- Tooth extraction
- Removal of a tooth cyst
- Bone tissue augmentation
- Resection of the apex of the tooth root
- Installation of a dental implant
- Installation of a mini-implant
Patients have more chronic dental diseases than acute ones. Advanced caries, pulpitis, periodontitis lead to the fact that after a few months or years the patient is faced with a neoplasm on the root of the tooth or its acute inflammation. In this case, resection helps to save the tooth.
When should tooth resection not be performed?
- The main condition for successful root resection is the presence of sufficient jaw bone volume in the patient - at least 5 mm, otherwise there is a risk of jaw fracture.
- A tooth root resection operation will be ineffective if the patient has chronic periodontitis and/or periodontitis, as well as mobility of the diseased tooth.
Tooth root resection is contraindicated if:
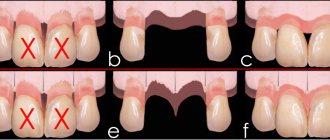
- Large cysts or granulomas, when they reach the size of a third of the tooth root or more.
- A completely destroyed dental crown, if the tooth cannot be replaced with prosthetics.
- Close proximity of the roots of healthy teeth.
- Severe mobility of the diseased tooth.
- Some common diseases, such as diabetes, blood diseases, heart diseases, immunodeficiency conditions.
Types of bone grafting
The dentist-implantologist has several methods at his disposal to effectively restore bone volume, and their choice depends on the nature of the deficiency. In this case, we mean a vertical or horizontal tissue deficiency, that is, an expansion of the narrow alveolar process or an increase in its height to install an implant. The following innovations are recognized as the most popular among dental implantologists:
- implantation of bone tissue of biological or synthetic origin;
- expansion of the alveolar part of the bones of the upper jaw;
- targeted bone regeneration with the installation of a specific membrane;
- For bone tissue atrophy in the marginal areas of the upper jaw, a sinus lift is used.
Each of these methods has its own advantages, however, like any other intervention in the body, there are significant disadvantages of bone grafting of any kind. The most important disadvantage of this manipulation is considered to be a large time investment, that is, the process of restoring the required volume of bone tissue can reach 6-7 months. Another disadvantage of the maxillofacial reconstruction process is the cost of the procedure, and only wealthy people can afford professional dental implantation.
Do I need to do a resection or still remove the tooth?
Tooth root resection is a tooth-preserving operation. The dentist will recommend it to you when there is at least the slightest opportunity to save the tooth. If the dentist does not see this possibility, then the conversation will immediately focus on removal.
When will the tooth have to be removed?
- You have a large cyst that affects more than a third of the tooth or several teeth.
- The root of the tooth is destroyed.
- There is severe inflammation of the tissues adjacent to the diseased tooth.
- The tooth is movable.
- Subsequent prosthetic replacement of a diseased, destroyed tooth with a crown is impossible.
Indications for surgery
- Poor endodontic treatment leading to inflammation of the root apex;
- the presence of a cyst, granuloma or other neoplasm, no more than 1 cm in diameter;
- perforation of the root walls during filling;
- pin or stump inlay in the dental canal;
- obstruction of the dental canal due to a congenital developmental defect;
- a crown or bridge placed on a tooth.
How is tooth root apex resection performed?
For the patient, resection of the apex of the tooth root is a simple operation and the procedure is tolerated quite easily.
First, the doctor makes an incision in the gum and bone tissue of the jaw to create access to the tumor. After which the tumor itself is removed along with the affected part of the tooth root. The entire cavity is thoroughly cleaned so that not even a small amount of infected tissue remains and is treated with an antiseptic.
Synthetic bone replacement materials are placed into the resulting space, which will take root over time and completely restore the patient’s bone.
Next, the wound is closed with a special self-absorbing membrane and the gum is sutured.
In order to protect the injured area, a bandage may be applied to the gum for up to 1 week.
After surgery, the patient may experience swelling of the gums and pain when chewing, which normally should subside within a few days.
Healing of the mucosa usually occurs in 7-10 days, the bone is restored in approximately 3-4 months.
Details about each of the listed methods
The most important advantage in dental implantation compared to conventional prosthetics and, in fact, the only way to solve the problem of dentition correction at the end of the last century was the preservation and stimulation of bone tissue. After the loss of a tooth, only an implant can ensure the safety of its alveolar parts, which significantly improves the quality of chewing food, diction and aesthetic appearance.
Splitting of the alveolar apex
This type of bone grafting is used in cases of horizontal bone melting to expand the area for implantation. In modern dentistry, this method is used most often, since it is suitable for plastic surgery of both jaws, and also has a low cost, due to the absence of the need to use expensive bone materials and membranes.
Splitting the area of the anatomical part of the jaw that bears the tooth serves as a kind of stimulation of natural osteogenesis. Another important advantage of the method is the possibility of simultaneous implantation, which significantly speeds up the process of restoring the dentition and the natural functions of the masticatory apparatus. Even if implantation is not possible immediately for some reason, it is carried out within a couple of months at most, which still speeds up the process compared to other methods.
Bone transplantation
Implantologists use this method to expand and lift the alveolar part of the future tooth using bone tissue transplants of various origins. For this manipulation, specialists use the following type of biological materials:
- bone tissue is taken from the patient from another area of the jaw (usually in the area of the 8th tooth, where the most active osteogenesis is noted);
- it is possible to implant donor tissue, that is, fragments of bone tissue of another person, possibly deceased (cadaveric biomaterial), which is allowed in most countries of the world;
- bone tissue of cattle has also proven itself positively in the restoration process of the alveolar areas of the jaws;
- synthetic, highly adapted bone tissue, which has a high degree of engraftment and stimulation of its own osteogenesis.
The implantation of bone tissue from a donor or animal undergoes multi-stage sterilization and adaptation, but implantologists still call the most effective method autotransplantation, that is, the use of one’s own bone tissue. the main disadvantages of this type of bone grafting to be :
- the need for another operation;
- long-term healing and restoration of bone volume;
- delayed possibility of the final stage of dentition correction.
Targeted bone tissue regeneration
Targeted correction of alveolar process tissue effectively restores its width and height. The method involves the use of donor or own bone material, as well as a specific membrane that separates and protects the formation of the implant site from adverse effects. A barrier in the form of a membrane makes it possible to provide the necessary shape and volume to the deformed area of the alveolar process and protect the transplanted tissue from resorption and mechanical damage.
However, the pronounced foresight of this method in terms of limiting the area of bone restoration also has a negative side, since the upper layer of bone tissue, due to the presence of the membrane, can partially degenerate, since the connection with the circulatory system is lost. This fact is the main disadvantage of this type of bone grafting . In addition, the pricing policy also plays an important role here, which is available to very few patients, since bone material and a self-absorbing membrane require significant financial costs.
Sinus lift
The sinus lift method is used to restore the bone tissue of the upper jaw. This method is acceptable even in patients with severe bone tissue deficiency. The base of the maxillary sinuses is involved in the process, that is, some of it is filled with bone fragments, which allows for full implantation at the proper level, with guaranteed durability, high-quality chewing ability, diction and a smile.
Before the operation, the doctor carefully examines the patient for the presence of an inflammatory process in the maxillary sinuses, chronic pathologies, and any restrictions due to the anatomical features of the structure. The dentist-implantologist considers computer and magnetic resonance imaging to be the most informative means in this case, which provide a layer-by-layer image, reproduce the future sinus lifting process on the screen and determine the amount of required bone tissue.
It should be noted that all methods of bone tissue correction are performed under local or general anesthesia, and in some patients there is a need for preliminary sedation due to increased excitability in anticipation of surgery.
What to do after tooth root resection?
Root resection is well tolerated by patients and does not cause major problems even in the postoperative period, but it is necessary to follow a number of rules that will alleviate the condition and speed up recovery.
Typically, after surgery, patients are prescribed antibiotics and vitamin supplements. They must be taken strictly as prescribed by the doctor.
It is necessary to maintain gentle but regular oral hygiene and use antiseptic rinses.
You can't overwork your body. During the healing period, it is better to limit physical and emotional stress.
Do not eat hot or hard food, it should be warm and soft.
What are the possible complications?
During the operation, damage to nearby anatomical formations is possible - blood vessels, sinus nerves, roots of neighboring teeth, therefore such operations are not performed on teeth closely adjacent to them. Due to the fact that the tooth root becomes much shorter - in the future it may become mobile; for the same reason, teeth after resection are rarely considered as a support for orthopedic structures. If after resection you still have to remove a tooth, installing an implant in this area may be difficult due to the reduced potential of the bone to heal.
The most correct decision would be to prevent the development of pulpitis and periodontitis. Treat your teeth on time!
Preparing for tooth extraction
Removing a tooth or its roots is a rather complex surgical dental procedure, but it will not be difficult for the patient to prepare for it. If local anesthesia is planned to be used for pain relief, the patient should eat a large meal before visiting the dentist because:
- After removing a tooth or root, it is forbidden to eat for several hours;
- salivation after eating is significantly reduced, which will make the dentist’s work easier;
- after eating, blood glucose levels are normalized and the risk of loss of consciousness under the influence of local anesthesia is reduced
In the case of general anesthesia, on the contrary, it is necessary to abstain from eating for several hours before the removal procedure begins. Drinking alcohol before visiting the dentist is prohibited. Alcohol affects the structure of the blood and does not combine well with anesthetics, not to mention the negative impact on the human psyche and behavior.
Inflammatory and infectious diseases of any nature must be cured before surgery to remove a tooth or its roots. The dentist must be warned about the presence of allergies to certain medications, in particular to anesthesia drugs.
A normal pregnancy in general is not a contraindication to dental procedures. However, during this period the use of a number of drugs used in dentistry is prohibited, so information about pregnancy is entered into the patient’s dental record. Also, detailed information about the patient’s chronic diseases, especially heart pathologies, is recorded in the dental record.
What is the difference between PRJ and more complex operations?
Cholecystectomy
- Cost: 100,000 - 160,000 rubles.
- Duration: 25-30 minutes
- Hospitalization: 3 days in hospital
More details
A patient who has undergone pancreatic cancer usually does not require lifelong doses of vitamin and mineral supplements that are absolutely necessary after gastric bypass or biliopancreatic bypass. The likelihood of metabolic side effects (protein, vitamin and calcium deficiency) is also less here. PGC does not require removal of the gallbladder, although if gallstones form in the gallbladder during weight loss, this may be necessary later. At the same time, if we talk about the stability of weight loss, biliopancreatic bypass undoubtedly leads here. Due to the fact that the operation of prostate cancer is relatively young, no one can yet say how stable its results are after 5-10 or more years. Therefore, we warn all patients who are considering the option of longitudinal gastrectomy that if over time the result of PRG turns out to be insufficient, a second stage of treatment may be required - gastric bypass or biliopancreatic bypass. In this case, the second stage will be easier to complete, since the “gastric” stage of biliopancreatic bypass has actually already been completed.
How new is this operation?
Indeed, longitudinal (synonyms: reduction, sleeve, tubular, vertical) gastrectomy is a relatively new bariatric operation. I used the word “comparatively” because in fact, longitudinal gastrectomy (LG) is an integral part of the biliopancreatic bypass operation in the Hess-Marceau modification, known in the world since the early 1990s and successfully used in our clinic since 2003. Therefore, we can confidently say that the technical details of this operation have already been well worked out. However, as an independent operation, PRG was first performed in the USA in the early 2000s by M. Gagner et al. as the first stage of biliopancreatic bypass surgery in severely obese patients. The calculation was made to carry out the second, “intestinal stage” of biliopancreatic bypass, in the future, as the preliminary weight loss and improvement of the patients’ condition occurred. It later turned out that in some patients, PRJ turned out to be a completely self-sufficient operation to achieve the desired weight loss. Since that time, and this is only a little over five years ago, PRG began to be used in many foreign clinics, and then in our country, as an independent operation. In our clinic, prostate cancer was first performed as an independent operation in 2004.
Reviews
- Review by Anton Nikolaevich Logvin
The operation was performed 6 years ago. Weight was 175. My knees started to hurt. It was impossible to find clothes. Constant feeling of hunger. Now I weigh 110. The weight suits me. I don't want to lose weight anymore. Boris Yurievich Tsvetkov is a surgeon from God, a very decent person and a wizard, an architect of human bodies. I'll say this.
Photos and interviews
- Review by Olga Vladimirovna Ryabokon
Before the operation, the weight was 154 kg and there were a million concomitant diseases. Now 87-88. I’m no longer treating diabetes, it doesn’t bother me, my blood pressure is very rare. At 64 years old, I don’t walk, I run. Before, I couldn’t walk through the kitchen; I was out of breath.
And after me, my daughter also had the same operation. All the best that I can, I know, all the good words, I dedicate everything...
Photos and interviews
- Review by Irina Sergeevna
Thank you very much to Boris Yuryevich for the gift of a new happy life, with all my heart. I say that I celebrate the day of the operation as my second birthday. My life has changed, my mind has brightened, my soul has brightened, I don’t know, it’s as if I’ve actually become younger. I was 44, now I’m 45, a new life has begun. Thanks to him for his golden hands, thanks to the whole team...
Photos and interviews
- Review by Marina Konstantinovna and Nate Donelson
I would like to express my deep gratitude to Boris Yuryevich and his entire team. The man who changed my life, who changed my husband's life, who saved my husband's life. I am very grateful to him. We are now planning a second child. He may have saved another life. We will have a second child, and at my former weight I could not give birth.
This is a surgeon...
Photos and interviews
- Review by Alexander Semchev
Friends! Previously, some time ago, it was difficult for me to live because the moment of my “promiscuity” played a bad joke on me. But, thank God, Dr. Tsvetkov and his clinic appeared in my life. Thanks to his efforts, his attention, I began to live differently. Of course, with a plus sign.
Photos and interviews
- Anna's review
I would like to say a huge thank you to Boris Yuryevich. He told me everything about the operations competently and in a language that I could understand, where there were any pros and cons. He gave me comprehensive answers to all my questions. He is a professional with extensive experience whom I trusted. I can say one thing. That this is a person who tells patients it like it is, in simple language accessible to...
Photos and interviews
- Review by Tatiana
Boris Yuryevich is a great guy, of course. Attentive, he told me everything that interested me. I walked differently from Marina, for example. Marina probably teased him for a very long time; he probably told a lot of things for a long time. I flew on wings. Everything would have been done faster for me. But what interested me, for example, the same operation, what to do...
Photos and interviews
- Alina's review
Boris Yurievich Tsvetkov is truly a doctor of the highest category, who is adapted for people. All people are different. Some work for their own personal gain. And Boris Yuryevich works for the people. It is available 24/7, which was very important to me. That I could call him at night and say: “Boris Yuryevich, I’m not feeling very well.” He always…
Photos and interviews
- Olga's review
Thanks to Boris Yuryevich for making people beautiful and happy. I already told him that I really have become more beautiful, younger, and much happier. I would like to wish him long life, even more career growth, newer modern technologies.
It's too bad he doesn't do breasts. It does the stomach, but he says I don’t do the chest now. And that’s what I would do...
Photos and interviews
- Valeria's review
I had gastric resection surgery and I am very pleased. What happened before and what happened after is noticeable in life, in health, in everything. A person changes - this is a new life. There is no need to be afraid of this operation, you need to go and do it. Boris Tsvetkov is a worthy, high-quality surgeon who will care for and guide his patient from beginning to end. In the hospital…
Photos and interviews
- Feedback from Natalya Anatolyevna Kukshina
I am a person who, at the age of 26 (at the time of the operation), has experienced a lot - various cleansing programs, nutritionists, fitness programs for losing weight, buying and consuming tons of products, as advertising aimed at weight loss instills in us, I can only say one thing. If you have problems with excess weight, diseases caused by excess...
Photos and interviews
- Alexey's review
What Boris Yuryevich Tsvetkov did... I want to say frankly. Without praising him, nothing, simply, what Tsvetkov did - he simply did what is impossible to do, you know? Tell someone else. I talked with other doctors, with endocrinologists, with therapists, there are a lot of people we know in medicine. Even people who are in this profession…
Photos and interviews
Features of postoperative rehabilitation
After such surgery, the patient should refrain from any physical activity for 24 hours. Eating food is allowed only after 3 hours. Subsequently, care must be taken to ensure that the oral cavity is not exposed to thermal irritants, to limit the consumption of spicy and salty foods, as well as the use of overly aggressive means for rinsing and brushing teeth.
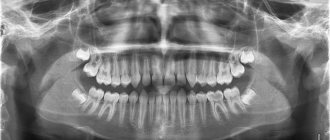
Swelling may persist for 1-2 days and moderate pain may be felt. To prevent the development of a purulent and inflammatory process, antibacterial agents and antiseptic solutions are prescribed, which must be used to thoroughly rinse the mouth. After 6 months you should undergo an x-ray examination.
Many patients are frightened by the phrase “gastric resection”. How justified are these fears?
Longitudinal gastrectomy is not at all the same resection that is performed for cancer or peptic ulcer disease. With PRG, the lateral part of the stomach is removed, while the important physiological valves of the stomach (cardiac sphincter and pylorus) are preserved, and thus the stomach after PRG remains physiologically quite functional. From a voluminous sac, the stomach turns into a narrow tube, where food does not stay long and quickly passes into the intestinal tract. The secretory activity of the stomach, of course, decreases, but this also plays into the hands of the goal of weight loss.
Are postoperative complications possible? What is their probability?
It is impossible to guarantee the absence of complications with any operation. In case of prostate cancer, a staple suture is placed along the entire stomach. Although these sutures are performed using high-quality staplers and are always reinforced, there is still a small risk of postoperative bleeding, as well as failure (cutting through) of some sutures, which in rare cases may require laparoscopic or surgical revision. To prevent suture insufficiency in the first two weeks after prostate cancer, nutrition should be in liquid form, without undue stress on the gastric sutures. Since the operation takes place in the area of the splenic hilum, we always warn that if significant bleeding occurs from the spleen, it may be removed. We also warn about this during other gastric surgeries performed due to obesity.
How likely is heartburn (reflux - esophagitis) to occur after prostate cancer? How to deal with this?
Firstly, the probability of reflux of stomach contents into the esophagus largely depends on the volume of resection, i.e. the larger part of the stomach is removed and the more the stomach looks like a narrow tube, the less the danger of reflux of gastric contents into the esophagus. Secondly, reflux esophagitis can be effectively treated and prevented with the help of antiulcer drugs (omez, quamatel, ranitidine, pariet, etc.) that inhibit gastric secretion. Such treatment can be prescribed for a period of 2 - 3 months after surgery, and then only if necessary. We are not proponents of additional “anti-reflux” interventions. They are justified only when it comes to large diaphragmatic hernias.