Content:
- Causes of pathology
- Signs of inflammation of the submandibular lymph nodes 1.1. First stage 2.2. Second stage 2.3. Third stage
- How to cure an enlarged lymph node in the submandibular area
- Prevention of the inflammatory process
Inflammation of the submandibular lymph node is one of the most common types of lymphadenitis.
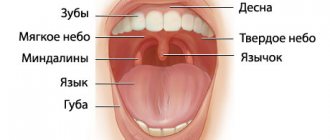
Its development is caused by inflammatory processes occurring in the oral cavity and less often in other parts of the body. Often the problem occurs with advanced caries, pulpitis, gingivitis, and inflammatory lesions of the tonsils. It is also caused by throat diseases. Let's take a closer look at why the submandibular lymph nodes are enlarged and what should be done to normalize the situation.
Complications and consequences
Lymphadenitis behind the ears is a dangerous disease for both children and adults. Most often, if you consult a doctor in a timely manner, the disease begins to recede immediately after the start of therapy for the provocateur of the disease and goes away after it is completely cured.
If you do not contact a specialist in time, the inflammation will progress, spreading to adjacent tissues. During the inflammatory process at the site of infection, lymphoid tissue dies and is replaced by connective epithelium. As a result of this process, the lymph node irretrievably loses its functional abilities: in the future, the problem node will no longer be able to perform the filtering function, which, with subsequent infection of a person, will provoke the direct entry of viruses into the body through its unprotected area.
Even more dangerous not only for health, but also for life is purulent lymphadenitis. The purulent formation, after maturation, opens on its own inward or outward. The second option in this situation is the most favorable, although it is accompanied by the danger of the onset of a septic process.
When an abscess ruptures into the internal muscle tissue, it is almost impossible to predict where the pus will come out. Near the parotid lymph nodes there are vascular connections that can transport pus specifically to the brain, which is almost 100% fatal.
The transition of lymphadenitis into a chronic form also carries hidden dangers for human life: impaired circulation of lymph in the body, expansion of the connective epithelium near the affected area, systematic swelling will become regular companions of the sick person.
Causes of pathology
If the lymph node changes its size, it can be assumed that a viral or bacteriological infection has spread. Taking into account the localization of the lesion, the doctor understands exactly where the source of the disease is located and which organs need urgent medical attention.
Among the dental provocateurs of enlarged submandibular lymph nodes:
- inflammation of the salivary glands;
- gingivitis;
- pulpitis;
- flux;
- stomatitis;
- alveolitis;
- periodontitis;
- deep caries;
- inflammation occurring under the crowns.
But the violation is not always associated specifically with dental diagnoses. Its reasons are:
- Respiratory diseases: pharyngitis, laryngitis, rhinitis.
- Pathologies related to the bone structures of the skull: damage to the bone structures of the lower jaw, damage to the temporomandibular joint, articular capsule.
- Infections: sore throat, measles, tonsillitis, otitis media, chicken pox, mumps. In all these cases, the lymphatic tissues swell a few days after the first symptoms of the disease appear.
- Specific pathologies caused by pathogenic pathogenic agents: toxoplasmosis, tuberculosis, syphilis, gonorrhea.
- Oncological neoplasms. Lymphatic tissue always reacts very sharply to tumor growth. Enlarged submandibular lymph nodes sometimes indicate the presence of a neoplasm in the area of the tongue, neck, or salivary glands.
- Autoimmune disorders. Always associated with disruptions in the functioning of the immune system. Then, by mistake, lymphocytes begin to treat healthy cells as dangerous pathogens. They destroy them, causing inflammation of the lymph nodes.
- Hyperthyroidism. With an exacerbation of this disease, the neck and cheek area swells, the lymph nodes become more voluminous.
In young children, parents may notice large round “balls” under the jaw during the period of active teething. This often causes an increase in body temperature. There is no need to be afraid of such symptoms. It is associated precisely with the inflammatory process provoked by the eruption of milk units. But, if the situation does not return to normal within three to five days, it is still worth showing the baby to a pediatric dentist, surgeon or pediatrician.
Methodology for the treatment of lymphadenitis of the parotid lymph nodes
The methodology for treating lymphadenitis of the parotid region varies depending on the form of the progressive disease and its stage. In the situation with parotid lymphadenitis, medicine provides an integrated approach to therapy, aimed at parallel elimination of negative symptoms, using local treatment of the lesion, taking antibacterial drugs, and targeted treatment of the original source of the pathology. If the disease is purulent, surgical intervention may be required.
Let us consider in more detail each of the areas of treatment of the disease, the rationality of its use in each specific case.
Antibacterial therapy vector
Antibiotics for lymphadenitis behind the ear are one of the central vectors for treating the disease, used for any form of pathology. In each specific case, the specialist selects the most effective antibacterial medication that will affect the source of the disease.
If the disease is provoked by infectious diseases of the standard category, the patient is predominantly prescribed antibiotics with extensive effects on the body. In mild forms of the disease, preference is given to tablet drugs, such as Amoxiclav, Ciprofloxacin, Biseptol and others. In difficult cases, inpatient treatment of the disease may be prescribed with the administration of antibiotics by injection. At the same time, the doctor controls the situation, regularly examining the patient and determining the effectiveness of therapy; if necessary, the antibacterial agent can be replaced.
Amoxiclav
If the patient has a specific type of pathology, then he is prescribed antibiotics of the appropriate category. In this case, it is important that antibiotic therapy does not cause more significant harm to the body and is in harmony with the treatment carried out for the underlying disease.
Painkillers
An equally important task for the doctor in the treatment of parotid lymphadenitis is to relieve intense pain that bothers the patient. During the period of exacerbation, pain symptoms are piercing in nature, which aggravates the general health of the patient and affects the effectiveness of the main therapy.
To eliminate pain, medications such as Ibuprofen or Paracetamol can be used, which, in addition to the analgesic effect, help stabilize body temperature and are characterized by a slight anti-inflammatory effect.
If the pain syndrome is not severe, the use of drugs in this category is contraindicated. In addition, the uncontrolled use of painkillers is strictly prohibited; they can only be used as prescribed by a doctor and in appropriate dosages, so as not to disrupt the dynamics of the effectiveness of therapy.
Antiallergic drugs
The antiallergic direction of treatment in the complex therapy of the disease is used in situations where the primary source of the pathology is allergen-type provocateurs. It is also permissible to prescribe drugs of the antiallergic class when a patient is taking antibiotics, which have allergic reactions as contraindications.
The appropriateness of using antiallergic therapy is assessed by the attending physician, with preference given to third-generation medications, which are characterized by a minimal number of adverse reactions and the absence of a hypnotic effect on the body.
Local therapy
Local treatment of the inflamed segment is an effective method of influencing the symptoms of the disease. Special medical products for external use, such as Sinalar or Dimexide, help reduce swelling and tissue regeneration inside the lesion.
Dimexide
If there are purulent formations in the area of the hearing aid, compresses with Ichthyol ointment or Vishnevsky ointment can be prescribed, which contribute to the effective release of purulent accumulations to the outside. It is rational to use these drugs only in cases where the inflammation is extensive.
Ear lymphadenitis is strictly forbidden to be treated with hot compresses or heating - this can contribute to the appearance of suppuration in the node with all the ensuing consequences. Applying cold compresses to “reduce swelling” is also strictly contraindicated, as it can cause even greater inflammation of already problematic lymph nodes.
Surgery
The radical, last resort treatment for lymphadenopathy is surgery. Doctors resort to such an extreme method of treatment only in cases where other methods of treating postauricular lymphadenitis are not effective, or the cause of inflammation is oncological in nature.
Signs of inflammation of the submandibular lymph nodes
How the disorder manifests itself depends on how far the disease process has progressed. If you do not carry out the necessary therapeutic measures, one stage will quickly pass into another.
First stage
The size of the lymph nodes changes very slightly, but the person already feels that they hurt when pressed. Discomfort occurs when turning the head. Body temperature often rises and a sore throat appears. A tickle or dry, unproductive cough is annoying. Pain occurs only on one side of the neck or on both sides at once. The first case is more likely if it is a viral disease.
Second stage
It is called “acute lymphadenitis”. Now the lymph node can be distinguished visually - it becomes convex and protrudes forward. Externally it resembles a subcutaneous ball. Its diameter reaches three centimeters, but can be more impressive.
The node is painful to the touch. Because of this, it is difficult for the patient to turn and tilt his head, and open his mouth wide. The mobility of the upper and lower jaw is significantly limited.
The pain may radiate to the cheek or ear. Body temperature increases. Overall performance decreases.
Third stage
Called purulent lymphadenitis. Here, the inflammatory process even affects structures adjacent to the lymph node. The patient complains of pain in the throat, collarbone, armpit, and head. The nerve endings of the teeth may become inflamed. Then acute toothache occurs.
Pus formed in lymphoid tissues consists mainly of necrotic cells. If it gets into the blood (and such a possibility always exists), the outcome can be extremely unfavorable, so the inflammatory process should not be started.
Patients can understand that the submandibular lymph node is inflamed and needs treatment as soon as possible by the following signs:
- the “ball” enlarges and becomes red or bluish;
- every day it becomes more dense and solid;
- the skin located above the lymph node takes on a red tint and is hot to the touch;
- the lower jaw area swells.
Symptomatic manifestation of parotid lymphadenitis
The symptoms of the disease vary depending on the form of progression of lymphadenitis in the patient. With a non-purulent type of lymphadenitis behind the ear, patients mainly complain of the following symptoms:
- painful sensations when palpating the inflamed segment;
- slight deterioration in general health indicators, which include body aches, increased fatigue and malaise;
- limited increase in size of one or more lymph nodes, their compaction.
How to cure an enlarged lymph node in the submandibular area
Therapy must be carried out under medical supervision. Its main goal is to eliminate the infection that caused the disorder. If the root cause of the condition is not established, it will not be possible to be completely cured.
If the problem is related to an oral disease, mandatory treatment is carried out. For severe inflammatory pathologies of internal organs, antibiotic therapy is carried out. For pathologies of a viral nature, patients are prescribed antiviral drugs.
If the examination reveals that pus has accumulated inside the tissues, it is drained using a drainage tube. Additionally, a puncture is taken to recognize the pathogen and understand whether the disease has a benign or malignant course.
As soon as the infectious focus disappears, the lymph nodes begin to shrink, stop hurting and gradually reach their normal state.
Features of the treatment of illness in children
The progression of parotid lymphadenitis in school-age children and adolescents is a fairly common occurrence. The causes of the pathology can be infectious and viral provocateurs, as well as the characteristics of the child’s body in the process of its physiological formation.
If symptoms of lymphadenitis appear behind the ear in a child, you should immediately contact your pediatrician to prescribe appropriate treatment. The fact is that children suffer more painfully from any form of lymphadenitis behind the ear; the disease is accompanied by the appearance of fever, severe malaise, and lack of appetite.
The methodology for treating lymphadenitis in children is practically no different from the treatment of adults. A feature of the treatment of pathology in pediatric patients is the selection of drugs according to age indicators, as well as their dosage.
Even if the problem lies in age-related changes, and not in the patient’s infection, the child should receive medical care. As the pathology progresses due to age, the patient may not be prescribed aggressive antibacterial drugs. In this case, methods of health therapy, including taking drugs to enhance immunity, vitamin complexes, and physiotherapeutic procedures, may be sufficient; however, the treatment methodology in each individual case should be selected only by a doctor, taking into account the course of the disease, associated factors and the prevailing symptoms.
Prevention of the inflammatory process
To reduce the risk of developing lymphadenitis, you must strictly follow the recommendations:
- Have annual preventive examinations at the dental clinic. Treat all emerging oral diseases in a timely manner. Avoid caries and take care of your gums.
- Do not ignore the presence of infections and treat them. During therapy, strictly follow all medical prescriptions.
- For any damage to the skin, treat wounds with antiseptics. This minimizes the risk of contracting an infectious disease.
- If you feel unwell, consult a doctor and get laboratory tests. This simple measure allows you to detect violations at the earliest stages.
It is necessary to understand that using “grandmother’s” methods for inflamed lymph nodes is dangerous. So, under no circumstances should you heat the inflamed area or apply cold compresses to it. It is unacceptable to massage him or put pressure on him. All of these actions can make the situation worse. Then it will be much more difficult to reverse the disease.
Diagnosis of the disease
Diagnostic procedures involve identifying the primary source of the disease. The first instance that a person with inflamed nodes in the parotid area needs to visit is a family doctor or therapist; for children, a pediatrician.
The doctor conducts a preliminary examination of the patient with palpation of the inflamed area. Based on the examination and complaints of the patient, a preliminary diagnosis of “parotid lymphadenitis” can be made. Next, the patient will have to undergo a series of specialists to determine the source of infection, as well as undergo standard laboratory tests. Additionally, the patient may be prescribed an ultrasound examination of the inflamed segment.
Further diagnostic procedures depend on individual indicators specific to the patient. If the source of lymphatic inflammation is “on the surface,” then steps are taken to treat it. Otherwise, the search involves additional tests and a comprehensive examination of the body.
The international classification of diseases ICD-10 classifies lymphadenitis in the section “Infections of the skin and subcutaneous tissue.” Inflammation of the parotid lymph nodes in medical documentation is identified by code L 04.0, indicating the localization of infected lymph nodes on the neck, face or head.