deficiency of vitamins in the body;
- vascular atherosclerosis;
- hormonal disbalance;
- diseases of internal organs;
- abnormal position of teeth, malocclusion;
- diabetes;
- elderly age.
With periodontal disease, the necks of the teeth are exposed, the mucous membranes become whitish and decrease in volume. A wedge-shaped defect may develop and increased sensitivity occurs. There is no bleeding or swelling of the gums. The teeth are well fixed in the socket; their mobility develops only with significant destruction of bone tissue.
Treatment of periodontal disease depends on the degree of development of the disease and may include:
- Professional oral hygiene.
- Elimination of malocclusion, alignment of incorrectly positioned teeth.
- Prosthetics in case of tooth loss.
- Surgical treatment aimed at restoring bone tissue.
- Periodontal massage and physiotherapy to improve blood circulation.
- The use of antibacterial agents and vitamin complexes.
Highly qualified specialists of the Formula of Health clinic will carry out all the necessary procedures to quickly rid the patient of periodontal diseases.
Treatment necessarily includes an x-ray using the latest generation Finnish digital device “Planmeca” to identify possible destruction of bone tissue.
Teeth cleaning is carried out using an Air Flow sandblasting machine, which painlessly removes plaque and tartar.
If the patient has an incorrect bite or misaligned teeth, it is recommended to wear the Damon braces system, which allows you to get good results within several months.
If a tooth is lost, it can be restored using crowns and veneers made of durable and high-quality materials in a variety of shades, ideally matching the color of the patient’s enamel.
In advanced stages of periodontal disease, surgical intervention may be necessary. Our specialists will perform an operation that allows you to completely get rid of the pathology and save your teeth.
Symptoms of periodontal disease
The first symptoms indicating the occurrence of periodontal disease are:
- tingling, itching, numbness in the gums;
- bleeding of gum tissue;
- swelling of the interdental papillae;
- thickening of the gingival margin;
- detachment of gums from dental crowns.
In the future, the clinical picture may be supplemented by:
- gradual exposure of the necks of the teeth;
- redness, hyperemia of the gums;
- formation of pathological gum pockets;
- increase in interdental spaces;
- gradual loosening of teeth.
Symptoms of tissue diseases also include increased sensitivity of dental tissues to irritants, as well as aching pain in the affected area.
Treatment of periodontal diseases
The general treatment program for periodontal diseases includes:
- removal of microbial plaque and mineralized deposits from the surface of teeth;
- caries therapy;
- preventing functional overload of certain areas of the dentition;
- rejection of bad habits;
- carrying out orthodontic treatment (if indicated);
- anti-inflammatory therapy;
- combating systemic diseases;
- the use of drugs that enhance immunity, stimulate osteogenesis and activate the adaptive and protective functions of the body;
- carrying out general hygiene measures (monitoring the regime of work, nutrition, rest, hygiene).
The treatment regimen for periodontal diseases is drawn up taking into account all manifestations of the disease and the results of a comprehensive examination of the patient. Timely seeking of professional help by a patient significantly improves the prognosis of the disease, shortens the duration of treatment and avoids the development of complications.
Classification of periodontal diseases 2022
- Periodontally healthy, gingivitis and other conditions
- Periodontitis
- Other conditions affecting the periodontium
- Peri-implant diseases and conditions
- Periodontally healthy, gingivitis and other conditions
Periodontal health is the absence of clinical signs of inflammation; it is a biological level of stability of the immune system, formed by clinically healthy gums and a state of homeostasis.
Clinical health can be achieved by therapy for gingivitis and periodontitis. Classification of clinically healthy gums:
Clinically healthy gums with intact periodontium
Clinically healthy gums with reduced periodontium:
Patients with stabilized periodontitis (successfully treated)
Patients without periodontitis (surgical lengthening, recession)
Intact periodontium refers to the absence of clinically detectable attachment and bone loss.
Predisposing and modifying factors:
- Local risk factors (predisposing)
— microbial plaque retention factors (biofilm) — dental anatomy, restoration margins
– dry mouth – decrease in the quantity and deterioration in the quality of saliva (Sjogren’s formula, medications, mouth breathing)
- Systemic risk factors (modifying factors)
— Smoking
— Metabolic factors (hyperglycemia)
— Dietary factors (vit. C)
— Pharmacological factors
— Sex hormones (puberty, pregnancy)
— Hematological conditions
| Intact periodontium | Healthy | Gingivitis |
| Loss of attachment | No | No |
| Sounding depth | ≤3mm | ≤3mm |
| Bleeding on probing | ˂10% | Yes |
| X-ray bone loss | No | No |
| Loss of periodontal tissue in non-periodontal patients (gingival recession, post-lengthening surgery) | Healthy | Gingivitis |
| Loss of attachment | Yes | Yes |
| Sounding depth | ≤3mm | ≤3mm |
| Bleeding on probing | ˂10% | Yes |
| X-ray bone loss | Possible | Possible |
| Successfully treated and stable patients with periodontitis | Healthy | Gum inflammation |
| Loss of attachment | Yes | Yes |
| Sounding depth | ≤4 mm (no areas ≥4 mm with bleeding) | ≤3mm |
| Bleeding on probing | ˂10% | Yes (˃10%) |
| X-ray bone loss | Yes | Yes |
- Periodontitis is a chronic multifactorial disease of inflammatory nature, associated with bacterial dysbiosis and characterized by progressive destruction of the tissues surrounding the tooth.
Primary categories: periodontal tissue loss, manifested clinically by attachment loss and radiographic bone loss, periodontal pocket formation, and gingival bleeding.
Patient with periodontitis: interdental loss of attachment is found in the area of 2 or more teeth, not adjacent ones. Buccal or oral attachment loss ≥3 mm with pockets of ˃3 mm found in the area of two or more teeth. The observed loss of attachment cannot be caused by causes other than periodontitis, such as trauma-induced gum damage, cervical caries, endodontic lesions, or tooth fracture.
Key elements of the classification of periodontal diseases:
- Severity - the degree of destruction of periodontal tissue
- Complexity of treatment – type of bone loss (horizontal/vertical), probing depth, furcation involvement, tooth mobility, number of teeth lost, occlusal/furcation aspects
- Extent (prevalence): number of teeth with detectable tissue destruction
- Rate of progression: direct or indirect evidence of rate of periodontal tissue destruction
- Risk factors: smoking, diabetes, general health, general compliance
Stage _
Classifies the severity and extent of existing tissue loss, including tooth loss, due to periodontitis.
Includes the level of complexity of treatment in terms of functional and aesthetic rehabilitation of the patient
Degree _
Includes the following categories: history-based rate of progression of periodontitis, risk of subsequent progression, expected outcome of treatment, and risk that the disease or its treatment may cause a negative impact on the patient's overall health.
| Severity of the disease and complexity of treatment | Stage I | Stage II | Stage III | Stage IV | |
| Evidence or risk of rapid progression, expected response to treatment, and impact on overall health | Grade A | Individual stage and degree | |||
| Grade B | |||||
| Grade C | |||||
Stages
| Stage of periodontitis | Stage I Initial periodontitis | Stage II Moderate periodontitis | Stage III Severe periodontitis with a tendency to tooth loss | Stage IV Developed severe periodontitis with severe tooth loss and a tendency towards edentia | |
| Heaviness | Interdental loss of attachment in the most severe area | 1-2 mm | 3-4 mm | ≥5 mm | ≥5 mm |
| Radiographic bone loss | Coronal third (˂15%) | Coronal third (15-33%) | Spread to the middle third of the root | Spread to the middle third of the root | |
| Tooth loss associated with periodontitis | No tooth loss associated with periodontitis | Lost ≤4 teeth due to periodontitis | Lost ≥5 teeth due to periodontitis | ||
| Complexity | Maximum probing depth ≤4 mm. Predominantly horizontal bone loss | Maximum probing depth ≤5 mm. Predominantly horizontal bone loss | In addition to the second stage: Probing depth ≥6 mm, vertical bone loss ≥3 mm, class II-III furcation involvement, severe ridge defects | In addition to Stage III: need for rehabilitation associated with secondary occlusal trauma (mobility ≥2), malocclusion, tooth movement, protrusion and formation of three, less than 10 antagonists, masticatory dysfunction, severe ridge defects | |
| Prevalence | Added to each stage as a description | Each stage is described as localized (˂30% of teeth involved), generalized, or incisor-molar type | |||
Degrees
| Grade A | Grade B | Grade C | |||
| Primary criterion | Direct evidence of progression | Long-term follow-up (for radiographic bone loss or attachment loss) | Evidence of no loss for 5 years | ˂2 mm for 5 years | ≥2 mm for 5 years |
| Indirect evidence of progression | Bone Loss Percentage | ˂0.25 | 0.25-1.0 | ˃1.0 | |
| Phenotype | A large amount of dental plaque and a small degree of destruction | Destruction corresponds to dental deposits | Destruction is disproportionate to the small amount of deposits; evidence of periods of rapid progression or early onset of disease; expected poor response to therapy | ||
| Modifying criterion | Risk factors | Smoking | I do not smoke | ˂10 cigarettes a day | ˃10 cigarettes a day |
| Diabetes | Normoglycemia/no diagnosis of diabetes | Glycated hemoglobin ≤7.0% in a patient with diabetes | Glycated hemoglobin ≥7.0% in a patient with diabetes | ||
Practical application of the classification:
Step 1: Initial assessment of the clinical case
Screening of radiographs, probing depth, lost teeth
Determine if it is initial and moderate periodontitis or severe and developed.
Step 2: Determine the degree
Determine maximum attachment loss or bone loss radiographically,
Determine whether bone loss is horizontal or vertical
Grade I or II
Tooth loss due to periodontitis
Determine the complexity of treatment (charting, furcations, occlusion\function, need for extended rehabilitation)
Grade III or IV
Step 3: Determine the stage
History\risk of progression\age
Risk factors
Medical status and systemic diseases
Response to standard therapy (scaling and root planing) and plaque control
Detailed assessment, staging
Step 4: Treatment Plan
| initial and moderate periodontitis | Periodontitis is severe and advanced |
| Grade I or II | Grade III or IV |
| Stage A,B,C | |
| Standard periodontal treatment | Comprehensive multidisciplinary treatment |