Foamy, viscous and stringy saliva in the mouth - causes and treatment
Consistency is one of the characteristics of salivary fluid in the mouth, which few people think about for no reason. Most often, a person learns that it can change when the metabolism in his body is disrupted. However, saliva in the mouth can become viscous and sticky for a variety of reasons, and the treatment of the defect directly depends on what exactly was the prerequisite for its development.
Saliva is normal
The salivary glands of a healthy adult produce from one to two liters of secretion every day. The purpose of this liquid is to lubricate the oral cavity to facilitate chewing and speaking. Thanks to the secretion, the digestion of food begins at the moment of chewing it, since saliva contains active enzymes. The perception of the taste of foods also depends on the degree of their processing by salivary fluid.
Saliva is the first most accessible natural antiseptic. This is why small wounds in the mouth heal much faster than on the skin.
In order for all these processes to proceed exactly as needed, salivation must be sufficient, and the discharge itself must be transparent or slightly cloudy, liquid and imperceptible to humans. A violation of the usual consistency of saliva cannot be ignored, as an obsessive feeling of discomfort is created, speech and the usual rhythm of life are disrupted, and problems with digestion, teeth and oral mucous membranes are possible.
White saliva
Thrush in the mouth
The cause of the appearance of thick white saliva should be sought in fungal infections of the oral cavity and nasopharynx. Most often, this pathology is observed with candidiasis, known as stomatitis or thrush. It usually develops in children, but sometimes appears in adults.
The salivary fluid is colored white by deposits in the form of a cheesy coating characteristic of this infection, which cover the mucous membranes of the mouth. To get rid of the disease, local and internal antifungal drugs are used to strengthen the immune system.
What should you be wary of?
Typically, patients' complaints are related to the fact that in the morning their saliva is not as usual: thick, sticky or foamy. In such cases, accompanying symptoms may occur:
- violation of taste perception;
- constant dry mouth and throat;
- feeling of persistent thirst;
- tingling sensation on the tongue;
- difficulty and pain when chewing and swallowing food;
- sore throat and hoarseness;
- cracks on the lips;
- rapid formation of plaque on teeth;
- inflammatory processes in the oral cavity and gums.
All these phenomena may be a consequence of changes in the composition, quantity and viscosity of saliva. A simple test that you can take yourself in the morning on an empty stomach will help you verify the validity of such suspicions or dispel them. To do this, you need to get a pipette with marked divisions and a stopwatch.
First, you need to put a milliliter of ordinary water into a pipette and observe how long it takes for it to flow out. Then you need to do the same with the salivary fluid. It remains to compare the two indicators - normally, they should be approximately the same.
But self-examination is a subjective thing, therefore, if there is any suspicion of a serious malfunction in the body, you should contact specialists to conduct accurate laboratory tests. Doctors determine whether the consistency of saliva is normal using a viscometer. If he confirms that the patient really has too thick saliva in his mouth, the doctor will determine the cause of the defect and prescribe the necessary treatment. Diagnosis will require additional tests and consultations with specialists, so self-medication in such a situation is unacceptable.
Diseases that cause dry mouth
In some pathologies, severe dry mouth can be a symptom, in others it accompanies the course of the disease.
Inflammatory diseases of the oral cavity
With inflammation of the gums or dental diseases, the amount of saliva may decrease due to greater fluid consumption for chewing food. The same situation occurs with a bad prosthesis. The salivary glands simply do not have time to replenish their reserves.
Diabetes
Excess weight is accompanied by metabolic disorders. If you are always thirsty and your throat is “dry”, and trips to the refrigerator are becoming more and more frequent, you should check your blood sugar level and make an appointment with an endocrinologist.
“Dry mouth and thirst are the first signs of diabetes.”
Especially if the above symptoms are accompanied by repeated visits to the toilet at night.
Infections
Infectious diseases are often accompanied by vomiting and diarrhea accompanied by fever. Losing a large amount of fluid causes dry mouth, which, usually, in this condition, few people pay attention to. However, this cannot be ignored. With severe intoxication, fluid loss is an additional risk factor, so the patient needs to drink a lot. Water removes toxins from the body and replenishes fluid deficiency.
Endocrine diseases
Some endocrine diseases may be accompanied by a decrease in the amount of saliva produced, for example, thyroid dysfunction. In women, dry mouth may be associated with pregnancy or menopause.
Xerostomia in autoimmune diseases
With autoimmune diseases, a person’s defenses fail and they attack their own body. This damages the entire system. The second name for these diseases is systemic.
As a striking example, consider Sjögren's syndrome. The disease affects the salivary glands, causing dry mouth and difficulty swallowing. The oral mucosa becomes bright pink.
Xerostomia in diseases of the brain and nervous system
During a stroke, partial death of brain cells occurs; it is difficult to predict which functions will be affected. Dryness of the oral mucosa can also occur with Alzheimer's or Parkinson's disease, pathologies of the trigeminal nerve and circulatory system.
Gastrointestinal tract and dry mouth: what diseases require an appointment with a gastroenterologist
Particularly noteworthy are diseases of the gastrointestinal tract. Xerostomia is not one of the symptoms of these diseases, but may accompany them:
- A stomach ulcer, as a result of smoking or drinking alcohol, is necessarily accompanied by dry mouth.
- Gastritis, acquired through dietary abuse or as a result of stress, also does not exist without this symptom.
- Acute pancreatitis is accompanied by vomiting and diarrhea, resulting in dehydration and its symptom – xerostomia.
Gastrointestinal diseases should not be joked about, so you need to visit a gastroenterologist and start treatment.
Acute pathologies requiring hospitalization
Acute pathologies, in addition to severe pain, also cause dry mouth. Appendicitis and intestinal obstruction, as well as perforation of the ulcer, require urgent surgical intervention.
Why is saliva viscous and stringy?
A symptom such as thick drool often causes dehydration due to insufficient fluid intake and intoxication , accompanied by vomiting and diarrhea. In addition, the cause of thick saliva may lie in the side effects of medications. Diuretics and choleretic drugs, antihistamines and antidepressants, as well as a number of painkillers, radiation and chemotherapy can cause malfunction of the salivary glands. In these cases, stopping or replacing the drug is enough to solve the problem.
Experienced smokers often experience dry mouth mucous membranes, which is accompanied by the appearance of viscous, sticky saliva. For some, such a violation accompanies them until they completely give up the bad habit.
The cause of viscous or foamy saliva may be a natural hormonal imbalance that occurs during pregnancy, menopause, or adolescence in adolescents. No drug therapy is required in these cases.
When the root of the problem lies in internal diseases, it can be very difficult to determine the true cause. Some diseases directly complicate the work of the salivary glands : with mumps, Mikulicz's disease and sialostasis, the glands enlarge and become painful, secretion production is significantly reduced, and salivary stone disease and neoplasms can even lead to their surgical removal. In any of these cases, the saliva may take on an unusual consistency. Cystic fibrosis, scleroderma, Sjogren's syndrome, HIV, retinol deficiency, and anemia can also manifest themselves in a similar way.
The reason for the appearance of unusually thick and viscous saliva in the mouth can also be an injury that causes rupture of the ducts or gland tissue. In this case, you will need the help of a surgeon. Various internal diseases can affect the functioning of the salivary glands and the properties of their secretions:
- neurological;
- hormonal;
- gastrointestinal;
- autoimmune;
- rheumatoid;
- psychosomatic.
Dryness and stickiness in the mouth, accompanied by a decrease or complete absence of saliva and resulting from deep internal pathologies, is called xerostomia. Associated symptoms of the disease are redness of the tongue, cracks and jams on the lips, soreness in the mouth and throat. Xerostomia develops progressively, depending on the cause, the pathology can be temporary or permanent - both require timely treatment under the supervision of a doctor.
Sticky mucus can look and feel different. Thick sputum is white, foamy, thick, viscous, and can create a feeling of a “lump in the throat.”
Causes of impaired functioning of the salivary glands
Problems with the glandular system are marked by symptoms: in the morning thick, foamy saliva appears, similar to mucus, lips, and the corners of the mouth become covered with cracks or ulcers. With impaired salivation, dry mucous membranes are constantly observed. Among the diseases and pathologies affecting the salivary glands are:
- Diseases of the salivary system
. The production of saliva sharply decreases, the areas under the jaw, closer to the ears, become inflamed. Pathology occurs with mumps, Mikulicz's disease, and sialostasis. - Removed glands
. Amputation occurs along with the excision of cysts, benign tumors, as a result of clearing salivary stones. - Cystic fibrosis
. Genetic cause of deterioration of secretory functions.
Causes of sticky saliva in the throat
Saliva can not only foam, but also seem to get stuck in the throat. In this case, it is necessary to examine an ENT doctor for damage to the tonsils and larynx. Purulent forms of tonsillitis or tonsillitis are accompanied by the appearance of plaques on the tonsils, which create discomfort and pain, and when opened, they release purulent contents into the pharynx, increasing the saturation of sputum.
Gum disease accompanied by the discharge of pus may also be an explanation for why saliva has become thick, viscous and felt in the throat. Such diseases include periodontitis, periodontal disease, cysts, cellulitis and abscesses. Sticky pus from the affected areas of the gums mixes with saliva and makes swallowing difficult.
How to relieve the condition when saliva is viscous and stringy
A person whose saliva thickens and foams experiences a lot of unpleasant sensations. In addition to discomfort, outbreaks of diseases of the throat, tongue, and gums may become more frequent, and teeth become more vulnerable to caries. Therefore, this symptom must be eliminated using conservative and traditional methods of treatment.
Having determined why the saliva in the patient’s mouth has become thick and viscous, the doctor will prescribe treatment for the underlying disease that caused xerostomia, as well as auxiliary local methods that will help quickly return to normal life:
- artificial saliva;
- various oral moisturizers in an easy-to-use form (gel or spray);
- specialized rinses;
- special chewing gum and lollipops;
- drinking plenty of fluids.
Folk remedies for the treatment of xerostomia include sage or fenugreek tea, lubrication of the oral cavity with a mixture of peach oil and propolis, and inhalations with eucalyptus. But it is better to discuss these treatment methods with your doctor.
It would not be superfluous to purchase an air humidifier for the room and give up tobacco, alcohol, soda and coffee, which additionally dehydrate the mucous membranes. The consumption of dairy products will also have to be minimized. The daily volume of clean water consumption should be at least one and a half liters. During this period, it is better to choose a toothbrush with soft bristles so as not to injure dehydrated gum tissue.
Don't wait until unusual sensations in your mouth develop into unbearable ones. The viscosity of saliva is one of the serious indicators of the health of the body. If it deviates from the norm, action must be taken.
Thick saliva
The salivary glands produce a multicomponent fluid (secret), which mainly consists of water. Only 5% of saliva is enzyme compounds, amino acids, acidic salt residues and various trace elements. This secret performs a lot of important functions in the human body:
- protective (moisturizes the oral mucosa, protects it from attacks by pathogenic bacteria);
- digestive (ensures the formation of a food bolus);
- allows you to taste the food.
In a healthy person, saliva is a transparent, odorless liquid, which upon contact with the mucous membrane does not cause irritation, burning or other discomfort.
Why is there a problem?
Thick saliva is a symptom that many patients may experience. The viscous, foamy liquid is the result of a failure in the production of mucin glycoprotein (high molecular weight components responsible for the formation of the food bolus). Other causes of thick saliva are disorders of the autonomic nervous system, eating foods with strong odors and strong tastes (increase salivation).
Pathological factors causing the appearance of white mucus in the mouth:
- Sinusitis. These are active inflammatory processes in the nasal sinuses, which “make themselves known” with thick and viscous sputum and bad breath. Snot from the nose enters the oral cavity, from there into the pharynx, flows down the back wall of the throat, and ends up in the stomach. The chronic course of sinusitis, in addition to local symptoms, can be complicated by regular severe headaches, fever, and weakness.
- Xerostomia. In this case, viscous saliva and mucus in the mouth are a consequence of disruption of the salivary glands themselves. Additional symptoms: swelling, hardness of the tongue, dryness, irritation, burning sensation on the mucous membrane. The throat may be sore, sore, and the functioning of the taste buds may be impaired.
- Fungal candidiasis. A disease of an infectious nature that develops against the background of an immune failure in the body. Thus, saliva becomes sticky in patients who take medications on a long-term basis - corticosteroids (hormones) or antibiotics. In addition, the candida fungus enters the oral cavity through contact (through a kiss, when sharing personal hygiene items). Associated discomfort: dysphagia, metallic taste in the mouth, burning and itching of the mucous membranes.
Common respiratory diseases such as tonsillitis, laryngitis, and pharyngitis also lead to the appearance of foamy saliva. The infection affects the tonsils, causing the formation of purulent blisters on the back wall of the throat - when they resolve themselves, purulent exudate flows into the oral cavity, causing the appearance of a putrid odor (taste), the feeling of thick mucus in the mouth. In addition, the course of such diseases is accompanied by an increase in body temperature, dehydration, and dysfunction of the salivary glands - the amount of secretion produced decreases, and saliva in the mouth thickens.
Dental problems can also be the “culprit” for the appearance of thick, viscous saliva. Periodontitis, periodontal disease (inflammatory lesions of the soft tissues of the oral cavity) lead to pathological changes in the structure of the gums, the amount of saliva produced decreases. In addition, elements of epithelial tissue mix with the secretion, making it viscous and thick.
Malfunctions of the gastrointestinal tract provoke the appearance of thick saliva in the throat. Gastroesophageal reflux disease causes stomach acid to rise up the esophagus and reach the mouth. Thus, the salivary glands are forced to produce more secretion to neutralize the effect of gastric juice on the mucous membrane - the consistency of saliva changes.
Thesiography - diagnostics of saliva. Saliva and its effect on oral health
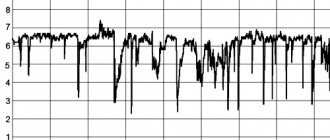
What is the pH of saliva?
This is a pH value that helps determine the acidity of oral fluid.
Determination of the pH of saliva is carried out with special test paper strips soaked in acid and an acid-base indicator. A drop of saliva from a pipette is applied to such a strip; the saliva, to one degree or another, neutralizes the acidic impregnation of the strip, as evidenced by a change in the color of the indicator. Most often, the initial acidic pH level = 4.5 corresponds to a yellow-brown color, slightly acidic pH = 4.5-5.5 - green color, neutral pH - blue color. The closer the strip gets to the neutral state under the influence of buffer forces, the better.
The role of Ph in the development of caries
The reflux of acidic stomach contents through the esophagus into the oral cavity helps reduce the pH of saliva and plays an active role in the development of “local” pathological processes. After the hydrochloric acid has reached its destination, the Ph of the mixed saliva decreases to 7.
The secretion, which normally has alkaline properties, with an acidity level of 6–6.2 causes the destruction of tooth enamel, its demineralization, which subsequently results in the appearance of carious lesions. The gums become inflamed, swollen, red, and the amount of mucus on the mucous membrane increases noticeably. Oxygen-rich saliva prevents the proliferation of pathogenic microflora; with reduced acidity, these microorganisms “bloom.” Hunger, excitement, stress, pronouncing a long monologue, breathing through the mouth - these are all the factors that lead to a decrease in Ph. The same phenomenon is associated with natural age-related changes in the body.
The pH of mixed saliva allows us to judge the degree of demineralization of free dental tissues. This biological fluid constantly maintains a neutral acid-base reaction (average value - 7.2) of the oral environment due to the proteins and phosphates it contains.
According to the results of modern research, it is the prolonged exposure of acids to the hard tissues of teeth that provokes the appearance of carious lesions. When acidity decreases, saliva retains and binds calcium atoms, which leads to demineralization of teeth. Biological fluid prevents the dissolution of enamel and ensures the diffusion of calcium and phosphorus ions.
Saliva and its effect on oral health
It should be noted that the development of caries is associated not only with teeth and the activity of bacteria. The oral cavity represents
is a complex of organs and tissues in a moist environment (saliva). Saliva is a complex secretion. Oral fluid is commonly referred to as "mixed saliva." It primarily consists of the secretions of the major and minor salivary glands. In addition, it contains a number of components of non-salivary origin. These include: fluid of the gingival groove, serum components and blood cells, bacteria and their metabolic products, desquamated epithelium and cellular components, viruses and fungi, food debris and sputum secreted from the bronchi. Saliva is 99% water. The remaining 1% consists of large molecules of organic compounds such as proteins, glycoproteins and lipids, as well as small molecules of organic substances such as glucose and urea, electrolytes, mainly sodium, calcium, chloride and phosphates.
Mixed saliva is complete saliva without impurities that can be removed by centrifugation, or a mixture of pure saliva from all sources. Pure saliva is a liquid produced and secreted into the oral cavity by three pairs of large and many small glands. Every day, from 300 to 1500 ml of saliva is secreted into the human oral cavity. The production of saliva during the day is uneven: within 14 hours, without eating, approximately 300 ml of the so-called basic, unstimulated saliva is produced (salivation rate - 0.25-0.50 ml/min), within 2 hours, 200 ml is released against the background of food stimulated saliva (at a rate of 2.0 ml/min), and in the remaining time - 8 hours of night sleep - salivation practically stops (0.1 ml/min). At any given time, there is about 0.5 ml of saliva in the oral cavity. The prevalence and intensity of caries depend on the rate of salivation; these indicators are higher in children with a sharp decrease in salivation.
Saliva is well known to have protective properties against dental caries. The most direct evidence of this fact is the development of “blooming” caries following the cessation of the functioning of the salivary glands due to irradiation with high doses, due to tumors of the head and neck. Such caries is so destructive that within a few weeks it affects usually caries-resistant surfaces and causes complete destruction of the crowns of the teeth.
The main properties of saliva that provide protection against caries are the following:
- dilution and clearance of food sugars; • neutralization and buffering of acids in dental plaque; • providing ions for the remineralization process.
- lysozyme - can destroy the cell wall and dissolve bacteria; • lactoferrin - connects iron atoms to bacterial cells, which gives a bacteriostatic effect; • lactoperoxidase group - thiocyanin - H2 + O2 - the formation of oxygen springs gives a bactericidal effect, these sources accompany the reaction of many unsaturated fatty acids in the cell wall of the bacterium.
Saliva has a significant effect on the pH level of dental plaque, including preparing the food bolus for swallowing, as a result of which mechanical and chemical cleaning of the oral cavity occurs, and food debris that adheres to the smooth surface of the tooth is eliminated.
At the same time, they are partially purified enzymatically. Both of these processes are essential for the prevention of caries. Saliva protects the mucous membrane from damage, and also protects teeth from pathological abrasion by antagonist teeth. The enamel-saliva system can easily withstand a short-term “attack” of acid on the teeth.
Fluorine, phosphates and calcium found in saliva are the initiators of remineralization. The buffer system can neutralize acids to some level. In the moist environment of the oral cavity, acidic bacterial products cause constant pH fluctuations, which are neutralized by the buffer system. The buffer system is a protective element of saliva. Direct release of substances that inactivate bacteria:
The concentration of calcium and phosphates in saliva is very significant for the integrity of teeth.
Saliva is saturated with a solution of these ions. Inhibitory substances, similar to some bodies containing phosphates, block the spontaneous precipitation of the salt mixture on the surface of the enamel, which weakens the connection of microorganisms with the tooth surface. On the other hand, the solubility of mineral substances decreases. The reason for the restoration of superficial carious defects is not a single deposition of ions from saliva, but rather the recipitation of dissolved mineral substances removed from the deeper layers of the carious defect. The frequency of fluoride use plays an important role. Mineralizing potential of saliva
The mineralizing potential of oral fluid can be judged by the type of crystal-like formations in a drop of saliva placed on a glass slide. By the type of microcrystallization of saliva, one can judge the patient’s susceptibility to caries. Microcrystallization of saliva has individual characteristics and this may be associated with the general condition of the body, oral cavity, and nutrient load. The formation of microcrystals can characterize the remineralizing ability of saliva, and the intensity of caries is associated with the type of microcrystallization. In caries-resistant individuals, tree-shaped crystal-like formations are observed with a tendency for a drop of saliva to be located in the center.
In those susceptible to caries, this structure changes or disappears completely. It is believed that there is a close relationship between the structural and mineralizing properties of saliva.
There are three types:
Type I - a clear pattern of elongated crystalloprismatic structures fused together and occupying the entire surface of the drop. This type is inherent in the compensated form of caries.
Type II - in the center of the drop, individual dendritic crystalloprismatic structures of smaller sizes are visible than in type I. Characteristic of the subcompensated form of caries.
Type III - a large number of isometrically located crystalline structures of irregular shape are visible throughout the drop. This type of microcrystallization is characteristic of the decompensated form of caries.
At the same time, microcrystallization of saliva reflects the state of the body as a whole, so this parameter can be used for rapid diagnosis of some somatic diseases.
Conclusion
In the structure of dental morbidity, dental caries occupies one of the leading places, which in the absence of timely and correct diagnosis, which in addition to the main examination methods, additional ones should be used (such as test-measurement of saliva pH and thesiography). It is impossible to prescribe adequate treatment, which in turn will lead to the threat of the development of various odontogenic complications, the appearance of foci of chronic infection, functional disorders of the dental system, which have a negative impact on the patient’s health as a whole. Therefore, all efforts of specialists should be aimed at preventing dental caries using the latest technologies and materials available on the global dental market.
In our Jasmine family clinic, you can conduct a saliva pH test and tesiography (determining the mineralizing potential of saliva), where the doctor will tell you in detail about the health of your oral cavity and select an individual course of prevention.
Diagnosis and treatment
It is quite possible that the increased thickness of saliva in the morning is the result of hormonal changes in the body, so the problem may resolve on its own after some time, the salivary glands will restore their normal functioning. If such an abnormal phenomenon persists for a long time, it is necessary to visit a dentist, assess the condition of the teeth and oral mucosa, and exclude local inflammatory processes. The doctor will give directions for studies to assess the “health” of the salivary glands.
Important! The first thing that needs to be done in case of increased viscosity of saliva is to cope with dry mouth and “wash out” pathogens that begin to attack the mucous membrane when local immunity is reduced. To do this, experts recommend rinsing your mouth with decoctions of herbs with anti-inflammatory properties (chamomile, calendula) and a soda-salt solution (½ teaspoon of each powder per glass of warm boiled water).
For laryngitis, pharyngitis and other respiratory diseases, it is advisable to use gels, sprays, and solutions with antiseptic properties. The dentist may prescribe artificial saliva or a spray humidifier for the oral cavity. Such products also have antibacterial properties and fight bad breath.
Bromlane, Acetylstein are mucolytic drugs that thin saliva well and help remove mucus in infectious respiratory diseases. Inhalation is another method of dealing with the problem. Pharmaceutical compositions or decoctions, infusions of medicinal plants well moisturize the mucous membrane, provide an anti-inflammatory effect, and make the consistency of saliva more liquid.
Prevention
To avoid problems such as increased viscosity of saliva, it is recommended to drink at least 2 liters of liquid per day, with preference given to purified water. It is better to limit the intake of carbonated, caffeinated drinks (they dehydrate the body). Quitting alcoholic beverages and smoking also has a beneficial effect on the functioning of the salivary glands.
It is useful to rinse your mouth with a warm saline solution from time to time, avoid hypothermia and stress, do not buy sugar-containing chewing gum, and humidify the air in the room. A well-structured, balanced diet with plenty of fiber (vegetables, fruits) and cereals is the best prevention of any problems with the digestive organs, including the salivary glands.
So, foamy, sticky and viscous saliva is a signal notifying about certain problems in the body. The cause of the anomaly may lie in a malfunction of the salivary glands themselves, hormonal or metabolic disorders, bad habits or chronic diseases (“the respiratory organs, gastrointestinal tract, and oral cavity suffer”). A dentist will help determine the cause of the problem and select the appropriate treatment, who, if necessary, will involve other specialists (immunologist, neurologist, gastroenterologist, etc.).
Causes not related to diseases
Sticky saliva in the mouth, dryness and discomfort occur as a result of other factors. You can simply avoid or eliminate them at home (or wait a while for the body to recover on its own). Here are the most common reasons:
- dehydration
- often appears after physical activity, in the hot season, after too much sleep; - dry air
- due to excessive operation of the heating system, dry mucous membranes develop; - radiation therapy
- changes in saliva occur with large doses of radiation or when treating the throat; - alcohol abuse and smoking
- lead to dehydration, problems with the secretion of all internal glands;
Saliva becomes viscous during certain physiological processes and pathologies.
Changes in saliva during pregnancy
During the first trimester of pregnancy, women may experience changes in their mouth. The process is especially noticeable in the evening before bedtime and at night. Additional symptoms occur: hot flashes, stomach problems, dry nose and mouth, metallic taste, cracked lips.
All unpleasant sensations during pregnancy associated with salivation depend on the functioning of the hormonal and metabolic system.
Sometimes the changes occur due to medications, other times due to increased volume of fluids in the body. Dry mouth and altered salivation are accompanied by frequent urination. An accelerated metabolism leads to sweating and, as a result, dehydration may occur.
Salivation disorders
Salivation (or salivation) is one of the most important processes in the human body, ensuring the normal condition of the mucous membranes of the mouth, gums, teeth, and tongue.
Unfortunately, the process of salivation in some cases can proceed incorrectly, which will be discussed in the article.
Types of disorders of normal salivation
Hypersalivation
Saliva is produced in too large quantities and must be constantly spat out or swallowed.
There are very frequent cases of saliva leaking from the mouth during sleep, when the muscles, including the facial ones, completely relax, and the person is simply not able to control himself at such a moment.
However, the condition of the oral mucosa most often does not cause any concern in patients.
Moreover, in the vast majority of cases, hypersalivation goes unnoticed and is considered a completely normal phenomenon.
In children who have not yet turned four years old, teeth cut and grow very quickly, and the gastrointestinal tract develops. Most often, the process of development of the salivary glands in this case simply cannot “keep up” with other development processes in the body.
Hyposalivation
Diseases in which this syndrome occurs
Excessive salivation may indicate:
- Parkinson's disease;
- Some helminthic diseases;
- Increased tone of the vagus nerve;
- Pancreatitis;
- Gastritis;
- Ulcer;
- Cholecystitis;
- Gingivitis, periodontitis;
- Diseases of the thyroid gland.
Insufficient saliva production indicates:
Diagnostics
Which doctors are recommended for a person to see if he notices a problem with salivation?
- Therapist (first of all!);
- Neurologist;
- Dentist;
- Endocrinologist;
- Gastroenterologist;
- Maxillofacial surgeon.
Hyposalivation can be diagnosed as follows : a specialist examines the oral mucosa; if it is very poorly moistened or completely dry, saliva resembles foam or is completely absent, then measures need to be taken.
The doctor will help determine whether hypersalivation is real or false (for example, increased salivation occurs during obsessive states, impaired swallowing functions, and neuroses).
It is worth saying that if hypersalivation is a consequence of inflammatory diseases of the oral cavity, then treatment is not required (except for the treatment of a specific inflammatory disease that has nothing to do with salivation).
If hypersalivation is associated with disorders of the nervous system, then it should be treated equally with the underlying disease. In this case, tranquilizers and antidepressants are used, as well as hypnotherapy.
In case of disturbances in the process of salivation, galvanization of the salivary glands is also used. Electrophoresis using a 1% solution of galantamine hydrobromide is often prescribed.
Main reasons
Malfunctions of the salivary glands are usually attributed to the following reasons:
- mumps, Mikulicz's disease, sialadenitis, sialostasis are diseases of the salivary glands, in which the glands themselves increase in size, become painful, and the amount of saliva secreted decreases;
- mucoviscitosis is a congenital disease that affects the exocrine glands;
- scleroderma - in addition to the secretion of saliva, the connective tissue of the mucous membranes grows;
- with a lack of vitamin A, the volume of epithelial tissue increases, thereby clogging the ducts of the salivary glands;
- damage to nerve endings in the head and neck area;
- injury to the salivary glands;
- HIV infection.