Anatomy, physiology
The periodontium
is a complex organ of the oral cavity surrounding the teeth, formed from specialized tissues. It is located on the jaws and its main functions are to support (support) the teeth and their nutrition and innervation.
Nutrition (trophism) is provided by blood and lymphatic vessels that supply oxygen and metabolic products to the periodontal tissue.
There are four main anatomical and functional elements of the periodontium:
- gum,
- periodontium,
- alveolar bone with periosteum,
- root cement
The gum is a soft tissue - a mucous membrane covering the alveolar processes, with an underlying connective tissue layer.
It contains lymphatic vessels (they are involved in regulating fluid pressure in tissues and protecting against microbial agents).
Through the periodontium - the ligament of the tooth, the latter is fixed in the jaw bone.
Periodontium
(otherwise known as desmodont) is a connective tissue formation surrounding the tooth and located between the root cement and the inner cortical plate of the alveolar bone.
This ligament, consisting of the main substance, fibers and cellular elements, like an elastic gasket, absorbs the load on the tooth, giving it minimal mobility. When periodontal disease and death occur, fusion of the bone with the tooth – ankylosis – can occur.
The next element of the periodontium is cement, which is also a hard tissue covering the root of the tooth. It is formed by collagen fibers directed along the root and an adhesive substance.
Bone
The alveolar process, in which the tooth is strengthened by periodontium, is composed of outer and inner dense plates and a spongy part between them.
Spongy bone consists of trabecular septa, the direction and shape of which is determined by the load on the jaws and teeth, and bone marrow.
Bone tissue contains mainly crystals of hydroxylapatite (inorganic) and small amounts of water and organic substances.
The cellular elements of bone - osteoblasts, osteoclasts and osteocytes, under the influence of the nervous and humoral system, determine changes in the shape, volume and quality of this tissue.
The bone tissue of the alveolar process is covered with a dense connective tissue structure - the periosteum; it, with the vessels located in it, plays a significant role in the blood supply to the bone.
The blood supply provides tissues and anatomical formations with organic and mineral substances.
At the level of the enamel-cement junction (neck of the tooth), an anatomical formation stands out in the marginal part of the gum - a vascular cuff, which, like an elastic band, ensures a tight fit of the gum to the tooth due to hydrostatic pressure.
The main source of blood supply to periodontal tissue is the external carotid artery with the maxillary and mandibular arteries branching from it.
Venules and veins collect blood into the internal jugular vein. The periodontium is innervated by the trigeminal nerve and the superior cervical sympathetic ganglion.
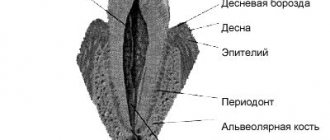
Among others, there is an anatomical formation - the dentogingival junction
. This is the connection between the gum epithelium and the neck of the tooth.
It is physicochemical: molecules of epithelial cells adhere to cement structures through gingival fluid cells.
Gingival fluid produced by periodontal tissue plays the role of a protective barrier against microorganisms through the activity of phagocytes and its chemical properties. It should be noted that the periodontium is washed by saliva. It is secreted by the major and minor salivary glands.
In addition to water (99.42%), saliva contains organic substances, salts and trace elements. Organic substances enter the oral fluid from blood serum and are secreted by the salivary glands and microorganisms present in the mouth.
Of the inorganic substances, calcium phosphate and calcium bicarbonate (they take part in the formation of tartar), phosphate and sodium chloride are important.
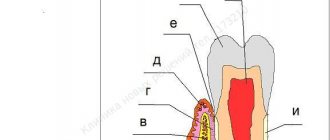
Diagram 1: periodontium
. a – submucosal layer with lymphatic vessels; b — mucous membrane of the attached gum; c - spongy bone of the alveolar process between the plates of the compact substance; d – periodontal fibers are woven into the root cement; e – gingival margin with vessels of the gingival cuff; e – dentogingival junction; g – tooth enamel; h – dental pulp; and – root cement; j – root dentin.
Age-related changes in periodontium
In the periodontium, with age, there is a decrease in the number of collagen fibers and a decrease in their quality. The epithelial layer of the mucosa becomes thinner, and keratinization is disrupted.
The bone tissue of the alveoli becomes less dense, the cortical layer atrophies.
Dentistry (rare atlases and books) / Periodontal diseases in children
7
the plate of the mucous membrane is smooth, because There are no connective tissue papillae here.
The attachment epithelium is multilayered and is a continuation of the sulcus epithelium. The surface cells of this epithelium provide attachment of the gum to the tooth surface using hemidesmosomes associated with the second (inner) basement membrane. As a result, they are not subject to desquamation. The cells lying under the surface layer of the epithelium undergo desquamation, which are displaced towards the gingival sulcus and sloughed into its lumen, i.e., epithelial cells from the basal layer are displaced simultaneously towards the enamel and gingival sulcus. The intensity of desquamation of the attachment epithelium is very high, but the loss of cells is balanced by their constant new formation in the basal layer, where epithelial cells are characterized by very high mitotic activity. The rate of renewal of the attachment epithelium under physiological conditions is 4-10 days in humans.
The cells of the attachment epithelium differ from the epithelial cells of the rest of the gum: they contain more developed granular endoplasmic reticulum and the Golgi complex, a set of cytokeratins, surface membrane carbohydrates, etc. All this is typical for poorly differentiated cells. This is important for preserving their ability to form hemidesmosomes, which ensure the connection of the epithelium with the surface of the tooth. The intercellular spaces in the attachment epithelium are expanded and occupy about 20% of its volume, and the content of desmosomes connecting epithelial cells is reduced four times compared to those in the sulcal epithelium. Due to this, the attachment epithelium has high permeability, allowing the transport of substances through it in both directions. From the oral fluid and from the surface of the mucous membrane, a massive flow of antigens into the tissues of the internal environment occurs; many substances are transferred in the opposite direction: from the blood to the epithelium and then into the lumen of the gingival sulcus.
The lamina propria in the area of the periodontal junction is formed by loose fibrous tissue with a large number of small vessels. Four to five parallel arterioles form a dense network-like plexus in the area of the gingival papilla. The capillaries of the gums are very close to the surface of the epithelium: in the area of epithelial attachment they are covered with only a few layers of spinous cells. The blood flow of the gums accounts for 70% of the blood supply to other periodontal tissues. Comparison of microcirculation levels at symmetrical points of the gums on the upper and lower jaws, as well as on the right and left, during a biomicroscopic study, showed a uniform distribution of capillary blood flow in the intact periodontium.
Granulocytes (mainly neutrophils) migrate through the vascular wall, less often monocytes and lymphocytes, which
Classification of periodontal diseases.
Gingivitis
Gingivitis is an inflammatory superficial disease of the gum tissue.
With gingivitis, there is no disruption of the periodontal junction and bone. Based on the form of manifestation of periodontal disease, the following are distinguished:
- catarrhal gingivitis,
- hypertrophic gingivitis,
- ulcerative gingivitis.
According to the type of course, gingivitis is divided into acute, chronic, aggravated and remission. According to the distribution, gingivitis can be localized and generalized. Without active treatment, gingivitis progresses to periodontitis.
Periodontitis.
Periodontitis is a deep inflammatory disease of the periodontium with destruction of the periodontal junction and bone tissue of the alveoli.
There are acute, chronic course of periodontitis, exacerbation of the disease and remission. Periodontitis can be mild, moderate or severe.
According to the prevalence, this gum disease is divided into generalized and localized periodontitis.
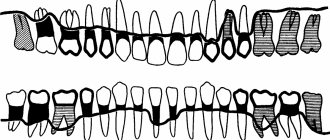
Photo 1. X-ray picture of severe periodontitis. The roots of the teeth are exposed by two-thirds.
2. 1.
Additionally, there is a condition known as
an aggressive form of periodontitis.
This diagnosis can be made by a doctor based on the presence of a set of signs of gum disease. In this case, periodontal destruction is generalized and rapid.
Such periodontitis is typical for ages from adolescence to 35 years. Often the aggressive form of periodontitis is accompanied by gum growth and granulation. During the period of remission, inflammatory manifestations may subside and even disappear.
Periodontal disease
Periodontal disease is a chronic degenerative periodontal disease.
In European and American classification as a separate gum disease
doesn't stand out. Periodontal disease is characterized by a long-term, benign course and almost does not lead to loosening and loss of teeth.
Periodontal diseases - as symptoms of other diseases
There are idiopathic periodontal diseases with progressive destruction of periodontal tissue (periodontal syndrome).
Such conditions can occur when exposed to physical factors (radiation), poisoning, immunodeficiency, diabetes mellitus, eosinophilic granuloma, Papillon-Lefevre syndrome, neutropenia, etc.
Periodontomas. Epulis (epulid) and gingival fibromatosis
Periodontomas are tumors and tumor-like conditions of the gums. The most common of them are epulis (epulid) and gingival fibromatosis.
Gingival fibromatosis is characterized by the proliferation of periodontal tissues, which causes tumor-like damage to the gum tissue. Gingival fibromatosis is most common in adults, but is sometimes diagnosed in children.
The diagnosis of gingival fibromatosis is made by a specialist based on the patient’s complaints, examination data, radiography, and histological examination.
The main reason for the growth of gum tissue, as a rule, is a violation of metabolic processes; drug-induced fibromatosis of the gums is also identified. Treatment of the disease is surgical and consists of excision of the overgrown gum to the periosteum.
Photo 2. Gingival fibromatosis
Periodontal diseases in children
Key words: periodontal diseases in children, gingivitis, periodontitis, periodontal disease, percentage
Introduction: The significance of periodontal diseases among the child population is determined by their steady growth, widespread distribution and the negative impact of periodontal foci of infection on the body as a whole. The severity of these changes depends both on the general condition of the body and on the age-related characteristics of the structure of periodontal tissues. During the period of growth and development of the dental system, and periodontal disease in particular, long-term pathological processes lead to disruption of tissue formation and early destruction of the periodontal complex, development of mobility and tooth loss. The prevalence of periodontal disease in children is increasing. Thus, according to A. M. Politun, in schoolchildren it is 39%; periodontitis is more common at puberty (13–15 years) and is 7.7% and 11.3% in 16–18 years. The issue of the prevalence of periodontal diseases in children has not been sufficiently studied, and therefore we decided to carry out this work.
Purpose of the study: To calculate the percentage of patients with various periodontal diseases among the child population of Vladikavkaz.
Materials and methods: The studies were conducted at the SOGMA dental clinic. The study involved 136 patients aged 4 to 16 years living in Vladikavkaz. All subjects were divided into 3 groups by age:
Group 1 – 4–7 years (39 people)
Group 2 – 8–12 years old (51 people)
Group 3 – 13–16 years old (46 people)
During the work, the data from the medical record (F.043/u) was taken into account. The study was carried out in two stages. At the first stage, a survey was conducted (identification of complaints and careful collection of anamnesis), examination of the oral cavity, percussion, and palpation. At the second stage, special research methods were used: Schiller-Pisarev test, x-ray, determination of Fedorov-Volodkina indices, PI and PMA. The presence of deposits of supragingival tartar, plaque (plaque), and subgingival tartar was assessed. Inflammatory phenomena in the gums were assessed according to the following signs: hyperemia, swelling, bleeding, desquamation, ulceration. In addition to these signs, atrophic and hyperplastic processes were noted. In the presence of a pathological process, its localization, quantity, symmetry, staining intensity, size, and quantity were taken into account.
Research results:
When examining the first group of patients (4–7 years):
− In 16 patients (41%), mild to moderate catarrhal gingivitis was found, which is characterized by hyperemia of the marginal periodontium, edema, bleeding from the apexes of the papillae when pressed at their base, and the presence of dental plaque. The general condition is not disturbed.
− 11 patients (28%) had hypertrophic gingivitis. Of these, 7 (18%) had an edematous form and 4 (10%) had a fibrous form. Clinically, this process manifests itself in the form of significant growth of the gums in the area of the front teeth. Swelling and hyperemia are weakly expressed.
- Hypertrophic gingivitis.
− Only 7 patients (18%) had ulcerative gingivitis. It is characterized by ulceration of the gingival margin, the ulcerative surface is covered with fibrinous plaque, which, when removed, causes bleeding.
− Localized periodontitis was observed in only 8 patients (21%), and generalized periodontitis (mild) in 15 patients (59%) and was objectively manifested by bleeding, deposits of subgingival tartar and plaque, mobility of teeth of varying degrees, pain, purulent discharge from pocket
− No periodontal disease was detected.
When examining the second group of patients (8–12 years old), we found:
− Catarrhal gingivitis with generalized symmetrical lesions in 19 patients (37%);
− Hypertrophic gingivitis was present in 21 patients (41%). Of these, the edematous form is in 15 (29%) people, the fibrous form is in 6 (12%) people.
− Ulcerative gingivitis, accompanied by fever, headache, insomnia and enlarged and painful regional lymph nodes, was observed in 10 patients (20%).
− Localized and generalized periodontitis was found in 11 (22%) and 17 (33%) patients, respectively.
− Periodontal disease was observed in 1 (2%) patient. In this form there are no inflammatory phenomena and periodontal pockets. It is characterized by good fixation of teeth, gum retraction, exposure of tooth necks and wedge-shaped defects.
When examining the third group of patients (13–16 years old), they received:
− Catarrhal gingivitis in 26 patients (57%), hypertrophic - in 23 patients (50%) and ulcerative - in 18 patients (39%). Localized periodontitis was observed in 15 patients (33%), and generalized in 10 patients (22%). Periodontal disease was observed in 3 (7%) patients.
Conclusions: Periodontal disease in children is one of the first morbidity problems in pediatric dentistry; it is necessary to devote more time to the prevention of periodontal disease in order to avoid morbidity, as well as to reduce the percentage of periodontal disease in childhood. It is necessary to talk with parents about the dangers of bad habits, proper nutrition and the consequences of abnormalities in the position of teeth and bite.
Literature:
- E. V. Borovsky, Yu. M. Maksimovsky // Periodontal diseases // Therapeutic dentistry 2001 - P.366–422.
- E. G. Denisova // Periodontal diseases in children // Textbook for dental interns, 2008 - pp. 55–75.
Etiology and pathogenesis (causes and development) of periodontal diseases
Calculus
The main point in the development of gum diseases such as gingivitis and periodontitis is dental plaque (plaque), which turns into tartar (calculus).
Photo 3. Soft plaque (plaque). Marginal periodontitis.
It is believed that organic soft dental plaque, which is formed from food debris due to poor hygiene, is gradually saturated with calcium from saliva and serum exudate of the gum pockets and is converted into hard tartar.
The latter can be of different hardness and color, which is determined by its composition. It consists of 18-25% organic matter (microbes and dead cells) and 75-82% inorganic matter (calcium, phosphorus, metal salts).
Tartar causes traumatic compression of the gums and prevents the cleaning of the periodontal pocket, promoting the development of microbial agents.
Microorganisms diffuse deep into periodontal tissues, lingering on the surface of the basement membrane and further into the bone tissue of the alveolar process.
Traumatic closure of teeth
In the absence of part of the teeth, in case of violation of the position of the teeth, in case of partial destruction of teeth and other traumatic factors, the remaining teeth are subjected to excessive and inadequate load. The latter, in turn, destroys the periodontium of the teeth.
Improper functioning of the temporomandibular joint (TMJ).
The ANS may be a significant factor in the development of gum disease.