The powerful lymph nodes located around the pharynx cannot cope with the attack of the pathogen, so the body begins to produce antibodies that can find pathogenic bacteria, paralyzing their activity.
As a result, streptococci are defeated, but the child’s body produces so many antibodies that, in addition to foreign cells, the body’s own tissues, primarily the heart and joints, begin to suffer. Therefore, it is always better to entrust the treatment of sore throat in a child to a qualified doctor.
In 10% of cases, sore throat in children can be caused by Staphylococcus aureus, rarely pneumococcus, Haemophilus influenzae, chlamydia and fungal flora. Viral pathogens (adenoviruses, herpes virus) more often attack the body of children under 3 years of age.
Symptoms:
- red, swollen tonsils with white or yellowish coating or streaks;
- a sore throat;
- difficult and/or painful to swallow;
- fever (temperature above 38.0);
- cervical lymph nodes are enlarged;
- hoarse or hoarse voice;
- headache;
- stiff neck muscles;
- abdominal pain (especially in young children).
In infants:
- drooling due to pain in swallowing;
- anxiety;
- refusal to eat
- With chronic tonsillitis, your breath may smell bad.
How and why does infection occur?
Infection occurs by airborne droplets, from a sick person, by using shared utensils and eating contaminated food, as well as by a number of other factors:
- weakened immunity;
- hypothermia or consumption of cold foods and drinks;
- mouth breathing (for chronic adenoiditis, deviated nasal septum);
- irritation of the nasopharyngeal mucosa with a runny nose;
- recent viral diseases;
- inflammatory diseases of the ENT organs (sinusitis, sinusitis, otitis);
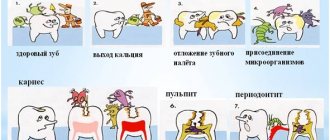
- caries and other oral infections.
Secondary tonsillitis in children can occur against the background of scarlet fever, diphtheria, mononucleosis, as well as blood diseases.
In any case, a sore throat develops rapidly, in a matter of hours, and is especially acute in children, accompanied by the main symptoms—a sore throat when swallowing and an increase in body temperature.
Complications of tonsillitis
- Labored breathing.
- Sleep apnea (holding your breath during sleep).
- Spread of infection to the tissue near the tonsils (peritonsillitis), peritonsillar abscess - accumulation of pus behind the tonsil.
- Acute cervical lymphadenitis is inflammation of the cervical lymph nodes.
Streptococcal tonsillitis can cause complications such as:
- acute rheumatic fever, affecting the joints, heart and other organs;
- glomerulonephritis (inflammation of the kidneys, which can lead to serious consequences, including kidney failure).
Treatment with antibiotics significantly reduces the likelihood of complications after streptococcal sore throat.
Diagnostic methods
During the consultation, the doctor will examine the patient’s throat and palpate the lymph nodes. The examination should be carried out by a pediatrician and pediatric ENT specialist. In case of decompensation of the chronic form, the child requires consultation with a pediatric cardiologist, rheumatologist, nephrologist, because tonsillitis can cause concomitant diseases. To rule out pockets of infection in the oral cavity, the child should be examined by a dentist. Laboratory and instrumental studies are also prescribed:
- blood and urine tests;
- pharyngoscopy;
- blood test to determine C-reactive protein;
- definition of ASL-O;
- bacterial culture from the pharynx for flora.
If there are difficulties in making a diagnosis, additional studies may be required - ECG, x-ray of the sinuses, etc.
Diagnosis of tonsillitis
- For tonsillitis, the doctor will examine the child's throat, as well as his ears and nose, where there may also be inflammation.
- The doctor will examine the child's skin, since streptococcal sore throat sometimes causes a specific rash. This is what is called “scarlet fever” - it is not some kind of separate disease, but a sign of damage to the body by streptococcus.
- The doctor will feel the cervical lymph nodes - as a rule, with tonsillitis they swell.
- The doctor will feel the spleen to distinguish a sore throat from mononucleosis, which also causes swollen lymph nodes.
- The streptococcal test is a simple and accurate way to distinguish streptococcal tonsillitis from viral tonsillitis. The doctor takes a scraping from the child’s throat and within 24-48 hours the result is ready.
- In some cases, a general blood test may be needed, the results of which can also indicate the viral or bacterial nature of the disease. It is usually taken if the streptococcal test is negative, but the course of the disease leaves the doctor in doubt.
About the clinic
Euromed Clinic is a multidisciplinary family clinic in the center of St. Petersburg.
- Calling a doctor to your home
- 24/7 therapist appointment
- Tests, ultrasound, x-ray
- Whole body diagnostics
- Hospital and surgery
- Vaccination
Find out more about the clinic
Causes of tonsillitis in children
The disease occurs due to the ingress of bacteria or viruses. Tonsillitis is often caused by streptococcus bacteria. The disease is also caused by adenoviruses, influenza and parainfluenza viruses, herpes, etc.
Other reasons:
- staphylococcus, pneumococcus, hemophilus influenzae and other microbial associations;
- enterovirus infection;
- mushrooms;
- parasites – membrane and intracellular (mycoplasma and chlamydia);
- disruption of the process of self-cleaning of lacunae against the background of restructuring of lymphoid tissue and dysbiosis of the respiratory tract;
- a single or multiple history of tonsillitis;
- ARVI, sinusitis, adenoiditis, caries, stomatitis, periodontal disease;
- anatomical features of the pharyngeal part of the lymphatic system - deep and narrow lacunae, adhesions, multiple fissure passages;
- burdened by concomitant diseases - food allergies, perinatal pathologies, rickets, impaired breathing through the nose, intestinal infections and other factors that reduce immunity.
Treatment of tonsillitis
The child should be provided with:
- peace and the opportunity to sleep as much as he wants;
- Drink plenty of fluids to relieve sore throats and prevent dehydration;
- air humidification;
- a sore throat can be relieved by both warm drinks and cold ice cream, especially popsicles;
- for a sore throat, it helps to gargle with a solution of table salt and soda - a teaspoon of salt and a small pinch of soda per 250 ml of warm water;
- Children over 4 years old can be offered lozenges for sore throats. Do not give candy to small children - they may choke;
- do not smoke when your child is sick, avoid strong odors that irritate the throat;
- A sore throat and fever can be relieved by medications containing paracetamol and ibuprofen. Don't give children aspirin; in rare cases, it can cause deadly Reye's syndrome.
Confirmed bacterial tonsillitis (usually streptococcal tonsillitis) is treated with antibiotics. It is dangerous to interrupt or stop the course because it increases the likelihood of infection spreading to the joints, heart, kidneys and other organs. Continue taking antibiotics even if your symptoms are completely gone.
Types of disease
- Spicy. Most often, the acute form develops after suffering from acute respiratory viral infection, due to reduced immunity. Source: A.D. Vetrova Acute tonsillitis in children: a pediatrician’s point of view // Pediatric pharmacology, 2014, v. 11, no. 2, pp. 61-64
- Chronic. Occurs after relapses if the patient has not fully recovered. Diseases in the mouth, nose, and structural features of the tonsils contribute to the development of chronic tonsillitis. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6248716/ Raja Kalaiarasi, Kalaivani S Subramanian, Chellappa Vijayakumar and Ramakrishnan Venkataramanan Microbiological Profile of Chronic Tonsillitis in the Pediatric Age Group // Cureus. 2022 Sep; 10(9): e3343
Clinical recommendations for disease prevention
The main methods of preventing tonsillitis in children are compliance with sanitary and hygienic measures (avoiding contact with patients and their things, washing hands, using a scarf and hand sanitizers) and strengthening the immune system (hardening, playing sports, etc.).
Tonsillitis is a common disease in children and adults, which without proper treatment can become chronic. If you notice symptoms of illness in your child, immediately contact the children's medical department.
Sources:
- HELL. Vetrova. Acute tonsillitis in children: a pediatrician’s point of view // Pediatric pharmacology, 2014, vol. 11, no. 2, pp. 61-64.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6248716/ Raja Kalaiarasi, Kalaivani S Subramanian, Chellappa Vijayakumar and Ramakrishnan Venkataramanan. Microbiological Profile of Chronic Tonsillitis in the Pediatric Age Group // Cureus. 2022 Sep; 10(9): e3343.
- T.V. Spichak. Diagnosis and treatment of tonsillitis in children from the standpoint of evidence-based medicine // Issues of modern pediatrics, 2010, vol. 9, no. 2, pp. 130-135.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Chronic tonsillitis in a child: treatment methods
This disease is diagnosed in children if inflammation of the tonsils occurs more than twice a year. In case of chronic disease, the tonsils themselves become a source of infection. The immune system weakens, and the child is often exposed to illness.
Chronic tonsillitis should be treated by an experienced otolaryngologist. Some ENT doctors recommend removing the tonsils immediately. But you need to remember, by removing the tonsils, you lose the body’s natural defenses against bacteria and viruses forever!
At the ENT Clinic of Doctor Zaitsev, we treat chronic tonsillitis, and we resort to removal of the tonsils only in the most extreme cases, when conservative treatment methods have been completely exhausted.
The procedures for ultrasonic medicinal irrigation of the tonsils using the “Tonsillor” apparatus (it can be seen in the photo) have a good therapeutic effect. Our clinic also has a unique vacuum attachment for this device, which has no analogues in other medical institutions. This attachment is painless, safe and can be used to treat children starting from school age.
Why does the temperature rise
Fever accompanies most infectious diseases, including acute tonsillitis2,3. The processes that cause an increase in body temperature are quite well studied. They are triggered by special substances pyrogens, which can enter the body from the outside (exogenous pyrogens) or be synthesized inside it (endogenous pyrogens).
Endogenous pyrogens are substances that enter the bloodstream during the destruction of immune cells and cells of the inflamed mucous membrane of the throat2,3.
Exogenous pyrogens in the case of tonsillitis can be various microorganisms: viruses, bacteria, fungi3. In children aged 3 months to 3 years, tonsillitis most often develops with mixed herpesvirus infections3. When a child reaches the age of 3-7 years, viruses give way to bacteria, and in 30% of cases the disease is caused by group A3 beta-hemolytic streptococcus. In addition, the tonsils are often affected by streptococci of other groups, staphylococci, etc.1 In adults, acute tonsillitis is often viral and accompanies ARVI1.
Exogenous and endogenous pyrogens affect the thermoregulation center located in the brain2,3. As a result, he begins to perceive normal body temperature as lower and increases the level of heat production, which leads to an increase in body temperature2,3.
Up to contents
When should you see a doctor?
Even slightly enlarged tonsils in a child are a signal to contact a pediatric otolaryngologist. However, mild hypertrophy of the glands often does not manifest itself in any way, so it cannot be noticed visually. A visit to the doctor is required if the child, in addition to enlarged tonsils, has:
- classic signs of a cold: pain when swallowing, redness of the throat, cough, nasal congestion, fever, uncharacteristic weakness, headache;
- white plaque on the tonsils;
- swollen lymph nodes;
- pustules, ulcers in the larynx;
- swelling of the neck.
"ENT Clinic of Doctor Zaitsev"
Treatment of tonsillitis in children in Moscow is offered by many medical institutions: from district clinics and multidisciplinary centers to private clinics. The main thing is to make the right choice!
Our clinic accepts patients from the age of three. The ENT clinic has everything necessary for the successful treatment of sore throat and chronic tonsillitis: the most modern equipment and instruments, its own treatment methods, and most importantly, highly qualified ENT specialists with extensive practical experience. A visit to a doctor for a small patient is always stressful, and our task is to make the appointment as calm and easy as possible for the child. The examination takes place in a playful way: the baby no longer perceives the treatment as something scary and unpleasant, and the mother’s saved nerves are worth a lot. Our clinic is equipped with a children's corner where a child can play, read, or just drink tea and cookies while the mother and the doctor discuss the treatment regimen. Prices for our services have not changed for more than three years and remain one of the best in Moscow.
If you have discovered the first signs of a sore throat in your child, or he has been suffering from relapses of chronic tonsillitis for several years, please do not delay and make an appointment. We will help you cope with this illness.
Treatment of candidiasis
The main method of treating the disease is the use of local antifungal and antibacterial agents, as well as antibiotics. Antimycotic (antifungal) drugs can not only eliminate the symptoms of the disease, but also destroy the fungus in the oral cavity, as well as in other organs and tissues. For this purpose, antibiotics of the polyene series (levorin, nystatin, etc.), as well as clotrimazole, econazole and other imidazoles, are used. Fluconazole, Diflucan, and Nizoral also have a pronounced antifungal effect.
A significant part of antibiotics has a number of side effects and has a negative impact on the immune system. Therefore, when treating children, antibiotics are used only in the most severe cases, as well as in cases where there is a risk of complications and generalization of the process. At the initial stages of the disease and with a mild course of the disease, preference is given to local remedies. We recommend using ASEPTA series rinses, which contain chlorhexidine and other active ingredients that have antimicrobial and anti-inflammatory effects. To remove plaque, you can use special ASEPTA Baby wipes. The individually packaged finger wipe is made of hypoallergenic materials and allows you to carefully clean the mucous membranes without the risk of damaging them or causing additional infection. It is also recommended to regularly treat the oral cavity with Lugol or silver solution. This procedure must be repeated every three hours.
For the prevention and treatment of candidiasis in children, diet and oral hygiene are also of great importance. It is recommended to exclude or strictly limit the amount of food containing simple carbohydrates - these are, first of all, confectionery and flour products. Make sure your child brushes his teeth regularly - it is best to use a special toothpaste for this, for example - ASEPTA Baby, Kids, Teens. The components contained in these pastes help prevent caries and, as a result, reduce the infectious load on the child’s immunity.
Causes
The main cause of the disease is infection with the Candida fungus, an opportunistic pathogen that is widespread among humans and animals. Candida is a yeast-like unicellular fungus that is part of the normal microflora in a significant proportion of healthy people. Most often it can be found on the surface of various mucous membranes of the body, for example, in the intestines, mouth, pharynx and tonsils. Today, about 150 varieties of this microorganism are known, 20 of which are capable of causing diseases in humans. The destructive effect of Candida on the mucous membranes and other tissues of the human body is due to the release of a large number of enzymes that break down proteins, fats and other cell components. As a result of this, symptoms characteristic of candidiasis such as burning, dryness, and soreness occur.
When unfavorable conditions occur, Candida becomes covered with a special protective shell, which helps the fungus survive in the external environment and travel from host to host. Infection can occur in various ways - airborne, household contact, intrauterine. Newborn children are infected, as a rule, from medical personnel, or during childbirth, when passing through an infected birth canal.
At an early age, the child’s body does not have a developed immune system, if only for the simple reason that he has had virtually no contact with infectious agents and has not developed the appropriate antibodies. This is why children under one year of age are especially prone to developing candidiasis. However, this disease also occurs in older children. In this case, its appearance and development is often preceded by the formation of multiple carious lesions of the teeth. Caries, which is a constant source of infection, contributes to the weakening of local and general immunity, resulting in the rapid and active proliferation of opportunistic and pathogenic microflora. This category also includes various fungi of the genus Candida and fluorosis.
Factors that can provoke the development of candidiasis in a child’s mouth are also various concomitant diseases, such as diabetes mellitus, diseases of the gastrointestinal tract, acute or chronic infections, and other somatic ailments. Poor oral hygiene, taking antibiotics, hormones and immunosuppressants, and insufficient or unbalanced nutrition also increase the risk of developing candidiasis.
For active reproduction of the fungus, certain conditions are necessary - in particular, this microorganism is most active at temperatures from 30 to 37 degrees Celsius. The level of acidity that is optimal for the growth of Candida occurs in a person’s mouth when consuming large amounts of sweets, flour and other foods containing many simple carbohydrates.
How is inflammation treated?
The tactics for treating enlarged tonsils in a child consists of treating the underlying disease that caused this symptom (taking antibiotics, antiviral or antifungal drugs), and influencing them directly to regenerate the affected tissues. The latter includes:
- washing the tonsils from pathogenic microorganisms and mucus with antiseptic solutions;
- reducing swelling - taking antihistamines and ultraviolet irradiation;
- UHF therapy, which improves blood microcirculation;
- exposure to ultrasound to free the lacunae of the tonsils from pus, which can accumulate in them;
- laser exposure to destroy infection and its pathogens.
Literature
- Delyagin V. M. Fever (new touches on an ancient picture) // Pediatrics. Consilium Medicum. - 2022. - No. 2. — pp. 89-93
- Belan Yu. B., Starikovich M. V. Fever in pediatric practice // Attending physician. - 2022. - No. 1. — P. 40-43.
- Krasnova E.I., Khokhlova N.I., Provorova V.P., Evstropov A.N. Differential diagnosis and therapeutic tactics for acute tonsillitis (tonsillitis) at the present stage // Attending physician. - 2022. - No. 11. - P. 58-63.
- Instructions for use of the drug HEXORAL® solution.
- Instructions for use of the drug HEXORAL® aerosol.
- Instructions for use of the drug HEXORAL®TABS.
- Instructions for use of the drug HEXORAL®CLASSIC.
- Instructions for use of the drug HEXORAL®TABS EXTRA.
Up to contents
come back
The degree of enlargement of the tonsils in a child
There are 4 stages of hypertrophy of the glands:
- At the first stage, the inflamed tissue of the tonsils covers no more than 30% of the lumen between the pharynx and the sky. In this state, it causes almost no discomfort, so it is difficult to detect at this stage.
- At the second stage, hypertrophied tissue covers half of the lumen. The child begins to have difficulty swallowing and breathing freely, and a sensation of a foreign body in the throat.
- At the third stage, there is severe difficulty in breathing and swallowing.
- On the fourth, the pharynx is almost completely blocked by inflamed tonsil tissue. It is difficult to bring the condition to this stage, since already at the third stage the child’s well-being requires immediate medical attention.
Prevention of tonsillitis
To reduce the risk of developing the disease, you need to devote time to preventing this disease and strengthening the immune system. It is necessary to accustom children to hardening procedures. Hardening will bring positive results if you do it gradually, and at the same time consistently and regularly.
It is important to eat healthy and varied, eat foods rich in vitamins and avoid seasonings that irritate the throat. You also need to remember the relationship between the ENT organs and the surrounding tissue. Therefore, it is extremely necessary to promptly treat dental diseases and any inflammatory processes in the nasopharynx and larynx.
From an early age, children should be taught sanitary standards: washing hands, washing fruits, covering their mouths when coughing with a handkerchief or napkin. During periods of epidemics, it is advisable to avoid places with large crowds of people.
Following these simple measures will help avoid inflammation and the unpleasant consequences of this disease.