Functions of the sky and structural features
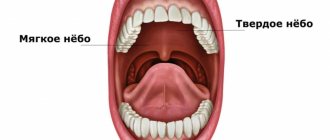
The palate is a vault that separates the oral cavity from the nasopharynx. The structure of the palate consists of two sections - hard and soft. This organ performs an important function - it prevents food from entering the nasopharynx from the oral cavity.
In addition, receptors on the surface of the palate are associated with the larynx and take part in articulation and influence the timbre of the voice and the pitch of sounds. Thus, the inflammatory process of the upper palate disrupts all the functions of this important organ, and therefore requires mandatory treatment.
How and where to treat a cleft palate?
Cleft palate surgery and cosmetic facial plastic surgery can eliminate external defects and restore the functionality of the oral and nasal cavities in a newborn (questionable, the operation is performed at the age of two years).
During the surgical operation, the palatine and pharyngeal muscles are connected in the correct position, the integrity, normal shape and functioning of all structures are restored. The extent of surgical interventions and the appropriate age for this are determined by the type of anomaly and the complexity of the case. After a thorough examination of the baby by the surgeon, one of the treatment tactics for children with cleft palate is selected:
- Uranoplasty (corrective surgery) from the age of 2 years – for incomplete clefts in children with regular upper jaw dentition.
- Uranoplasty at 4-6 years of age with preoperative orthodontic therapy - with a narrowed upper jaw and clefting, including the alveolar process.
- Two-stage correction (soft tissue plastic surgery with narrowing of the pharynx and, 6-8 months later, surgery on the hard palate with the alveolar process with simultaneous bone grafting).
Why does inflammation occur?
The muscular structure of the palate is covered on top with a mucous membrane, which is subject to the development of an inflammatory process. Inflammation often occurs under the influence of such factors:
- burn of the mucous membrane as a result of consuming excessively hot food and drinks;
- damage to the palate due to dental diseases - periodontitis, stomatitis, caries, pulpitis;
- disruption of the oral environment due to the action of metals - when wearing braces or installing crowns;
- smoking;
- allergic reactions to medications;
- neurological diseases affecting the joints of the upper or lower jaw;
- osteomyelitis - an infectious lesion of the bone tissue of the jaw;
- malignant neoplasms;
- infectious diseases of the upper respiratory tract - sore throat, tonsillitis, pharyngitis, rhinitis.
The development of the inflammatory process of the palate may be facilitated by some of these causes in their entirety or separately from each other.
FREE CONSULTATIONS!
We are pleased to announce the start of free admission at the Konstanta Clinic for patients under 18 years of age by maxillofacial surgeon, pediatric surgeon L.A. Eremeyshvili. for questions:
- Congenital facial pathologies: cleft lip and palate;
- Benign neoplasms of the face and oral cavity;
- Diseases of the temporomandibular joints;
- Pathology of the frenulum of the oral cavity: lips and tongue.
Correction (plasty) of tongue frenulum is provided free of charge for children under 1 year of age.
*Valid for residents of Yaroslavl and the Yaroslavl region.
You can make an appointment by phone or through the website (4852) 37-00-85 Daily from 8:00 to 20:00
Sign up for a consultation
Congenital cleft palate or cleft palate is a fairly common malformation of the facial region. This pathology is ranked 4th among all developmental defects, and it is diagnosed with a frequency of 1:700 births. Often, a cleft palate is not an independent deviation, but part of a hereditary syndrome.
Signs and symptoms of inflammation of the palate
Depending on the causes of inflammation in the oral cavity, a person may experience the following unpleasant symptoms:
- A feeling of acute pain that makes it difficult to eat. Soon the pain increases, sometimes even swallowing becomes impossible.
- If the inflammation is caused by the action of a fungus, a white coating and erosion forms on the surface of the palate. The process is accompanied by an unpleasant putrid odor from the mouth.
- When the cause of inflammation is an infectious lesion - sore throat or tonsillitis, the palate becomes red and swollen.
- In case of acute inflammation, an increase in body temperature and fever is possible.
- If the cause is dental disease, the patient will be bothered by toothache.
- With cancer, the patient complains of aching pain in the palate.
What to do if your palate hurts. Treatment methods
First of all, it is necessary to treat exactly what served as the impetus for the development of the pathological process. As part of supportive symptomatic therapy, special solutions for oral baths and mouth rinses are usually prescribed. These may be antibacterial, anti-inflammatory or antifungal agents, depending on the nature of the problem.
Gels and ointments are also often prescribed for external use, with a similar therapeutic effect or, for example, antihistamine action, if swelling, redness and itching are an allergic reaction. If a serious infection occurs, your doctor may prescribe antibiotics. It is important to remember that only a professional doctor can select adequate treatment in your particular case.
Various gels may be prescribed for treatment
How is inflammation of the palate treated?
How to treat inflammation on the roof of the mouth, a specialist will tell you after determining the diagnosis. The following therapy methods can be used:
- If the cause of inflammation is minor damage to the mucous membrane, rinsing with decoctions of medicinal herbs is usually sufficient. Decoctions and infusions based on calendula, sage and chamomile have an antiseptic and healing effect. The herbal decoction for rinsing should be used warm.
- When the palate is affected by a fungus, patients are prescribed topical agents. The most effective are the solution and gel “Chlorhexidine”, “Rotokan” or “Stomatofit”.
- In case of severe pain symptoms, regardless of the cause of inflammation, drugs of combined action are prescribed. “Cholisal-gel” and “Kalgel” have proven themselves well.
- If a purulent inflammatory process is detected in the oral cavity, the patient is prescribed antibiotics. The minimum course of treatment is usually 7 days, but there are also stronger drugs that only need to be taken for 3 days. Along with local agents, antibacterial drugs for internal use - Sumamed, Flemoxin Solutab - can be prescribed.
- The inflammatory process of the palate is easily treatable. The earlier therapy is carried out, the less likely it is to develop complications.
Key Causes of Palate Pain in the Mouth
Although there can be many causes for pain and discomfort in the palate, there are a number of common factors observed in more than 95% of symptomatic manifestations. These include:
- The development of a bacterial infection (stomatitis), causing hyperemia and swelling of the palate. Accompanied by the appearance of a specific dirty-gray plaque, ulcers and erosions on the mucous membrane, as well as bad breath;
- Pathologies of the salivary glands, provoked by the penetration and development of infection;
- Neuralgia and pathologies of the jaw joints - pain is felt both in the palate and in other parts of the oral cavity;
- Pathologies of the tonsils, tonsillitis, tonsillitis - in terms of their symptom complex, they have a similar manifestation to a bacterial infection. If not treated in a timely manner, they can cause serious consequences for human health, including: polyarthritis and myocarditis;
- Non-compliance or improper compliance with oral hygiene: mechanical injuries from a toothbrush, burns of various etiologies (physical, chemical, thermal), as well as other injuries received due to negligence;
- Unprofessional dental treatment that caused mechanical injuries to the palate, gums and bone tissue;
- Benign and malignant neoplasms. Benign formations can dissolve and burst, causing the appearance of small painful wounds;
- Leukoplakia or a precancerous condition, accompanied by discomfort in the palate, injuries to the mucous membrane and temperature fluctuations;
- A number of dental problems: pulpitis, periodontitis, advanced forms of caries, periodontal disease, etc.
Most often, the appearance of pain and discomfort in the palate is caused by advanced dental problems that have not received timely diagnosis and adequate treatment. The patient should know what to do if the palate in the mouth hurts! It is worth seeking help from professional dentists; they will determine the cause and prescribe adequate treatment.
Prevention measures
Preventive measures come down to following simple rules:
- brush your teeth at least twice a day; - use mouth rinses every time after meals; - Avoid eating excessively hot food; — enrich the diet with vitamins and microelements to increase local immunity.
Elimination of stressful situations, a balanced diet, regular visits to the dentist and examination of the body - all these actions are reliable prevention of the development of inflammatory processes in the oral cavity.
How to treat inflammation of the palate depends on the causes of the development of the inflammatory process and its symptoms. To determine an accurate diagnosis, you should visit the dentist's office.
This article is for informational purposes only, please consult your doctor for details!
Embryology
Rice.
1. Frontal section of the head of a human embryo (according to L.I. Falin): a - seven-week-old embryo (1 - nasal septum, 2 - tongue, 3 - palatine process of the upper jaw, 4 - ventral cartilage of the lower jaw); b — embryo of eight weeks (1 — nasal septum, 2 — palatine processes of the upper jaw have taken a horizontal position and are located above the tongue, 3 — the tongue has moved down, 4 — ventral cartilage). The formation of the palate begins at the 6-7th week of intrauterine development with the formation of lamellar projections - palatine processes - on the inner surface of the maxillary processes (see Face). The latter are initially directed downward, later taking a horizontal position (Fig. 1, a, b). At the end of the 8th week. During intrauterine development, the edges of the palatine processes fuse with each other and with the nasal septum. Fusion begins from the anterior parts of the palatine processes and gradually spreads posteriorly. In the posterior part of the oral cavity, the palatoglossal and velopharyngeal arches are formed from the palatine processes.
Anatomy
The palate is divided into the anterior section - the hard palate (palatum durum) and the posterior section - the soft palate (palatum molle).
Solid sky
It is represented by the bony palate (palatum osseum), covered with a mucous membrane with a submucous base, the severity of the cut in different parts of the solid N. is different. The bony palate is formed by the palatine processes of the upper jaws (processus palatinus maxillae) and the horizontal plates of the palatine bones (laminae horizontales ossis palatini). The right and left halves of the bone N. are connected by a median palatine suture (sutura palatina mediana), along which a palatine ridge (torus palatinus) protruding towards the oral cavity often runs. At the anterior end of this suture there is an incisive fossa (fossa incisiva), into which the incisive canal (canalis incisivus) opens. In the posterolateral areas of the bone N., at the junction of the upper jaw and palatine bone, a large palatine opening (foramen palatinum majus) is formed. In the horizontal plate of the palatine bone next to the greater one there are small palatine foramina (foramina palatina minora). All openings lead into the greater palatine canal and further into the pterygopalatine fossa (see). The palatine grooves (sulci palatini), separated by the palatine spines (spinae palatinae), run forward from the greater palatine foramen.
Along the midline of the mucous membrane of the hard N. there is a suture of the palate (raphe palati), on which behind the incisors, corresponding to the incisive fossa, is the incisive papilla (papilla incisiva). On the sides of the anterior section of the suture there are transverse palatine folds (plicae palatinae transversae), more pronounced in children.
The submucosa is present in the lateral sections of the N., on the border with the soft N.; in the area of the suture and at the transition of the N. mucous membrane to the gum, it is absent. In the anterior sections of the N., the submucosa contains a small amount of adipose tissue, penetrated by thick tufts of dense fibrous connective tissue, between which vessels and nerves pass. In the posterior sections of the solid N., this layer is occupied by the mucous palatine glands. The shape of the bone N. is related to the shape of the skull and face.
Rice. 2. Schematic representation of the muscles of the soft palate: 1 - muscle that strains the velum palatine, 2 - muscle that lifts the velum palatine, 3 - hook of the pterygoid process, 4 - palatoglossus muscle, 5 - uvula muscle, 6 - velopharyngeal muscle.
Soft sky
It is represented by the palatine aponeurosis, into which the muscles of the soft palate and pharynx are woven. With calm breathing and muscle relaxation, the soft palate hangs vertically, forming the so-called. palatine curtain (velum palatinum). In the middle of its rear edge there is a protrusion - a tongue (uvula). Soft N. includes the following muscles (Fig. 2): the muscle that strains the velum palatini (m. tensor veli palatini), the muscle that lifts the velum palatini (m. levator veli palatini), and the muscle of the uvula (m. uvulae). The terminal parts of the palatoglossus muscle (m. palatoglossus) and the velopharyngeal muscle (m. palatopharyngeus) are woven into the soft N. The muscle that strains the velum palatine is a pair, it begins with wide muscle bundles from the spine of the sphenoid bone (spina ossis sphenoidalis), from the membranous part of the Eustachian (auditory, T.) tube (tuba auditiva), from the scaphoid fossa (fossa scaphoidea) and the medial plate of the pterygoid process (lamina med. processus pterygoidei). The muscle bundles, converging, descend vertically downwards, the resulting tendon is thrown over the pterygoid hook (hamulus pterygoideus). Then, taking a horizontal direction, these tendon bundles, together with the tendon bundles of the opposite side, form the palatine aponeurosis, which is attached to the posterior edge of the hard N.
The muscle that lifts the velum palatine, also paired, starts from the lower surface of the pyramid of the temporal bone, anterior and medial from the external opening of the carotid canal (canalis caroticus) and the cartilaginous part of the Eustachian tube; approaching the midline, it intertwines with bundles of the muscle of the same name on the opposite side.
The uvula muscle is a paired muscle that starts from the N. aponeurosis and ends at the tip of the uvula; shortens and raises the tongue. The palatine muscle is a continuation of part of the bundles of the transverse muscle of the tongue (m. transversus linguae), at the root of the tongue it rises along the posterior part of the side wall of the mouth and is woven into the soft palate; the muscle forms the thickness of the palatine arch (areus palatoglossus), when contracted, it lowers the palatine curtain and reduces the diameter of the pharynx.
The velopharyngeal muscle is a steam muscle, located in the lateral wall of the pharynx, starting from the posterior wall of the pharynx and the thyroid cartilage of the larynx and, moving upward, is woven into the lateral sections of the velum palatine. The muscle forms the velopharyngeal arch (areus palatopharyngeus) and, when contracted, lowers and pulls back the palatine curtain and narrows the pharynx. Between the arches are the palatine tonsils (see).
Soft N. is covered with a mucous membrane, which has a submucosa containing mucous and mucoserous glands.
Rice. 3. Schematic representation of the blood supply and innervation of the palate: 1 - incisive canal, 2 - nasopalatine nerve, 3 - greater palatine nerve, 4 - greater palatine foramen, 5 - lesser palatine foramina, 6 and 7 - branches of the lesser palatine nerve, 8 - palatine tonsils , 9 - small palatine arteries, 10 - greater palatine artery, 11 - anastomosis with the incisive artery.
Blood supply
the palate (Fig. 3) is carried out by the maxillary artery (a. maxillaris) and the facial artery (a. facialis). The descending palatine artery (a. palatina descendens) departs from the maxillary artery, and from it to the hard nerve through the greater palatine foramen - the greater palatine artery (a. palatina major). This artery lies in the groove at the site of the transition of the hard N. to the base of the alveolar process, gives off branches to the mucous membrane of the hard N., and its terminal branches anastomose with the incisive artery (a. incisiva), emerging from the incisive canal. The incisive artery is terminal. It is formed from the posterior nasal lateral and septal arteries of the nose (aa. nasales post, laterales et septi), extending from the maxillary artery.
In addition, the small palatine arteries (aa. palatinae minores)—branches of the descending palatine artery—exit the hard palatine from the small palatine foramina, located posterior to the greater palatine foramen. The soft N. is supplied with blood through the ascending palatine artery (a. palatina ascendens), which extends from the facial artery.
Venous outflow occurs through the palatine vein (vena palatina), which originates in the thickness of the soft tissue, passes through the bed of the palatine tonsil and most often flows into the facial vein. Other veins drain into the pharyngeal venous plexus.
Innervation
carried out by the second branch of the trigeminal nerve due to the greater palatine nerve (n. palatinus major), emerging from the greater palatine foramen, and the small palatine nerves (nn. palatini minores), emerging through the small palatine foramina, as well as the nasopalatine nerve (n. nasopalatinus), exiting through the incisive foramen. The motor innervation of the soft nerve is carried out by the branches of the IX and X pairs of cranial nerves. The muscle that strains the velum palatine is innervated by the mandibular nerve (n. mandibularis).
Lymphatic drainage
occurs to the deep cervical lymph nodes (nodi lymphatici cervicales profundi), retropharyngeal nodes (nodi lymphatici retropharyngei), as well as to the submandibular lymph nodes (nodi lymphatici submandibulares).
Traditional medicine for pain in the palate
Pain in the palate causes discomfort and interferes with the usual way of life. Infusions from decoctions of medicinal herbs will help reduce pain, relieve swelling and alleviate the general condition.
| Name | Description |
| Onion peel decoction | For 3 tablespoons of chopped onion peel you will need half a liter of water. The composition is brought to a boil, then put in a dark place for 8 hours. Before rinsing, the broth should be strained and used 2-3 times a day. |
| Horse sorrel solution | Horse sorrel roots need to be chopped. For a glass of boiling water you will need one tablespoon. The solution is brought to a boil over heat and boiled for 15 minutes, filter and rinse the mouth. |
| nettle leaves | Finely chopped nettle leaves in the amount of 1 tablespoon are poured into two glasses of boiled water. You need to let the product sit for half an hour and strain. Such rinses help if ulcers on the mucous membrane do not heal well. |
| Collection of herbs | Ingredients required for preparing the infusion: salvia officinalis – 1 glass; calendula flowers – 1 cup; 1.5 glasses of water. Place finely chopped herbs in an enamel bowl and fill the contents with water. After thorough mixing, the pan should be placed in a water bath. Boil the infusion covered for about 10 minutes, then cool and strain. The solution is ready for rinsing. They need to be done several times a day. |
Using traditional medicine you can temporarily relieve pain
There are many other simple recipes to relieve pain.
- Combine 1 teaspoon of onion juice with 1 teaspoon of Kalanchoe juice and 3 tablespoons of water. After mixing, rinse your mouth for 1-3 minutes.
- A decoction of plantain will help eliminate ulcers. To prepare, grind 2 tablespoons of herbs, pour two glasses of boiling water over them and leave. Strain before rinsing; the broth should be warm.
Histology
The mucous membrane of solid H. is covered with stratified squamous keratinizing epithelium. In the epithelial layer, the basal, spinous, granular and stratum corneum are clearly distinguished. The stratum corneum is formed by several rows of completely keratinized cells (without nuclei). Glycogen is not normally detected in the epithelium of solid N., but it can accumulate here when the process of keratinization is weakened (for example, when wearing laminar dentures for a long time). The basal and spinous layers are characterized by high activity of redox enzymes. The connective tissue basis of the mucous membrane of solid N. consists of fairly dense connective tissue; Some of the bundles of its collagen fibers are directly woven into the periosteum of the palatine bones, especially in those areas where there is no submucosa, due to which the mucous membrane is tightly fixed to the bone. In the area of the palatal suture and when the N. passes into the gum, the submucosa is absent; throughout the rest of the solid N., a clearly defined submucosa is revealed in the mucous membrane. In the anterior section of the N., on the sides of the palatine suture, the submucosa is represented by an accumulation of adipose tissue, and in the posterior section by an accumulation of small mucous glands.
The mucous membrane of the anterior surface of soft N. is covered with multilayered squamous non-keratinizing epithelium. The cells of the spinous layer of the epithelium contain a large amount of glycogen; They are also characterized by high activity of enzyme systems. The lamina propria of the mucous membrane consists of relatively thin interwoven bundles of collagen fibers; At the border with the submucosa there is a massive layer of elastic fibers. The submucosa is represented by loose connective tissue, which contains the end sections of small mucous glands. The posterior surface of the soft N. is covered with multirow ciliated epithelium, characteristic of the respiratory tract. Both surfaces of the uvula in adults are covered with stratified squamous non-keratinizing epithelium, rich in glycogen. In newborns, on the posterior surface of the uvula there is a multi-row ciliated epithelium, which is replaced by multi-layered epithelium during the first month of life.