Bitterness in the mouth may indicate problems with the digestive system. Severe or persistent bitterness in the mouth is a reason to consult a doctor.
From time to time you may experience an unpleasant bitter taste in your mouth. As a rule, this is due to a sudden release of bile into the gastrointestinal tract. In this case, some bile may enter the esophagus and cause a bitter sensation in the mouth.
. Often a bitter taste in the mouth is felt in the morning, since bile can enter the stomach during sleep (especially if you sleep on your left side and dinner included fatty foods).
Bile is a secretion produced by the liver and is necessary for digesting food. The bile duct carries bile from the liver to the gallbladder, which acts as a storage reservoir. During the active digestive phase, bile from the gallbladder enters the duodenum. Some substances have choleretic properties, that is, they increase the production of bile. Eating foods with choleretic properties (for example, pine nuts) can provoke a sharp increase in the flow of bile into the intestines and, as a result, the appearance of bitterness in the mouth. Some medications have the same effect - both medical preparations and traditional medicine (St. John's wort, sea buckthorn oil, etc.).
However, bitterness in the mouth should not be ignored
. Its appearance indicates that not everything is in order with the digestive system. For example, a bitter taste may appear after eating fatty (heavy) foods. Fatty foods stimulate bile secretion. Normally, the secreted bile should not enter the stomach and esophagus, but should be released exactly as much as is necessary for the digestive process in the intestines. The appearance of bitterness indicates that this is not the case. And we need to figure out what caused this. If bitterness in the mouth occurs frequently or persists for a long time, then it is better not to delay a visit to the doctor.
Causes of bitterness in the mouth
Bitterness in the mouth can be a symptom of various diseases.
Most often it is caused by diseases of the organs responsible for the production and movement of bile in the body, such as chronic cholecystitis
(inflammation of the gallbladder),
cholelithiasis
(in this case, the formation of stones interferes with the proper outflow of bile),
biliary dyskinesia
(impaired motility). Sometimes patients who previously had a bitter taste in the mouth due to cholelithiasis or inflammation of the gallbladder, and who had a cholecystectomy (surgery to remove the gallbladder), are surprised by the return of the symptom. But a bitter taste in the mouth can occur even in the absence of a gallbladder, because bile is still produced and can enter the stomach, and from it into the esophagus. If a person has had their gallbladder removed but has not changed their eating habits, the return of digestive problems and a bitter taste in the mouth is very likely
Bitterness in the mouth can occur with various disorders of the digestive system, for example with chronic gastritis
or
chronic pancreatitis
Liver diseases can lead to changes in the composition of saliva, which may also result in a bitter taste in the mouth.
Another group of reasons for the feeling of bitterness in the mouth is diseases of the oral cavity (stomatitis, inflammation of the tongue). A bitter taste can also be a reaction to dentures if they were chosen incorrectly (the individual intolerance of the material from which they are made was not taken into account).
Sometimes bitterness in the mouth is caused by other reasons: toxicosis (in pregnant women), acute poisoning, cancer.
Why do expectant mothers so often complain of heartburn and indigestion?
There are two main causes of heartburn and indigestion during pregnancy:
Hormonal changes in the body of the expectant mother
During pregnancy, the amount of progesterone produced increases, causing muscle relaxation. Accordingly, increased production of progesterone provokes relaxation of the muscles of the lower esophageal sphincter. The sphincter is a ring of muscle that prevents stomach contents from entering the esophagus. As a result, when the sphincter muscles relax, the contents of the stomach (including gastric juice) can freely pass into the esophagus, causing irritation of its mucous membrane. The esophageal mucosa is not designed to accept large amounts of gastric acid for a long time. This is why we feel pain.
Child's height
As your baby grows, it begins to put more and more pressure on the organs of your digestive tract, stomach and intestines. This pressure can cause stomach acid to flow into the esophagus.
Most often, problems with the digestive system during pregnancy are faced by those who had similar problems before pregnancy, as well as those for whom this is not their first baby.
Heartburn and indigestion can also be caused by other reasons. For example, some foods and drinks also cause excessive stomach acid production, which can destroy the protective lining of the stomach. The protective layer is the mucous membrane, which is in direct contact with the contents of the stomach, including gastric juice. If its destruction occurs, it can lead to discomfort and unpleasant sensations.
Additional symptoms of bitterness in the mouth
Bitterness in the mouth may be accompanied by additional symptoms. If heaviness or pain is felt in the right side, this may indicate liver or gallbladder disease. If bitterness in the mouth is accompanied by nausea, heartburn, and belching, then the cause may be stomach diseases. If the cause is diseases of the oral cavity, then the feeling of bitterness may be accompanied by bad breath.
Acid-dependent diseases during pregnancy
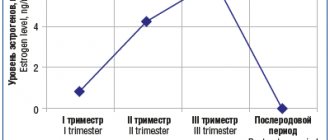
Heartburn during pregnancy is a very common complaint. It is known that up to 80% of pregnant women experience symptoms characteristic of gastroesophageal reflux disease (GERD) (heartburn, dysphagia, belching and others), and the frequency of heartburn in the first trimester is 7.2%, in the second - 18.2%, in the third - 40%.
The main factors responsible for such a high prevalence of GERD during pregnancy include hormonal changes, such as hyperprogesteronemia (increased levels of the hormone progesterone) and hyperestrogenemia (increased levels of estrogen hormones), as well as increased intra-abdominal pressure due to the growth of the uterus and fetus.
The effect of gestational hormones in the first trimester of pregnancy is due to the fact that, without affecting the basal tone of the lower esophageal sphincter (LES), they reduce the increase in pressure of this sphincter in response to various physiological stimuli, including food intake. In the second and third trimesters of pregnancy, progesterone and estrogen reduce the basal tone of the LES to 50% of the initial level, the maximum reduction occurs at the 36th week of gestation. After successful delivery, the tone of the LES in women who did not suffer from GERD before pregnancy, as a rule, returns to normal - in connection with this, this condition is called “pregnant heartburn”.
Heartburn in pregnant women usually does not lead to the development of esophagitis, complications of GERD (strictures, ulcers, bleeding) and does not require serious drug treatment.
If a woman suffered from GERD before pregnancy, during gestation the complaints may worsen and require examination and drug treatment.
The diagnosis of GERD during pregnancy is established primarily on the basis of complaints, medical history and objective examination. X-ray examination in pregnant women - due to a possible damaging effect on the fetus - is not used; pH-metry and manometry can be used, but the need for its use is doubtful.
Esophagogastroduodenoscopy (EGD) is the method of choice for diagnosing GERD in pregnant women, but it should be used only for strict indications, such as a history of complications of GERD and the ineffectiveness of drug therapy.
Treatment of GERD in pregnant women should be based on changes in lifestyle and nutrition: avoiding a horizontal body position immediately after meals, sleeping with the head of the bed elevated (15 cm), avoiding physical activity that increases intra-abdominal pressure (including wearing corsets, tight belts, bandages). The last meal should take place no later than 3 hours before bedtime, you need to eat in small portions, and pay special attention to normalizing stool.
First-line drugs for the treatment of GERD in pregnant women include antacids and alginates. If these drugs are ineffective, it is permissible to prescribe prokinetics (metoclopramide), histamine H2 receptor blockers and (if strictly indicated) proton pump inhibitors (PPIs).
H2-histamine blockers are the most commonly prescribed group of drugs for pregnant women. They are classified as risk category B by the US Food and Drug Administration (FDA) (“drugs that have been taken by a limited number of pregnant women without evidence of an effect on the incidence of congenital anomalies or harm to the fetus”). Russian instructions allow only cimetidine and ranitidine with the caveat: use during pregnancy is possible only if the expected effect of therapy exceeds the potential risk to the fetus. Famotidine and nizatidine are contraindicated in the Russian Federation for pregnant women.
Despite the fact that the FDA also classifies most PPIs as risk category B, in Russia there are stricter restrictions on the use of this group of drugs in pregnant women. Thus, lansoprazole is contraindicated in the first trimester; in the second and third trimesters, its use is possible only if the expected benefit of therapy outweighs the potential risk to the fetus. The use of pantoprazole and esomeprazole is possible only under strict indications, when the benefit to the mother outweighs the potential risk to the fetus. Rabeprazole is contraindicated during pregnancy.
Pregnancy has a beneficial effect on the course of peptic ulcer disease: 75–80% of women experience remission of the disease, and it does not have a noticeable effect on its outcome. However, some patients may experience an exacerbation. Most often this is observed in the first trimester of pregnancy (14.8%) and the third trimester (10.2%), as well as 2–4 weeks before the due date or in the early postpartum period. Uncomplicated peptic ulcer disease does not have a negative effect on fetal development.
Treatment of peptic ulcer in pregnant women includes adherence to generally accepted “regime” measures and diet; taking non-absorbable antacids in usual therapeutic doses (1 sachet 3 times a day 1 hour after meals and adsorbents 1 sachet 3 times a day 1 hour after meals). If there is no effect, H2-blockers are prescribed (ranitidine 150/300 mg once at night); if they are insufficiently effective, as well as if complications develop, we can take PPIs (omeprazole 20–40 mg, lansoprazole 30–60 mg, pantoprazole 40 mg). mg, in the morning before the first meal). Bismuth preparations are contraindicated for pregnant women. Eradication therapy for H. pylori infection is not carried out in pregnant women.
Nutrition during pregnancy
Organization of nutrition during the perinatal period is aimed at maintaining the health of the woman and ensuring the harmonious development of the baby. The main tool in achieving the goal is the responsible attitude of the expectant mother to her daily diet. Poor nutrition during pregnancy results in nutritional deficiency. This leads to the occurrence of intrauterine pathologies, complications of gestation, increases the chances of the child developing autoimmune reactions, and activation of unfavorable genetics (hereditary predisposition to diseases).
The causes of nutritional imbalance in the body of a pregnant woman are:
• Calorie deficit and surplus. The low energy value of the diet forces the baby’s body to turn on the mechanism of accelerated absorption of everything that the mother eats. Nutrigeneticists claim that the habit of eating everything continues after birth, threatening obesity. In the female body, a lack of calories is reflected in the weakness of the uterine muscles. There is a danger of miscarriage. Excess calories lead to excess weight gain, and this puts stress on joints, blood vessels, and the risk of developing gestational diabetes mellitus, hypertension, and varicose veins. • Lack of vitamins. Hypovitaminosis during pregnancy is a direct threat to the life and health of the child. Deficiency of vitamins A and E slows down fetal growth and provokes premature birth. Deficiency of B1, B9 causes defects in the development of the nervous system. Vitamin D deficiency is the cause of neonatal rickets and visual impairment. Hypovitaminosis B2 results in heart defects, cleft palate, and deformation of the arms and legs of a newborn. • Lack of minerals. Microelements participate in embryonic development no less than vitamins. Copper deficiency leads to a decrease in the immune status of mother and child, calcium, phosphorus - to demineralization of fetal bone tissue, iodine - to a delay in the neuropsychic development of the baby, iron - to iron deficiency anemia in a pregnant woman, the threat of miscarriage, magnesium - to premature birth, development arrhythmias in the mother, zinc - to slow growth of the embryo.
Eating right means ensuring your child’s stable growth and development, and protecting yourself from perinatal risks and complicated childbirth. A pregnant woman needs to eat not “for two,” but “for two.”
Approximate vitamin and mineral norm per day (in mg)
Minerals
- calcium - 1200
- phosphorus - 700
- magnesium – 360
- iodine - 200
- zinc - 15
- iron - 30
- copper - 2-3
Vitamins
- retinol (A) - 1.2
- thiamine (B1) - 1.8
- pyridoxine (B6) - 2.1
- folic acid (B9) - 400 mcg
- tocopherol (E) – 10
- ergocalciferol (D) – 500IU
- ascorbic acid (C) – 100
To prevent vitamin and mineral deficiency, it is recommended to supplement your diet with special vitamins for pregnant women.
Features of the treatment of unpleasant taste in the mouth during pregnancy
To understand how to get rid of sour or any other notes on the tongue during pregnancy, you need to know the cause of this phenomenon, which is usually found out after a detailed diagnosis. Treatment is based on a mandatory diet and the use of medications (if a strange taste is the cause of any disease).
Diet for an unpleasant taste in the mouth during pregnancy
Regular meals and a varied diet contribute to a successful pregnancy and are a reliable prevention of various diseases that affect the change in taste in the expectant mother. Nutritionists suggest: in such a situation, it is good to satisfy your hunger with slimy soups, mashed potatoes, oatmeal and rice porridge. The diet must certainly include dairy products (milk, cream), as well as homemade, moderately sweetened compotes and jelly. But it is better to avoid sweets, bread, various spices, sour and pickled foods, radishes and fatty first courses.
Let us recall the general principles of healthy eating during pregnancy:
- Smoked and fried foods are only harmful, so their presence in the diet during pregnancy is unacceptable.
- Cabbage and legumes can only be eaten in very modest portions.
- Vegetables, herbs and fresh fruits should always be present on the expectant mother's plate.
- Lean varieties of meat and fish are a priority.
- You can’t give up buckwheat, apples, seaweed, pomegranate seeds and liver. These are rich sources of iron.
Medicines for bad taste in the mouth during pregnancy
Depending on what disease is causing the change in taste in the expectant mother’s mouth, the doctor may decide to use the following groups of medications:
- vitamins;
- antiseptics;
- antibiotics;
- iron-containing preparations;
- enzymes;
- antisecretory drugs;
- prokinetics;
- drugs that regulate blood sugar levels;
- anti-inflammatory.
It is possible to understand what caused the unusual taste in the mouth only after a comprehensive examination of the pregnant patient. Practice shows that this condition is not always a consequence of any pathology. In this way, the female body reacts to bearing a child, and after giving birth the new mother’s well-being quickly improves.
Prevention measures
Is it possible to prevent the strange taste from occurring? Some tips for prevention:
- Changing your diet. During pregnancy, a woman needs to monitor her food intake. Minimize the content of fatty, fried and smoked foods in the menu. It is better to make small portions, but eat them at intervals of 2-3 hours. It is recommended to drink a sufficient amount of fluid (in the early stages - at least 1.5 liters, in the later stages - at least 1 liter).
- Regular visits to the dentist. The cause of unpleasant odor and taste in the mouth may be diseases of the teeth and gums. You should rinse and brush your teeth after every meal.
- Rejection of bad habits. Smoking and alcohol are strictly contraindicated for pregnant women.
If bitterness and acidity in the mouth are accompanied by other symptoms (burning, heartburn, abdominal pain, nausea), you should immediately consult a doctor. Such symptoms can be a sign of many diseases.