What is the temporomandibular joint - TMJ
We use this joint while talking, chewing, yawning, laughing - very often. Around it are muscles and tendons that allow the jaw to move in different directions for different purposes.
TMJ problems occur for many reasons:
- violation of the dental system, for example, congenital anomalies of teeth, gums or bone tissue, malocclusions, injuries, poor-quality prosthetics;
- congenital anatomical abnormalities of this joint;
- increased or decreased tone of muscle fibers around the TMJ;
- active conversational load, for example, among actors, singers, speakers;
- central nervous system problems;
- disruptions in the functioning of the endocrine system;
- excessive tension of the jaw muscles, for example, due to the bad habit of biting nails.
What is the temporomandibular joint and why do problems arise with it? Detailed and clear - in the video:
Actors and singers with active oratorical articulation are at risk for TMJ arthrosis
Causes of pain in the jaw joint.
Like any other, the mandibular joint is a connection of bones. The lower jaw bone, the head of which is covered with cartilage tissue, is attached to the temporal bone. The articular disc serves as a kind of layer between them. Mouth movements are regulated by the work of the chewing muscles, which are already recognized as the most trained in the body. Together with ligaments, the muscles provide strength to the mandibular joint, while allowing the jaw to move in different directions. The mobility of the jaw is individual for each person and largely depends on the anatomical features of its structure.
Pain in the jaw when chewing or speaking causes significant inconvenience. There are many reasons why it can arise. To prevent complications, it is important to receive timely treatment.
The main causes of pain in the jaw joint:
Fracture
A fracture is diagnosed when complete or partial damage to the jaw bone is detected. A fracture is often the result of a strong mechanical impact on the mandibular joint. Fractures can be open or closed, single or comminuted. The consequences of a fracture can be deformation of the dentition, loosening or loss of teeth at the site of injury, displacement of teeth, numbness of the lower jaw, headache, and dizziness.
Treatment:
- the mandibular joint must be fixed with a tight bandage, and if necessary, the tongue is also fixed;
- ensuring peace;
- urgently seek qualified medical help.
Treatment is aimed at creating conditions for proper bone fusion and restoration of bite.
Osteomyelitis of the jaws
Osteomyelitis is an acute inflammation of the lower jaw bone caused by an infection, usually through a diseased tooth. Symptoms - not only the tooth hurts, but the entire jaw, fever - 38 and above, swollen lymph nodes in the neck, the inflammatory process is confirmed by a blood test.
Treatment:
- removal of infected teeth;
- complete sanitation of the oral cavity with antibacterial drugs;
- in case of complications, an incision is made in the area of the purulent focus and the purulent formations are removed.
- Delayed seeking medical help can lead to an abscess or sepsis.
Temporomandibular joint dysfunction syndrome
In addition to pain when chewing, dysfunction of the mandibular joint is accompanied by the presence of obvious sounds when moving the jaw, these can be clicks, a “clicking” sound or grinding. Noises of this kind indicate a displacement of the jaw bone in relation to the articular disc. Dysfunction in most cases occurs due to overstrain of the mandibular joint. It can occur as a result of periodic involuntary clenching of the jaw, for example, in sleep. In addition, dysfunction can develop due to stress.
Treatment:
- removal of muscle tone;
- eliminating muscle spasms (taking painkillers, applying cold compresses and ensuring complete rest is often quite enough to eliminate joint dysfunction).
Neuralgia
Various types of neuralgia can also lead to pain. For example, cranial neuralgia, which is a consequence of inflamed nerves of the skull, is often a source of jerking pain. With neuralgia of the glossopharyngeal nerve, the pain is localized in the area of the mandibular joint, and the area of its spread is extensive; the right or left side of the head can hurt completely, starting from the chin up to the temporal part. The pain will increase with palpation.
Treatment:
- prescription of medications;
- local anesthesia.
Arthritis
The most common disease of the jaw joint is arthritis. Depending on the cause, purulent, rheumatoid or traumatic arthritis can be diagnosed. Purulent arthritis. It develops if the maxillofacial joint becomes infected, resulting in purulent formations. The infection can result from diseases such as tonsillitis, influenza, or be the result of hypothermia. Infection in the mandibular joint can also penetrate through the blood, for example, with otitis media. In addition to pain, there is general weakness and increased body temperature.
Treatment:
- taking antibacterial drugs;
- in complicated cases, the purulent focus is opened, and the mandibular joint is treated from the inside with antiseptics;
- ensuring rest of the jaw joint during the treatment period.
Rheumatoid arthritis
It is also a very common disease that is infectious and allergic in nature. The most common culprits for this type of arthritis are streptococcal and staphylococcal infections. The consequences of rheumatoid arthritis are muscle fiber atrophy and tendon damage.
Treatment:
- electrophoresis session;
- physiotherapy;
- restriction of motor activity of the jaw joint during rehabilitation.
Traumatic arthritis.
It is a consequence of hemorrhage in the maxillofacial joint, resulting from strong mechanical impact. It is possible to develop this type of arthritis after dislocation of the lower jaw. The consequence may also be
subsequent deformation of the mandibular joint.
Treatment is similar to that used for other types of arthritis.
Osteoarthritis.
The main factor of occurrence is time. The disease appears due to wear and tear of the mandibular joint. People over 50 years of age are more susceptible. However, it can develop earlier and the cause may be previous diseases of the jaw joint, such as joint dysfunction, arthritis, or even unprofessional dentures. Symptoms in the form of pain appear in the later stages of the disease.
Treatment:
- relieving excess stress and load;
- use of special tires;
- conservative physiotherapy.
How to understand what is bothering you with TMJ: 4 obvious signs
If you feel discomfort while talking, chewing, or yawning, look out for these signs:
- Are there any clicks or popping sounds during jaw operation (only 20% of people who notice this symptom complain of pain, however, this is a reason to suspect arthrosis of the temporomandibular joint and go for a diagnosis);
- Is there a feeling of jamming of the joint (if the fossa and the articular head are not in perfect contact, you have to open your mouth as much as possible, trying to find the right point);
- How severe is the pain (can occur when chewing, radiate to the temples, under the tongue, ears, neck, sternoclavicular region);
- Has your general health changed (headache and dizziness, insomnia, hearing impairment, depression and other uncharacteristic manifestations are possible).
With TMJ dysfunction, some patients develop snoring
There are two main types of TMJ dysfunction:
- Myogenic (source: muscle pain);
- Arthrogenic (associated with TMJ condition).
Myogenic TMJ dysfunction usually occurs due to fatigue or tension in the masseter or accessory muscles. Leads to facial pain, headaches, and sometimes neck pain.
Arthrogenic dysfunction of the TMJ, as a rule, is the result of inflammation, degenerative changes in hard and soft tissues in the joint. It most often occurs due to capsulitis or synoviitis (inflammation), slipped discs, and degenerative arthritis.
Treatment tactics
If there is no arthrosis, but there is dysfunction, the tactics are as follows:
- determine the root cause and eliminate it, for example, grind teeth and fillings that impede the functioning of the joint, correct prosthetic errors, and correct the bite;
- reduce the load on the joint - the patient is recommended to switch to soft foods, massage the facial muscles and exercises to relax the jaws;
- if the defects are serious, surgical treatment is performed - bone or muscle plastic surgery of the area of dysfunction.
If the doctor determines degenerative changes in the cartilage tissue, treatment for osteoarthritis will be prescribed. With the help of painkillers, they relieve pain. If necessary, a complex of physical therapy is prescribed, for example, laser or ultrasound. Good results are achieved by intra-articular injections of the Noltrex synovial fluid prosthesis, which restore the functionality of the joint by replenishing the missing lubrication.
Arthrosis of the TMJ is successfully treated with intra-articular injections of Noltrex
TMJ diseases
Diseases of the TMJ (temporomandibular joint) are characterized by a common symptom - dysfunction of the masticatory apparatus - and are the competence of orthopedic dentistry.
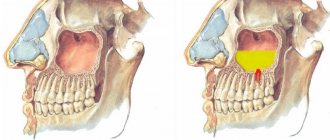
Arthrosis of the TMJ
Arthrosis of the TMJ is a disease that occurs as a result of uneven load on the joint: on the one hand, compression, and on the other, stretching. Increased loads can occur due to malocclusion, occlusion and articulation, as well as if incorrect prosthetics were performed (insufficient examination, poorly fixed fixed prosthesis, incorrectly sized bridge, excessive grinding of the tooth for a crown).
Symptoms of TMJ arthrosis:
- Pain in the joint in a calm state, inactivity;
- Clicking and crunching in the joint;
- Stiffness in the lower jaw after a night's sleep or after prolonged exercise (long conversation, chewing food);
- Limited mouth opening;
- Moving the jaw to the side when opening the mouth.
Treatment
The treatment of arthrosis of the TMJ requires an integrated approach from a group of doctors:
- Orthopedic treatment – corrects malocclusion – straightens the shape of the teeth, corrects the relationship of the dentition, installs or replaces previous dentures;
- Therapeutic treatment – partial grinding of teeth that interfere with the normal closure of the jaws;
- Physiotherapeutic methods – galvanization, massage, electrophoresis.
Arthritis of the TMJ
TMJ arthritis is inflammation of the temporomandibular joint of infectious or non-infectious origin. Initially, it spreads only to the joint capsule, then it can reach areas of the bone, accompanied by the melting of cartilage and the appearance of connective tissue in the joint cavity.
There are two stages of the disease: acute and chronic. When acute pain becomes severe, visible deformation of the face and swelling are observed. The joint is constantly stiff. In the chronic stage, painful sensations increase with movement, and in an immobilized state they are moderate or weakly noticeable. The joint is stiff in the morning.
Symptoms of the disease:
- Acute throbbing pain when moving the joint (talking, chewing), radiating to the temple, back of the head;
- Pain on palpation of the lower jaw;
- Redness of soft tissues and their swelling;
- Feeling of fullness in the jaw.
Treatment
- Immobilization of the diseased joint by applying a sling-shaped bandage to the lower jaw or other methods;
- A diet that excludes chewing food for 3 days;
- Using analgesics and cold compresses for pain relief;
- Taking antibiotics, injections of chondroprotectors and corticosteroids into the joint;
- Physiotherapeutic measures – mud therapy, ultraphonophoresis.
Ankylosis of the TMJ
Ankylosis of the TMJ is a partial or complete loss of mobility of the lower jaw, which is caused by fibrous or bony fusion of the joint surfaces. The danger of this disease is that it can occur for many years without symptoms until the cartilage completely dies. Bone ankylosis develops in childhood, while fibrous ankylosis occurs in adults.
Symptoms of the disease:
- Limitation in opening the mouth;
- Impaired breathing (night apnea and snoring), speech, chewing;
- Distortion of the face to the side;
- Shortened and underdeveloped lower jaw;
- Increased formation of plaque and tartar.
Treatment
The treatment has two goals: restoring joint mobility and facial aesthetics.
In the first stages, treatment may be limited to physiotherapeutic measures in the form of ultraphonoresis, hyaluronodase, as well as hydrocortisone injections into the joint. Sometimes they resort to mechanical expansion of the jaws under anesthesia or surgical dissection of the adhesions.
Persistent deformities and adhesions in late stages of development can only be eliminated surgically. The complexity of the operation should be taken into account due to difficulty breathing in patients with this disease. In some cases, a tracheotomy is required.
Ankylosis can be prevented by timely treatment of diseases of the facial joints and birth injuries in children.
Musculo-articular dysfunction of the TMJ
Impaired coordination of the muscles of the lower jaw and the joint, as well as the placement of the head and disc of the joint relative to the tubercle. Factors that contribute to the development of this disease may be incorrect orthodontic treatment, unprofessional implantation, bone grafting of teeth, sinus lifting, as well as endocrine, articular and other diseases.
Symptoms:
- Painful sensations in the jaw, increasing at night and with movement (in another form, painful sensations may be absent);
- Clicking sounds when moving the jaw;
- Temporary stiffness in jaw movement;
- Tension of the facial muscles, most often one-sided;
- Sleep disturbance.
Treatment
The main task is to create the correct bite for the patient and restore normal jaw closure. These tasks are carried out by grinding protruding contacts on the surface of the teeth, which interfere with the normal closure of the jaws. Advanced stages can only be treated surgically - dissection of adhesions, straightening and installation of the disc in place.
TMJ dislocation
TMJ dislocation is a displacement of the head of the joint beyond its normal location, in which the function of the lower jaw is completely disrupted. There are 2 types:
- traumatic - received as a result of a blow to the jaw, yawning or screaming;
- habitual - which develop as a result of stretching of the joint capsule and ligaments.
Symptoms:
- The lower jaw is displaced downwards, the mouth does not close on its own;
- Excessive salivation;
- The appearance of depressions in the area of the tragus of the ear and protruding heads of the joint in the area of the cheekbones;
- Strong pain.
Treatment
- Reduction of the joint;
- Immobilization of the TMJ.
What symptoms should you see a doctor for?
The earlier the diagnosis is made, the more favorable the prognosis. So seek help if:
- you experience pain in the lower jaw - intense or mild;
- you cannot fully move your jaw, you feel limited;
- hear a painful clicking or crunching sound when opening and closing your mouth;
- pain and noise in the ears appeared (especially if the otolaryngologist did not find any pathologies);
- There was a feeling of incomplete bite.
Arthrosis of the TMJ is not a very common phenomenon, but quite dangerous. Our usual comfort during conversation, eating, and other household activities is at risk. To avoid this, do not attribute alarming symptoms to fatigue and do not rely on “it will go away on its own”: be sure to find time for yourself and your health!
Dental pathologies
The temporomandibular joint hurts quite often due to problems with the gums or teeth. In such cases, discomfort may be reflected. Initially, they are localized in a certain area of the jaw, and then spread to neighboring areas of the face. TMJ pain sometimes occurs after installation of braces or removable dentures. Associated symptoms include recurrent headaches and excessive tooth mobility. Usually, after the correct bite is formed, all unpleasant sensations disappear without a trace. But if the pain persists for 6-8 weeks, you should contact your dentist for an examination. Also, discomfort in the TMJ area sometimes occurs several days or weeks after tooth extraction. The causes of acute or aching, pressing pain can be the following pathologies:
- alveolitis Post-traumatic infection and inflammation of the tooth socket. The pathological condition is characterized by severe pain, weakness, elevated body temperature, enlarged submandibular lymph nodes, and an unpleasant, putrid odor from the mouth;
Alveolitis.
- phlegmon. This is a purulent process without clear boundaries, caused by Staphylococcus aureus, prone to spreading to surrounding tissues. The upper and (or) lower jaw swells, when trying to open the mouth, acute pain occurs, there is a lack of appetite, hyperthermia, facial asymmetry, weakness, drowsiness, apathy;
Phlegmon of the lower jaw.
- abscess of the jaw area. In the connective tissue structures, a cavity is formed, limited from the surrounding tissues and filled with purulent contents. An abscess is characterized by swelling, elevated body temperature, skin soreness, fluctuation, headaches, hyperemia, malaise, and sleep disturbance.
Abscess.
But the most dangerous pathology is osteomyelitis, which affects the temporomandibular joints. With the development of a purulent infectious-inflammatory process, all structural components of the jaw bone are gradually involved in it. In the absence of medical care, osteonecrosis occurs. Clinical manifestations of osteomyelitis of the jaw include weakness, fever, chills, pain, limited mouth opening, tooth mobility, inflammatory infiltration of the soft tissues of the face.
If your temporomandibular joint hurts, it is advisable to first consult a dentist. The doctor will conduct the instrumental and laboratory tests necessary to make a diagnosis. The dentist will eliminate pathologies that correspond to his profile, or refer the patient to other specialists for further treatment.
Main causes and clinical manifestations
The jaw joint always hurts when its integrity is violated as a result of injury. This kind of damage to bone or cartilage structures is often the result of an impact, a fall from a height, or a traffic accident. Under mechanical influence, the lower and (or) upper jaw is injured. Fractures happen:
- direct or reflected;
- single or multiple;
- open, closed, displaced.
Localization of fractures.
The most severe form is considered to be splintered, requiring complex surgery. The victim finds out that the jaw joint hurts due to a fracture during an X-ray examination at the emergency room. But sometimes, for example, after a fight, the intensity of the discomfort increases gradually. The causes of pain are cracks in the bone, dislocation or subluxation, which disrupt the functioning of the TMJ. The following clinical manifestations indicate injury:
- pain that increases when opening the mouth;
- swelling of the lower jaw;
- stiffness of movement, impaired motor functions.
If the integrity of the skin is damaged during injury, pathogenic microorganisms can penetrate into the joint cavity from the surface of the epidermis. During their life, they release toxic substances that provoke the development of the inflammatory process.
Osteomyelitis
Osteomyelitis is an inflammatory pathology of the bone marrow that affects all elements of the bone: periosteum, spongy and compact substance. The pathology is provoked by pathogenic bacteria that penetrate the TMJ with the blood flow from the primary lesions or when the pocket, which is located between the gum and one of the teeth, is damaged. Osteomyelitis can be nonspecific, caused by staphylococci, streptococci, enterococci, and pathogenic fungi. A specific disease occurs with tuberculosis of bones and joints, brucellosis, gonorrhea, chlamydia, syphilis. When choosing treatment methods, its form is taken into account:
- post-traumatic, most often occurring after open fractures;
- gunshot, the cause of which is a fracture as a result of a bullet wound;
- postoperative, developing due to the installation of wires or the application of compression-distraction devices;
- contact, provoked by the spread of the inflammatory process from soft tissues.
If the jaw joint hurts, then the cause may be endogenous osteomyelitis of the TMJ. Pyogenic bacteria penetrate bone tissue from foci located in other parts of the body. They are carried by blood from phlegmons, infected wounds, soft tissues affected by purulent inflammation.
Acute osteomyelitis is indicated by frequent headaches, elevated body temperature, lack of appetite, insomnia, and fatigue. Chronic pathology is diagnosed quite rarely, usually in young patients. Relapses occur with exacerbation of concomitant diseases, decreased immunity, and hypothermia.
Odontogenic factors
The jaw often hurts when chewing due to the development of an odontogenic inflammatory disease - periodontitis, periostitis. Their complications can also provoke discomfort: abscesses, phlegmons, lymphadenitis, sinusitis. The pathological conditions have one thing in common: the tooth or nearby tissues become the entry gate for pathogenic microorganisms. The infection spreads in various ways, affecting the bone jaw structures, perimaxillary soft tissues, lymph nodes, anatomical formations localized near the TMJ and distant organs.
The cause of pain can be banal caries. If left untreated, the deep parts of the tooth are damaged, including the nerve, pulp, and soft tissue. As a result of demineralization and destruction of hard tooth tissues, a cavity defect is formed, in which the source of infection is located - pathogenic bacteria and fungi.
A patient at a dentist's appointment complains of throbbing, sharp pain, often occurring in the jaw joint at night. Their severity increases when chewing or eating hot or cold food. If the pathology affects the trigeminal nerve, then the lips begin to go numb, the chewing muscle tone decreases, and the pain becomes piercing, radiating to the back of the head, temples, and forehead.
Osteoarthritis
Osteoarthritis of the TMJ is a chronic pathology caused by degenerative processes in the tissues of the joint. It is characterized by the gradual destruction of cartilage tissue and the formation of bone growths (osteophytes). As a result of thinning of cartilage and decreased production of synovial fluid, the functional activity of the joint is significantly reduced. While experiencing food or talking, painful sensations arise. When you move your jaw, you hear crunching and clicking sounds. In the morning, the joint swells, but during the day the swelling disappears due to the production of special hormone-like substances in the body. After sleep, some stiffness of movements and joint stiffness are felt.
Under the influence of negative factors, for example, hypothermia or the development of any infection, synovitis can occur - an inflammatory process in the synovium with the accumulation of fluid in the joint cavity. It is often accompanied by symptoms of general intoxication of the body:
- increased body temperature;
- headaches, dizziness;
- dyspeptic disorders.
After about six months, the range of movements of the TMJ is limited, stiffness is observed, and the patient involuntarily shifts the jaw to one side when opening the mouth. The area affected by osteoarthritis may experience numbness and tingling of the skin. Headaches, ear pains, and eye pains occur. Sometimes a person with osteoarthritis turns to an otolaryngologist with complaints of hearing loss. Patients often ask doctors why the jaw joint hurts and why it hurts to open the jaw. Often this indicates the development of ankylosis - complete or partial fusion of the joint space.
Arthritis
The jaw joint often hurts as a result of arthritis. This pathology affects almost all structures of the TMJ - synovial membranes, capsule, cartilaginous and soft tissues, adjacent muscles, ligamentous-tendon apparatus. The disease begins with the development of an inflammatory process in the membrane lining the inner surface of the joint. Gradually it spreads to other structures, which leads to disruption of the functioning of the joint.
| Type of temporomandibular joint arthritis | Causes |
| Specific and nonspecific infectious | The cause of inflammation is the penetration of viruses, pathogenic bacteria or pathogenic fungi into the cavity of the TMJ. These can be Staphylococcus aureus, streptococci, E. coli, pathogens of syphilis, gonorrhea, brucellosis, tuberculosis |
| Reactive | Occurs as a result of infection of the TMJ. But pathology does not develop as a result of the vital activity of microbes and viruses, but due to an inadequate response of the immune system to their penetration |
| Rheumatoid, including juvenile | The development of pathology is provoked by a combination of certain factors. This is a genetic predisposition, infection, a sharp weakening of the body’s defenses |
| Gouty | Occurs when there is a metabolic disorder of uric acid, the salts of which begin to crystallize and deposit in the TMJ |
At first, the clinical manifestations are not pronounced. A person occasionally feels weak and gets tired quickly. Malaise is usually attributed to fatigue after a hard day at work. But the severity of symptoms increases, as does the frequency of their manifestations. Soon the clinical picture is complemented by the leading sign of any form of arthritis - arthralgia, or joint pain. She has a stable wavy character. The intensity of the pain syndrome increases in the second half of the night and in the morning.