What is geographic language
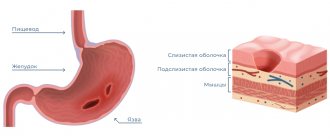
Geographic tongue (desquamative glossitis) is an inflammatory disease of the mucous membrane of the tongue, which is normally covered with small papillae (hairs). With the development of pathology, the latter become deformed, the surface becomes smooth and red. In appearance, the lesions resemble a geographical map with islands.
Inflammatory foci have elevated, clearly defined boundaries. They differ in their ability to heal in one place and move to another. More often there is an alternation of compactions with sagging mucous membranes.
Before prescribing treatment for a disease, it is necessary to accurately determine the causes that led to the pathology and, if possible, eliminate them, since this problem is not only cosmetic in nature, but can also lead to serious consequences.
What is glossitis?
Glossitis is an inflammatory condition of the tongue that is usually caused by a bacterial or viral infection.
This pathology is characterized by a change in the color of the tongue, its structure, color and overall appearance become different. If ulcerative defects form on the tongue, plaque forms or its natural color changes, these act as signals of a disorder. There are several types of glossitis. They differ in symptoms and causes of the pathological process. Sometimes glossitis does not act as an independent disease, but as a consequence of another pathology present in the body. Glossitis is not a harmless disease, as it affects the neck. It develops in both adults and children. Elderly patients often suffer from glossitis. To cope with inflammation, you need to find out the cause of its occurrence. To do this, you should contact your dentist. The doctor will determine the type of disease. If necessary, he will refer the patient to another specialist. Sometimes patients need the help of an infectious disease specialist, gastroenterologist, immunologist, or allergist.
ICD code
ICD-10:
K14.0
ICD-10-CM:
K14.0
ICD-9-CM:
529.0
Causes
Today, the disease is quite common, but despite this, it has not been fully studied, especially the etiology. It was possible to identify a number of reasons that contribute to its development:
- Diseases of the digestive system.
- Pathologies of the thyroid gland.
- Liver diseases.
- Disorders in the circulatory system.
- Malignant and benign tumors.
- Autonomic-endocrine disorders.
- Infectious processes.
- Autoimmune diseases.
- ARVI, ARZ.
- Pathologies of the nervous system.
- Allergic diathesis.
- Pathologies occurring in the oral cavity.
- Hereditary genetics.
- Avitaminosis.
- Chronic skin diseases.
- Stressful situations.
- Diabetes.
- Long-term therapy with antibiotic drugs.
In childhood, desquamative glossitis can manifest itself against the background of general diseases of the liver, kidneys, pancreas, spleen, and desquamative glossitis. In girls, it is more often observed before the first menstruation or during bleeding.
The disease can occur either independently or as a symptom of a concomitant disease. Therefore, it is divided into primary and secondary desquamative glossitis.
Primary glossitis most often occurs when the tongue is injured by sharp edges of teeth or dentures, as well as from chemical or thermal burns. In young children, geographic tongue is diagnosed during teething.
The development of the secondary form occurs as a result of pathological reactions in the human body. This is observed due to increased sensitivity to changes in the mucous epithelium of the tongue. Such changes are promoted by chronic diseases of the liver, gall bladder, severe vitamin deficiency and others. The pathology often begins with colds, scarlet fever, measles, and typhoid fever.
What is a serrated tongue?
Severely uneven edges of the tongue
A scalloped tongue, also known as a scalloped tongue or ragged tongue , is a descriptive term for the appearance of indentations on the sides of the tongue as a result of compression of areas adjacent to the teeth “[Wikipedia.org]. Some people describe these changes as wavy edges , indentations on the sides of the tongue, a grooved or uneven edge, or marks or tooth marks on the sides of the tongue. Whenever the tongue becomes larger than normal, it puts pressure on the teeth and can result in indentations. According to Chinese traditional medicine, “irregularities on the tongue indicate a lack of Qi energy ” [wikipedia.org], while in homeopathy, according to numerous sources, they indicate high blood pressure.
Symptoms
Geographical language is manifested by the following features:
- Cloudiness of the mucous membrane - during the initial development, a whitish coating with a gray tint appears. The lesion is small - no more than three millimeters.
- Detachment of the papillae - with further development, the papillae desquamate, and underneath there is an area of bright red color, which stands out strongly against the general background of the tongue. Such an “island” can grow and move, but the boundaries remain clear.
When the focus becomes as large as possible, the boundaries are not so clearly defined and begin to blur. In the center of the lesion, the mucous membrane takes on a normal state, and along the borders keratinization and peeling (desquamation) are observed. Since the affected areas are capable of displacement, desquamation is layered one on one.
That is, new lesions appear on old lesions, the mucous membrane becomes similar to a geographical map. This process is characterized by the fact that all areas of the tongue are affected, excluding the lower part. And this picture can change daily.
Desquamative glossitis manifests itself without pronounced symptoms, so many people learn about the disease only when examined by a doctor. Occasionally, patients complain of itching and burning, discomfort while eating, and impaired sensitivity to the taste of food.
All about the symptoms and treatment of glossitis
The main symptom of the disease is the appearance of the tongue. Some patients, as a result of the disease, develop a pathological fear for their life, a panicky fear of the appearance of a malignant tumor (cancerophobia).
The development of pathology is influenced by severe stress, and it does not matter what emotions a person experiences: positive or negative. In approximately half of the cases, a parallel course with the folded tongue is observed.
Despite the fact that the pathology does not bring much discomfort, the patient is frightened by the very sight of the affected organ, which is stressful and accordingly worsens the course of the disease.
A feature of desquamative glossitis is its complete disappearance, more often for a long time, but then the symptoms reappear.
What does the tongue tell you about: what diseases are visible on it?
If the eyes are the mirror of the soul, then the tongue for an experienced doctor is the mirror of health. It is not for nothing that when visiting a doctor you are asked to open your mouth and stick out your tongue in order to carefully examine it. Tongue diagnosis is used in traditional medicine in China, India, Vietnam and many other countries. It is carefully assessed by physicians and gastroenterologists, and sometimes neurologists, to determine the onset of a stroke!
This is an important way to diagnose the patient’s health condition, and sometimes the condition of the tongue can be decisive when deciding what to do and which organ to treat first.
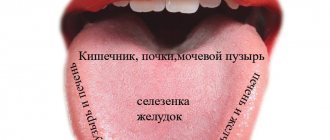
"Map" of the language
On the Internet you can find pictures that show which areas of the tongue are “responsible” for which organs. So, for example, the tip of the tongue is a projection of the heart, and on the sides of it are the lungs. The root of the tongue, where usually the most plaque is found, is the large intestine, which often suffers from inflammatory pathologies and dysbiosis. Thus, if a doctor keeps this “map” of the tongue in his head, he will immediately understand which organs need to be examined first.
Like the sole of the foot, which is used in reflexology, or the earlobe (auriculotherapy), the tongue is a kind of map of the body's organs. Often what language “tells” you about a patient’s health is more important than what other diagnostic methods reveal.
Diagnosis of the tongue, if the doctor has experience in its use, is also quick: he simply looks, notes the changes, the nature of the plaque, the condition of the papillae of the tongue and other characteristics. No need to touch, listen, do x-rays or ultrasound.
When to do a tongue diagnosis
Diagnosis is carried out in good lighting, preferably daylight, because with artificial light you may not be able to see the natural colors and plaque. It is important that the patient does not brush their teeth or tongue before the appointment, and does not eat or drink colored foods. It is not advisable to examine your tongue after exercise or a hot shower; its color may change. Ideally, the patient should drink a few sips of water, rinse his mouth, after which the specialist can examine the tongue. To diagnose the tongue you do not need any additional devices. Sometimes the doctor may scrape the tongue a little with a spatula to examine the plaque.
Almost all internal organs, as well as their biological points, are projected onto the surface of the tongue. This means that you can often "see" how these organs and systems work simply by examining your tongue for a few minutes.
For example, the back of the tongue reflects kidney function, while the front and tip are responsible for the heart. In front of the kidney area is the area of the spleen and stomach, and between them and the heart is the area of the lungs. The sides of the tongue reflect the work of the liver with the gall bladder, gradually moving to the tip in the chest area, including the woman’s mammary glands, heart and lungs.
The way the tongue moves, its shape, color, coating, and how wet or dry it is also important in diagnosis.
Appearance of the tongue
It is important to evaluate the shape of the tongue during examination, paying attention to its general condition. For example, you need to focus on cracks in the tongue. They occur in different places and reflect different health problems. The most common is a longitudinal median fissure, running up the center of the tongue from front to back. If it is wide and shallow, then this usually indicates stomach problems - gastritis and peptic ulcers.
If the crack reaches the tip from the very back of the tongue, this indicates problems with the heart, probably due to severe worry and anxiety. And the redder the tip of the tongue, the worse a person’s sleep and the higher the blood pressure. If cracks appear in the area of the front of the tongue along the projection of the chest, you should look for problems with the bronchi and lungs.
Swelling of the tongue
Swelling of the tongue, as well as swelling anywhere in the body, indicates an inflammatory process or neoplasia. If only one part of the tongue is swollen, this indicates problems in the area whose projection is located in this zone, but this is often possible at high temperatures. For example, if the tip of the tongue swells, this indicates damage to the heart; if the sides are swollen, this means liver inflammation, especially if the area is red. With a recent stroke, the tongue will be uniformly swollen. If swelling occurs with a deep central line, this indicates a nutritional deficiency - due to dieting, fasting, vegetarianism. Additionally, a bare, redder, swollen area at the tip denotes the patient's poor sleep and constant anxiety.
Teeth imprints on the tongue
For problems in the lung area, the tongue is slightly pale, with dental marks on one side. In addition, this is possible with blood pathologies, especially anemia, the presence of sputum in the lungs and lesions of the spleen. Lines from the teeth indicate chronic gastritis. Dental marks on the sides of the tongue can also occur when bile stagnates in the liver. If anemia develops, then the tongue may be thinned, pale or bright red, without a coating.
Tongue color, plaque assessment
If a person is healthy, his tongue has a natural pink color without plaque or any abnormalities. Many pathologies affect the color of the tongue and provoke the formation of plaque.
A pale tongue often indicates anemia, that is, circulatory disorders, or infectious, inflammatory lesions of the body. If the color is pale only in certain areas, it indicates lesions in those areas. Plus, the color of the tongue also depends on the amount of saliva. It provides moisture to the mouth, so if the tongue is dry and pale, it indicates dehydration and lack of fluid in the body. This is typical for various infections and intestinal lesions with diarrhea.
A crimson tongue with prominent papillae may be due to an infection such as scarlet fever, or it may be a sign of hypertension. A purple tongue suggests slow blood movement, venous congestion. The more blue and purple, the worse, similar processes can occur with varicose veins.
No less important is the coating on the tongue - its thickness, color and even smell. It mainly reflects the health of the stomach and digestion in general. In healthy people, in the morning after sleep, before brushing their teeth, a thin white plaque may appear, which can be easily removed with oral hygiene. The tongue itself is smooth, pink in color, without cracks or enlarged papillae. This indicates normal stomach acidity and intestinal function.
If the tongue is covered with a thick, thick white coating, you need to check the stomach: most likely, gastritis or ulcerative defects will be found. In addition, you need to adjust your diet. It is also possible to have such plaque in diseases of the teeth and oral cavity. Another white coating is typical for the acute stage of infectious diseases.
Yellow plaque, especially at the root of the tongue, may indicate damage to the liver and gallbladder, cholelithiasis and problems of the small intestine.
A dark, almost black plaque occurs with fungal infections of the oral cavity, pathologies of the pancreas, liver or intestines, and with some infections. It is also possible for sore throats. A spotted or “geographical” tongue with alternating patches of plaque and normal areas of the tongue can form due to kidney problems, immune disorders and allergies.
Often, the color of the tongue and the coating on it can be affected by medications taken, antibiotics or some other drugs, as well as certain types of foods and drinks - beets, spinach, rhubarb, brightly colored sodas.
Diagnostics
Making a correct diagnosis is not particularly difficult, so any doctor can recognize the geographic language based on the following studies:
- Collection of anamnesis, which is based on the patient’s complaints and examination data.
- General analysis .
- Bacteriological culture to detect pathogenic microorganisms and determine the causative agent of the disease.
- Polymerase chain reaction (determination of the pathogen by DNA).
- Enzyme immunoassay (presence of non-standard antibodies).
- Scraping the mucous membrane of the tongue to identify treponema pallidum (if syphilis is suspected).
- analysis to detect worms.
To differentiate from other diseases, the doctor focuses more on the movement of lesions.
Identification marks
Ulcers, spots, lines on the tongue can also tell a lot to an experienced interpreter. Thus, a curved line running in the middle of the tongue “hints” at a deformation or curvature of the spine.
Enlargement or inflammation of the papillae on the entire surface of the tongue often occurs with gastritis with increased secretion of gastric juice. And, conversely, a smoothed surface of the tongue occurs with gastritis with low acidity, as well as with diseases of the liver and gall bladder. The imprint of teeth along the edges of the tongue indicates poor intestinal function and insufficient digestion of food. The so-called “geographical” language, in which continents and oceans seem to be imprinted, is a sign of food allergies. One crack in the tongue appears with gastritis, and numerous creases appear with fever, diarrhea, diabetes, and anemia.
Treatment
Treatment is primarily aimed at eliminating the cause (problems with the gastrointestinal tract, bad habits, endocrine disorders in the body).
- Sanitation of the oral cavity – treatment of carious teeth, maintenance of oral hygiene.
- Diet – the patient is prescribed a special diet that does not contain foods and drinks that irritate the oral mucosa. For example, hot, spicy and smoked dishes, carbonated and alcoholic drinks and others.
- Quitting tobacco products.
- Local treatment involves the use of antiseptic rinsing solutions. The most commonly prescribed drugs are Chlorhexidine, Miramistin, Furacilin, and potassium permanganate.
- Novocaine blockades - injections into the area of the lingual nerve (10 injections per course).
- Solutions with an analgesic effect - in the presence of ulcers and erosions. Treated with an antiseptic solution using a tampon.
- Preparations to boost immunity: vitamin complexes, immunostimulants, antihistamines.
- Ointments – have a healing and analgesic effect, applied in the form of applications. The specialist often prescribes Actovegin, Kamistad, Lidocaine.
- Antibiotics - when purulent processes are detected in the oral cavity, regional lymph nodes and tissues: Tetracycline, Doxycycline, Rocephin, Suprax and others. In the most advanced situations, surgical intervention is prescribed.
- Mycotic drugs when fungal microorganisms are detected: Lamisil, Nystatin, Exifin.
Some patients with cancerophobia need psychological help; this requires consultation with a psychologist or psychotherapist.
Causes of glossitis
As mentioned above, glossitis can act as an independent disease, or it can be the result of a pathology of the body. Bacteria (streptococci and staphylococci), herpes viruses and fungal flora can provoke the inflammatory process.
If the disease is non-infectious in nature, then a tongue injury can serve as the impetus for its development. It can be injured by fragments of teeth, sharp edges of dentures or fillings. The tongue is a delicate organ; chemical irritants, as well as exposure to high temperatures, can damage the integrity of its membranes. The likelihood of developing glossitis increases in people who abuse alcohol and smoke a lot.
Other risk factors for developing glossitis include:
- Consumption of hot foods and drinks, spices and caramel
- Poor oral hygiene
- Using mouth fresheners or toothpaste too often and in excess
- Using someone else's toothbrushes
- Wearing braces and dentures
- Piercing the tongue to place earrings in it
Glossitis can be a consequence of pathologies such as:
- Vitamin deficiency (E, A, B12, folic acid)
- Diseases of the dermis
- Dry mouth
- Anemia
- Measles and scarlet fever
- Diphtheria
- Diseases of the digestive system
- Infection with worms
- Lichen planus
- Allergy
- Stomatitis
- Rheumatism
- Uncontrolled use of antibacterial drugs.
The chronic form of the disease can be triggered by dysbiosis or a general decline in the body's immune forces. At the same time, it produces autoantibodies that increase inflammation.
Statistics indicate that glossitis most often develops in men over the age of 40. However, when the tongue is exposed to traumatic factors (burn, trauma, chemical damage), the disease manifests itself at any age.
Glossitis rarely develops only under the influence of a single factor. Most often, they appear in combination, when a person has diseases of the oral cavity and disturbances in the functioning of the gastrointestinal tract, then an injury or burn can trigger the onset of inflammation. If the tongue is constantly influenced by chemical factors, then the likelihood of developing glossitis increases.
Complications
The development of desquamative glossitis should not be ignored, and if detected, you should seek the help of a specialist. Many patients, having discovered a similar pathology in themselves, mistakenly take it for a cancerous tumor, although in fact the geographical language has nothing in common with it.
This benign disease does not have a tendency to become malignant; it is treated by a dentist and a gastroenterologist; in serious cases, an examination by a hematologist, gastroenterologist and endocrinologist is required.
If therapeutic measures to eliminate the geographic tongue are not carried out in a timely manner, the disease takes on a more advanced form with relapses and will be more difficult to treat. In addition, there is a risk of swelling of the tongue, which adversely affects breathing; chewing and swallowing functions are also affected. Next, the process involves regional tissues and organs.
Is it worth diagnosing by tongue?
Doctors have been studying the question of what diseases can be identified by language for several hundred years. The results of research by ancient and modern scientists show that this connection exists, but it must be properly understood and assessed. If a healthy person has irregularities or the color of the plaque has changed, this phenomenon may be the very first symptom of a disease that will manifest itself in the future with other abnormalities.
There is an assumption that the imprints of the disease appear on this organ several days before its clinical signs, but you should not use diagnosis by a person’s tongue for further self-medication. This is a whole science, and only a good specialist can understand it. Treatment can begin only after a full examination and establishment of a correct diagnosis.
Prevention
To prevent the development of such a disease, you need to follow some simple preventive rules:
- Promptly treat all diseases that provoke the development of pathology.
- Do not abuse alcoholic beverages, tobacco products, sweet foods and sugar, and strong coffee.
- Take enough vitamins to avoid vitamin deficiency.
- Perform hygiene .
- Treat caries in a timely manner.
There are separate preventive measures for children:
Caring for baby teeth – timely treatment and removal of baby teeth. If a child complains of dry mouth, rinse with herbs such as sage, St. John's wort or chamomile.
Brushing your teeth should be done only with toothpastes, since the powders contain mint oil and menthol, which are bad for the oral mucosa in children.