Osteomyelitis of the jaw
In surgical dentistry, osteomyelitis of the jaw is considered a common disease. Osteomyelitis of the jaw (ICD 10 code M.86) - (osteomyelitis from the Greek osteon bone + myelos bone marrow) is a severe inflammation affecting soft tissue elements, bone tissue and periosteum. It is accompanied by necrotic damage (decomposition) of the bone, which subsequently leads to its deformation. The development of the pathological process is provoked by bacteriological microorganisms that penetrate the jaw bone together with infected blood or in response to post-traumatic damage - fractures and wounds.
Osteomyelitis of the jaw (ICD code M.86) is a serious pathogenic process that, without timely treatment, can lead to complications. The risk group consists of male patients under 40 years of age. The primary and main thing is to identify the symptoms of the disease, thanks to a clear differential diagnosis. Thus, dental surgeons from the West Dental family clinic network in Yanino-1 and Vsevolozhsk will help diagnose and treat the problem at a reasonable price.
The causes and symptoms of the disease, which specialist to contact and how to treat - we will consider below in the article.
Diagnostic methods
Suspicion of the presence of a disease may appear after receiving relevant complaints from the patient and conducting a general examination. In order to establish an accurate diagnosis and fully formulate it, it is necessary to perform x-ray diagnostics.
Confirmation of the presence of osteomyelitis of the jaw bone can be early and late X-ray signs. Early radiological indicators are:
- the presence of zones of rarefaction and compaction of bone tissue, alternating with each other;
- minimal thickening of the periosteum caused by periostitis;
- lack of clarity and blurred bone pattern.
Late radiological manifestations of osteomyelitis include:
- formation of foci of destruction with the formation of sequesters 1-1.5 weeks from the onset of the disease;
- an increase in the thickness and density of bone tissue in the area of inflammation.
In difficult cases, the doctor may prescribe an MRI examination, the results of which help to more accurately detect the extent of tissue damage. Also, such diagnostics helps to visualize small lesions with purulent contents.
In addition to X-ray diagnostics, patients also undergo general clinical tests, with which the doctor can determine the activity of inflammation:
- a general blood test allows you to detect an increased content of leukocytes, an insufficient number of red blood cells, determine hemoglobin and features of the leukocyte formula, indicating the presence of an inflammatory process;
- biochemical blood test showing the presence of inflammatory markers and electrolyte disturbances.
In order to identify the causative agent of the pathology and determine the possibility of using antibacterial medications, a bacteriological examination of the contents of the fistula tracts is performed. The discharge is inoculated onto special media with further microscopy of the samples.
Causes
The main provocateur of the formation of osteomyelitis in the upper and lower jaw is considered to be pathogenic microflora - streptococci and anaerobes, present in the oral cavity of every person. They aggravate the infection, affecting the soft and hard components of the mouth. There are several ways to penetrate deeper into the pathological process:
- Missed dental caries, which destroyed the enamel with dentin and penetrated into the pulp chamber.
- Traumatization – crack, violation of the sealing material. The damage must be deep (fracture of the HF or LF) to provoke an infectious process (staphylococci).
- Chronic infection occurs in other parts of the body. Pathological microorganisms can reach the jaw through the lymph nodes or blood vessels (ENT organs).
In most patients, osteomyelitis is located on the lower jaw, since the lower units are more likely to be affected by caries or trauma. Also, people with immunodeficiency and blood diseases are at risk, because they have difficulty healing wound surfaces and the immune function of the body is weakened.
Other factors:
- smoking;
- alcohol;
- Diabetes type I and II;
- eating disorders;
- syphilitic infection;
- radiation and chemotherapy.
If you miss and do not treat acute osteomyelitis in the upper or lower jaw, then the process becomes chronic, which is more difficult to treat and leads to many complications.
Differential diagnosis
This method is used for the reason that an error at the stage of determining the diagnosis can cause the choice of the wrong treatment method and the lack of desired results during therapy. This leads to further progression of the disease and a negative impact on overall health.
Specialists perform differential diagnosis of osteomyelitis with the following diseases:
- acute form of pulpitis;
- suppuration of a dental cyst;
- purulent inflammation of soft tissues in the maxillofacial area;
- acute periodontitis;
- periostitis;
- odontogenic sinusitis in acute form.
Classification
According to the method of penetration of osteomyelitis infection on both jaws, a classification has been compiled:
- Hematogenous - pathogenic microorganisms move through the blood from other foci of infection. This feature is characteristic of secondary pathology of the upper oral part, which develops against the background of another disease (scarlet fever, diseases of the ENT organs). The bone elements of the oral apparatus are primarily affected, followed by the gingival tissue.
- Odontogenic – infection comes from a tooth, damaged pulp or root (pulpitis, periodontitis, cyst, alveolitis).
- Traumatic – advanced fractures and injuries of the maxillofacial area.
According to the symptoms, the process happens:
- spicy;
- subacute;
- chronic.
By distribution:
- local (with clear boundaries);
- vague (diffuse).
Main reasons
In most cases, osteomyelitis of the jaw develops due to pathogens entering the bone tissue. Infection can occur in the following ways:
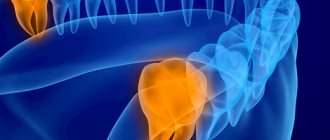
- Odontogenic pathway. In such cases, the source of the problem is a tooth with caries. At the first stage, microorganisms penetrate into the pulp tissue, and then into the bone tissue (through dental tubules or small vessels).
- Hematogenous route. Microorganisms enter the maxillofacial area through the blood from the main area of infection. There are different sources of infections - tonsillitis, furunculosis or erysipelas. Sometimes osteomyelitis develops against the background of scarlet fever, typhus or influenza.
- Traumatic path. The pathology develops as a result of infection after surgery on the jaw or fracture. Such cases are considered the rarest.
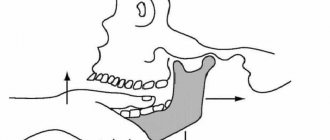
The odontogenic path is in most cases accompanied by infection of the lower jaw, but with the hematogenous path the upper jaw is usually affected. The second option involves the location of a purulent focus deep in the tissue with minimal manifestation of periostitis.
Osteomyelitis of the upper and lower jaw: symptoms
The course of the disease process is slow, and the first sign is pain in the area of the affected unit.
Then joins:
- spread of pain to nearby segments;
- swelling and redness of the gum tissue;
- periodontal damage, which causes mobility of units;
- pain in the temporal region;
- numbness of the chin;
- difficulty eating;
- speech defects;
- unpleasant odor from the mouth;
- increase in l/u;
- swelling in the problem area.
Acute osteomyelitis on the lower jaw (ICD M.86) develops very rapidly in conjunction with an increase in temperature and chills. In the absence of outflow of pus, abscesses and phlegmons form, which requires immediate surgery. This pathology in a child may be confused with mumps (mumps).
With osteomyelitis on the lower jaw (ICD-10 code M.86), in addition to damage to the alveolar part and body, the inflammatory process can spread to its branch and processes. One important feature is complications from the soft tissue elements around the NP - many muscles and tissue spaces.
After the acute period (1-2 weeks), the subacute period begins, after the formation of a fistula for the discharge of pus. The condition improves, pain decreases, and the mobility of units increases—gastrointestinal diseases develop. The subacute form becomes chronic, which lasts several months. As a result, in adults the clinical history ends with the removal of necrotic tissue, with a favorable outcome.
Acute osteomyelitis
Often, signs of this form of the disease appear unexpectedly and are manifested by general symptoms. General manifestations are not specific and indicate only serious inflammation in the body:
- a significant increase in body temperature (minimum 39 degrees);
- increased sweating;
- aching joints, feeling of weakness, headaches;
- pallor of the skin.
In addition to these manifestations, the following local symptoms appear:
- Severe continuous pain in the area where the source of infection is located. In this case, inflammation constantly develops, which leads to increased pain. As the infection spreads, the localization becomes less obvious, so the entire jaw or a certain part of the skull may ache, radiating to the corresponding eye or ear area.
- The tooth that is the source of the problem is loose. If a diffuse inflammatory process develops, nearby teeth may also become loose.
- Swelling of the soft tissues contributes to spasm of the masticatory muscles, as well as disruption of facial symmetry.
- Often, the inflammatory process affects the jaw joint, which leads to the development of arthritis, due to which the mouth is constantly in a slightly open state (it is impossible to close the jaw completely).
- Swelling and soreness of the oral mucosa and gums.
- Serious enlargement of regional lymph nodes.
Patients with the hematogenous form of the disease face the greatest difficulties, since it affects other cranial bones and internal organs. All this has a very negative impact on the future prognosis.
Traumatic osteomyelitis has a blurred clinical picture against the background of trauma. But when, a few days after a jaw fracture, the pain intensifies, the body temperature rises, health deteriorates, significant swelling of the oral mucosa and purulent discharge appears, the diagnosis is obvious.
Diagnostics
If you experience pain in the tooth area of unknown etiology, or changes in the gums, contact your dentist (he has a Leica M320 operating microscope in his arsenal), who will then refer you to a surgeon or orthopedist as necessary. At the initial stage of pathology, the doctor chooses to collect complaints and study them, visual and instrumental examination. The degree of mobility of the units and their pain, the state of the oral mucosa is determined.
It is important to distinguish the acute period of the disease from periostitis, cysts and periodontitis, so the experience of a specialist is very important.
This is a purulent infectious process, which means that general blood and urine tests will be of research significance. To type the pathogen, a tank is performed. sowing of pus.
In the chronic stage, bone changes are already noticeable, so X-rays (CT) are necessary, for which West Dental has a panoramic CBCT Pax-i3D. The image shows sequestration and the depth of the process.
Chronic osteomyelitis
The transition of the problem to a chronic form is accompanied by an improvement in the patient’s well-being. But over a long period of time, patients experience weakness, problems with appetite, problems with night rest, and pale skin.
During the examination, in the presence of a chronic form of the disease, fistulas are discovered that open in the mouth and on the skin of the face. Small amounts of pus come out of them. In addition, an increase in the size of regional lymph nodes, swelling of the mucous membranes and loose teeth are often observed.
Pain in the remission stage is minimal or absent. However, during the acute stage, the pain may intensify, and it may be difficult for the patient to determine its specific location.
Complications
If you see a doctor in time, make a diagnosis and choose the right treatment, the prognosis will be favorable.
If you ignore all the conditions, complications will arise:
- Meningitis
- Abscess of the brain and lung.
- Orbital phlegmon.
- Sinusitis.
- Vein thrombophlebitis.
- Sepsis.
- Mediastinitis.
Pathological data require immediate assistance to prevent death.
The chronic process, with its long course, affects the soft tissue and bone areas of the maxillofacial area, and is accompanied by:
- traumatization;
- changes in the TMJ;
- the formation of adhesions in the joints and scars on the masticatory muscles;
Such disorders limit chewing movements or lead to immobility.
Treatment methods
Therapy for osteomyelitis of the jaw is carried out to achieve two key goals:
- Get rid of the source of infection in the bones and nearby soft tissues as quickly as possible.
- Correct functional disorders caused by the presence of infection.
All patients are required to be hospitalized in the surgical department, which deals with problems related to the maxillofacial area. In the absence of an appropriate hospital, the patient is treated in a department that has experience in the field of dental surgery. The list of main therapeutic actions is as follows:
- An operation involving opening a purulent area in order to remove necrotic masses and ensure effective drainage.
- Improving the functioning of the immune system.
- The use of medications to relieve intoxication and inflammation.
- Use of broad-spectrum antibacterial agents.
It is very important to adhere to a complete diet with a complete list of important vitamins, minerals and nutrients (patients are prescribed a hypoallergenic diet), as well as to maintain bed rest.
Treatment
The effectiveness of therapy depends on the initial causes of the formation of the inflammatory process. Therefore, in osteomyelitis of the jaw, comprehensive treatment is important, not only by a dentist, but it is recommended to go for a consultation with doctors of medical specialties.
- Sanitation of the oral cavity with antiseptic solutions. Further spread of infection to surrounding structures is prevented. Also, necrotic soft tissue formations are eliminated.
- Anti-inflammatory drugs. Minimize intoxication of the body.
- Immobilize the fracture, and if there is a tooth in it, then remove it.
- Taking antibiotics, regardless of provoking factors.
- Intraosseous lavage may be necessary and will provide positive results. Minimizes the occurrence of complications and quickly prevents the growth of a harmful process.
- In case of a fistula, sequestrectomy is performed - necrotic areas of bone tissue are eliminated under anesthesia, taking into account the extent of the damage.
- If the teeth are mobile, they are splinted.
- After eliminating symptoms and carrying out all interventions, physical therapy, vitamins and immunomodulators are recommended.
Prevention of such pathology consists only of timely and regular visits to the dentist’s office and treatment of pathological processes in the oral cavity. Do not treat yourself at home, so as not to make it worse. Also, it is necessary to strengthen the body’s immune system, avoid injuries and not let the pathological process become chronic.
What is bone osteomyelitis?
In general surgery, bone osteomyelitis is an inflammatory process in bone tissue with a complex pathogenesis. Today, experts highlight different options for the development of the problem. But it is impossible to establish the exact reason, since each of the existing options only complements all the others. Therefore, osteomyelitis is considered a multifactorial disease. The occurrence of pathology is facilitated not only by infection in bone tissue, but also by problems in the functioning of the immune system and impaired blood flow.
When an infectious agent appears in bone tissue, the body reacts very actively to this, provoking the development of a purulent inflammatory process. In order to get rid of the infection, leukocytes move to the affected area, producing a large number of enzymes. As a result, bone structures are destroyed and cavities with liquid pus are formed. They contain sequestra or pieces of bone. In some cases, nearby soft tissues may also be affected, resulting in fistulous tracts appearing on the skin.
With proper functioning of the immune system, the inflammatory process can be limited on its own with further transition to a chronic form. However, immunodeficiency leads to the spread of infection and the formation of serious purulent complications, including sepsis. It often ends in disability or death.
Treatment of spinal infection
As a rule, in the main cases osteomyelitis is treated conservatively. Therapy is carried out with intravenous antibiotics.
Since the disease is primarily caused by the Staphyloccocus bacterium, which is highly sensitive to antibiotics, the intravenous treatment process takes about a month, and then a control two-week course begins, which is administered orally. During the entire period, the patient is prescribed bed rest.
Antibiotics for osteomyelitis
Important! If the infection is of tuberculosis etiology, the patient may take antibiotics for up to a year.
In addition to therapy, the spine is fixed for six to twelve weeks using a rigid corset, until x-rays show positive dynamics of therapy.
Consequences and rehabilitation
Osteomyelitis can have quite serious consequences in childhood:
- defects associated with bone tissue;
- jaw fractures that cause abnormal joints to form;
- the jaw is deformed;
- absence of permanent teeth, edentia;
- arthrosis, ankylosis, arthritis that relate to the joints of the temples and lower jaw;
- the jaw grows much more slowly, microgeny is noted;
- soft tissues are deformed and look like scars.
Due to the above complications, cosmetic defects may occur, but they do not have any effect on the masticatory apparatus or its functioning.
In order to restore the anatomy of the face and jaw to the maximum and ensure its normal functioning, it is necessary to take certain rehabilitation measures:
- sometimes plastic surgery is used. But this is done only after the facial bone stops growing;
- If adentia develops, then temporary dental prosthetics can be done. And as soon as the skeleton is finally formed, then permanent prosthetics are allowed;
- To improve the temporomandibular joint and its functioning, it is worth applying physiotherapeutic procedures.
All children who have suffered osteomyelitis that affected the jaw area are registered at the dispensary. They are required to visit the dentist at least 2 times a year.
OSTEOMYELITIS OF THE EXTREMITIES
- CLASSIFICATION
- NON-SPECIFIC OSTEOMYELITIS
- SPECIFIC OSTEOMYELITIS
- CAUSES
- PHOTO OF OSTEOMYELITIS
- TREATMENT OF OSTEOMYELITIS OF THE EXTREMITIES
- ACUTE HEMATOGENIC OSTEOMYELITIS
- POST-TRAUMATIC AND POST-OPERATIVE OSTEOMYELITIS
- OSTEOMYELITIS OF JOINTS AND SPINE
- HEMODIALYSIS AND DRUG ADDICTION
- SICKLE CELL ANEMIA
Content
Osteomyelitis is an inflammatory process of a purulent-necrotic nature that affects the bone tissue surrounding the periosteum and bone marrow. The causative agents of osteomyelitis, in the vast majority of cases, are staphylococci and streptococci.
Osteomyelitis that occurs for the first time is called acute. If the patient has a protracted course of the disease with exacerbations and remissions, then we are talking about a chronic course of the inflammatory process of osteomyelitis. Often, with osteomyelitis, the entire bone tissue, including the bone marrow area, is involved in the inflammation process. In the chronic process of osteomyelitis, bone sclerosis and deformation occur.
TREATMENT OF OSTEOMYELITIS OF THE EXTREMITIES
When treating osteomyelitis, mandatory hospitalization is indicated. Along with surgical treatment of the affected area, it is necessary to prescribe massive antibiotic therapy (intravenous and intramuscular administration of antibacterial drugs), powerful detoxification therapy (plasma transfusions and blood substitutes), immunostimulants, vitamin therapy, hemosorption, hyperbaric oxygenation.
ACUTE HEMATOGENIC OSTEOMYELITIS
When treating acute hematogenous osteomyelitis in children under six years of age, the following is indicated:
- Cefuroxime and Amoxicillin/Clavulanate (first-line drugs);
- Ampicillin/Sulbactam;
- Ceftriaxone and Oxacillin (alternative drugs);
For children over six years of age and adults, the following are used for the treatment of acute hematogenous osteomyelitis:
- Oxacillin and Gentamicin;
- Amoxicillin/Clavulanate (first-line drugs);
- Cefuroxime;
- Cephalozolin and Netilmicin;
- Lincomycin and Gentamicin;
- Clindamycin and Gentamicin;
- Fluoroquinolone and Rifampicin (alternative drugs);
POST-TRAUMATIC AND POST-OPERATIVE OSTEOMYELITIS
For post-traumatic and postoperative osteomyelitis, the following are prescribed:
- Ofloxacin;
- Ciprofloxacin and Lincomycin (first-line drugs);
- Cefepime;
- Vancomycin and third-fourth generation cephalosporins;
- Imipenem;
- Linezolid and Ceftriaxone;
OSTEOMYELITIS OF JOINTS AND SPINE
For osteomyelitis of the joints and spine the following are prescribed:
- Oxacillin;
- Ceftriaxone and Aminoglycosides (first-line drugs);
- Ciprofloxacin and Rifampicin (alternatives);
HEMODIALYSIS AND DRUG ADDICTION
For patients on hemodialysis and drug addicts, the following are used:
- Oxacillin and Ciprofloxacin;
- Vancomycin and Ciprofloxacin;
SICKLE CELL ANEMIA
For patients with sickle cell anemia:
- Ciprofloxacin or third generation cephalosporins (Ceftriaxone, Cefotaxime, Cefoperazone).
Causes of osteomyelitis
The main cause of osteomyelitis is pathogenic microorganisms. In most cases, the disease is caused by anaerobic bacteria and streptococci. The peculiarity of the development of the inflammatory process is that these bacteria are always in the oral cavity. The development of osteomyelitis begins when microorganisms have access to bone tissue.
Routes of infection.
- Carious cavity.
- Deep tooth trauma (crack, fracture).
- Poor quality filling.
- Fracture of the jaw bone.
The cause may be a chronic infection of the ENT organs. Bacteria travel to the jawbone and teeth through the lymphatic or circulatory system.
Osteomyelitis of the lower jaw develops predominantly, since injuries and caries of the teeth of the upper jaw occur half as often.