Everyone wants to have a white-toothed smile, but what to do if a person has total edentia (the jaws are completely toothless)? Prosthetics in case of complete absence of teeth is the best way out of the situation. Depending on the condition of the oral cavity and other important factors, there are several types of prosthetics - completely removable and conditionally removable. In the first case, a person will have to take the dentures out of his mouth every day, clean them and put them in a glass of water at night. In the second, several implants are implanted into the gums, on which artificial teeth will be installed.
Types of prosthetics for complete absence of teeth
In dental orthopedics, there are two options for complex prosthetics for total edentia: removable and fixed.
Fixed prosthetics
The Family Dentistry clinic performs daily rehabilitation operations for patients with complete absence of upper or lower teeth. We have performed more than 1,200 total jaw replacements.
All-on-4
A protocol for complex prosthetics, involving the installation of a fixed prosthesis with 10 or 12 crowns supported by four implants:
- two are implanted in parallel in the anterior section;
- two at an angle of up to 45° in the distal.
Why is inclined implantation of two implants used? Firstly, to increase the contact area between the bone and the implant (allows you to abandon the sinus lift). Secondly, in order to eliminate the risk of damage to the mandibular nerve or maxillary sinuses.
All-on-4 technology or “All-on-4” is a predictable and well-studied method of treating complete edentia (used since 1998) without bone grafting with good results in the short, medium and long term.
3-4 hours after installation of the implants or 3-7 days (often you need to wait for the swelling of the mucous membrane to go away after surgery), a temporary prosthesis is attached to the abutments.
After complete engraftment of titanium screws into the bone tissue (on average, this takes from 3 to 6 months), fixation is carried out with a permanent orthopedic structure.
All-on-6
A technique for complete jaw prosthetics for total edentia, developed on the basis of the All-on-4 protocol and being its logical, modified continuation.
To make it possible to use the technology in the rehabilitation of patients with a complex clinical picture (severe bone tissue atrophy, periodontitis/periodontal disease, diabetes mellitus, osteoporosis), six implants are used:
- two are fixed in the frontal zone;
- four – in the distal lateral section (two each on the right and left).
The use of a larger number of implants provides more reliable support for a fixed prosthesis (a bridge structure with a length of 14 crowns can be installed) and uniform distribution of the chewing load throughout the entire arch.
Stages of prosthetics
Creating a comfortable prosthesis with a minimal adaptation period will require several visits to the clinic. To eliminate inaccuracies in manufacturing, several pairs of impressions, fittings and bite testing are necessary.
- Taking impressions Taking preliminary impressions of the jaws to make a plaster model and final impressions to make a prosthesis template with the exact boundaries of the base.
- Bite study Determination and fixation of central occlusion based on facial characteristics using a facebow for transfer to the articulator in order to recreate the bite.
- Creating a template In the laboratory, the artificial teeth are first placed in the articulator on a wax template, taking into account the occlusion and the data obtained during the diagnosis.
- Try-ons The patient can visually evaluate the result and determine the degree of comfort. The doctor determines the relationship of the jaws in the oral cavity and their correspondence to facial features.
- Making a prosthesis When the template of the prosthesis is perfected, in the laboratory the model goes through a technological stage, the wax is replaced with a permanent plastic base through polymerization.
- Check in the articulator The bite is fixed with the finished prosthesis, the closure of the jaws is checked in the articulator in the clinic. If the smallest deviations are detected, adjustments are made.
The finished prosthesis is fixed to the jaw by applying slight pressure. Next comes the most important stage - getting used to or adapting to a removable denture. Sometimes there may be some discomfort in the first 1-2 weeks. It may be necessary to make a few more adjustments - we bring the prosthesis to an ideal state so that the person is extremely comfortable and convenient, so that he stops feeling it .
Prices for complete prosthetics
| Name | Price, rub) |
| Complete jaw prosthetics on 4 Osstem implants (South Korea) with a fixed plastic prosthesis | RUB 225,000 |
| Complete jaw prosthetics on 6 Osstem implants (South Korea) with a fixed plastic prosthesis | 275,000 rub. |
| Promotion! Jaw prosthetics on 4 Straumann (Switzerland) or Nobel (USA/Sweden) implants with a fixed plastic prosthesis | 260,000 rub. |
| Promotion! Jaw prosthetics on 6 Straumann (Switzerland) or Nobel (USA/Sweden) implants with a fixed plastic prosthesis | 320,000 rub. |
Removable prosthetics
At the Family Dentistry clinic, treatment of patients with complete absence of teeth in the upper or lower jaw is carried out only by the method of permanent prosthetics on implants. The main disadvantage of removable dentures is atrophy of the jaw bone. The longer you wear them, the more bone tissue decreases. Subsequently, when the patient decides to install a fixed prosthesis, preliminary bone grafting will be required. If you decide to wear a removable denture, we can only help you find a good dental clinic that provides removable denture services.
1 Acrylic prosthesis
2 Acry Free dentures
3 Nylon prosthesis
A classic option for restoring the integrity of the dentition with complete edentia. In demand due to its low price. But at the same time it is the most inconvenient type of complete removable denture. Pros:
- low price;
- fast production times;
- easy to repair, adaptable (increases service life).
Minuses:
- provokes injury and inflammation of the gums due to constant stress;
- takes up a lot of space in the mouth (more voluminous than its counterparts), it is difficult for the patient to get used to wearing a plastic prosthesis;
- may cause an allergic reaction as a result of the free monomer contained in acrylic reacting with saliva;
- the artificial gum is opaque, the acrylic prosthesis does not look natural;
- Acrylic absorbs food coloring pigments and requires careful care.
Acry Free thermoplastic plate prosthesis is the most durable, aesthetic and long-term solution in complete removable prosthetics. Pros:
- The Akri Free prosthesis is thin and fits more tightly to the tissues of the prosthetic bed (the patient gets used to wearing it faster);
- does not cause allergies, as it does not contain methyl methacrylate;
- thanks to the aesthetic artificial gum, it is practically indistinguishable from your own teeth;
- has no pores (unlike acrylic and nylon), does not absorb food pigments, does not cause bad breath, and is less demanding in care;
- easy and inexpensive to repair.
Minuses:
- fragile, does not always withstand increased chewing loads and breaks;
- the price is twice as high as for an acrylic prosthesis.
Made from dental nylon, which is lightweight and elastic. Typically used as a temporary solution. Pros:
- takes up less space in the mouth, weighs less, so it is comfortable to wear;
- the prosthesis is flexible, easy to remove and put on, and will not break if accidentally dropped on the floor;
- The orthopedic design is practically invisible, as it is made of translucent material with a shade close to the color of the gums.
- does not cause allergic reactions like acrylic prosthesis.
Minuses:
- due to flexibility, it does not distribute the chewing load over the entire mucosa and leads to rapid atrophy of the alveolar ridge;
- nylon cannot be polished; after 2 years, plaque and pigments accumulate on it, and its attractiveness is lost;
- Eating hot food/drinks increases the elasticity of the prosthesis; frequent adjustments are required;
- rubs the gum, causing its atrophy (abrasions and bedsores form under the denture);
- repair of a nylon removable denture is very complex and expensive, and relining in the oral cavity is impossible;
- absorbs odors, after 1-2 years it begins to smell unpleasant.
Examples of work “Before” and “After”
Basal implantation of both jaws with complete edentia
Case: the patient complained of missing teeth in the upper jaw, in the area of chewing teeth in the lower jaw, as well as mobility and pain when chewing in the area of the front teeth in the lower jaw.
Basal implantation of ROOTT with complete edentia
Case: destruction and absence of chewing teeth, destruction of frontal teeth under crowns, atrophy of bone tissue and gums due to periodontitis.
Why is fixed prosthetics better than removable prosthetics?
Preventing bone atrophy With complete removable dentures, the main part of the chewing load is transferred to the mucous membranes, so bone tissue resorption begins. Implants function like real tooth roots. The chewing load is distributed onto the artificial teeth as if they were your own. Bone loss stops.
Reliable fixation A removable denture covering the entire jaw can fall out at any time. Fixed prosthetics on implants eliminates the risk of falling out. It eliminates the constant fear that the denture will fall out of the mouth at the most inopportune moment.
Preservation of taste/heat sensitivity A complete denture covers the palate. As a result, the taste and heat receptors of the oral cavity do not work.
Full restoration of chewing function A complete removable denture restores the chewing ability of the dentition by only 20-30%.
Prosthetics on implants
If the patient’s budget and health condition allow for minimally invasive surgery, it is better to opt for implant prosthetics.
There is no need to install 28 units of titanium rods separately. In some cases, patients are offered the installation of 4-6 implants on each row and fixation of solid prostheses on them. Advantages of installing dentures on implants
- Reliability – the prosthesis on the implant is held as firmly as your own living tooth with roots.
- Aesthetics – dentition restored in this way pleases with its natural appearance and beauty.
- Ease of chewing
- Durability – the guarantee for implants is determined by the manufacturer at the level of 10-50 years. It is enough to choose the right prosthesis and forget about problems with missing teeth for several decades.
- Possibility of replacing dentures - if the coronal part is destroyed, you can always install a new denture on the metal root.
The disadvantages of the method include the presence of contraindications and higher cost compared to prosthetics without implants.
Stages
1 Consultation, diagnostics
2 Preparation
3 Surgery
4 Orthopedics
The doctor will visually examine your teeth and gums to make an initial assessment of their health. He will collect anamnesis, conduct a hardware examination (orthopantomogram + computed tomography), and make sure that there are no contraindications to prosthetics on implants.
Plaque and stone are removed, diseased teeth on the antagonist jaw (if there are teeth) are treated. The implant dentist prepares a treatment plan, incl. 3D model of the jaw for detailed planning of the operation. A date for the operation is set and a contract is concluded.
An injection of local anesthesia is administered. Four or six implants are installed depending on the technology used for prosthetics of a toothless jaw.
On days 3-7 after installation of the implants, a temporary (adaptation) prosthesis is fixed on them. At the end of the period of osseointegration of the artificial roots, a permanent prosthesis is placed.
What are the causes of complete tooth loss?
You can lose all your teeth for several reasons:
- advanced caries. Untimely treatment of dental caries invariably leads to their destruction and the gradual removal of all teeth.
- gum disease, in particular periodontitis (meaning the extensive form (generalized), when all gums are affected by periodontitis). With severe periodontitis, the teeth become so loose that they can no longer be saved.
- injury. Teeth can be lost, for example, in a car accident, oral surgery, or other circumstances.
Questions and answers
Are there any contraindications to fixed prosthetics supported by implants?
Absolute contraindications include:
- chronic heart failure, angina pectoris, arterial hypertension;
- diseases of the blood and hematopoietic system;
- oncology (cancer, sarcoma);
- pathologies of the immune system.
Relative contraindications in which surgery is postponed include:
- poor oral health;
- presence of dental diseases (gingivitis, pulpitis, periodontitis);
- malocclusion;
- diseases of the temporomandibular joint, etc.
What material do you use to install a permanent fixed prosthesis?
For total prosthetics of an edentulous upper or lower jaw supported by implants, we install a permanent bridge with crowns made of zirconium dioxide - the most durable and aesthetic material in modern dental orthopedics.
How to care for a fixed overdenture on implants?
- Be sure to purchase a new toothbrush with a soft or ultra soft hardness level. Start brushing her new teeth only after three days from the date of surgery. It is better to use a herbal paste to prevent gum inflammation.
- To clean the interdental spaces and the space between the denture and the gum (a toothbrush cannot get there), use an irrigator, but only from the 3rd week after installation of the implants. You should start with the initial speed, gradually increasing it.
- Use a mouthwash after every meal. They fight bacteria in the mouth and freshen breath.
- Visit your dentist once every six months for a preventive examination and professional oral hygiene (cleaning your teeth from plaque and tartar).
Is complete prosthetics of the upper jaw different from the treatment of an edentulous lower jaw?
The peculiarity of the upper jaw is that it receives less chewing load and is therefore inferior in density to the lower jaw. Its structure is looser and more susceptible to resorption. For her rehabilitation, the “All-on-six” method is indicated. A larger number of supports is necessary to ensure reliable fixation of the complete bridge.
For the treatment of total adentia of the lower jaw, in most clinical cases, the “All-on-4” concept is optimal, since four are quite enough to support the orthopedic structure.
It is important to know that dental implants take root faster in the lower jaw - in 2-3 months. On the top it is slower - in 5-6 months.
Clinical aspects of revision prosthetics
V. G. Masliy
general dentist, LLC "NEODENT" (Krasnodar)
The durability of artificial restorations in dentistry is limited to a certain service life. The need for repeated prosthetics is caused by imperfect technological processes for the manufacture of orthopedic structures, errors at the clinical stages and individual characteristics of the functioning of the stomatognathic system.
The human dento-alveolar complex undergoes significant changes in the process of ontogenesis. The end of the formation of a permanent bite marks a new stage of development - attraction. The stage of “aging” of the dentition is characterized by a slow progression of physiological abrasion. The response defense mechanism is the synthetic activity of odontoblasts, which results in the deposition of secondary physiological dentin and gradual obliteration of the pulp cavity.
The natural process of attractional development of human dentition is disrupted under the influence of the environment. Factors that have a negative impact include the nature of nutrition, errors in personal hygiene, bad habits, characteristics of professional activity and, paradoxically, the results of iatrogenic interventions.
The dynamics of progressive destruction of the occlusal surfaces of teeth as a result of caries and its complications, as a rule, significantly exceeds the rate of compensatory mechanisms inherent in nature. Secondary deformations of the dentition aggravate the mismatch of the occlusal scheme. As a result, the need for prosthetic restoration arises.
The history of orthopedic dentistry began with timid attempts to restore lost areas of the dentition using prosthetics made of gold, ivory, and ceramics. In 1807, while opening the pyramid of Pharaoh Khephres, who lived 4,500 years ago, the Italian traveler Balzoni discovered a prosthesis near the mummy. According to the researcher, the prosthesis was made of wood.
For a long time, artificial teeth were made arbitrarily, which, of course, gave rise to many errors, and the prostheses themselves were imperfect. The matter advanced after Purman (1648-1721) and Pfaff (1756) began to take impressions of the jaws with wax or sealing wax. Pfaff is also credited with the idea of casting plaster models from impressions. In 1820, Delabar invented and began using impression trays. These events laid the foundation for the precision of dental art.
Technological progress in recent decades has led to the use of artificial supports - implants of various designs in combination with superstructures that imitate the shape and function of the crown of the tooth. How young implantology science is in Russia can be judged by the information presented in the textbook “Orthopedic Dentistry” (A. A. Shcherbakov et al.), published in 1997. I quote: “Many dentists vigorously preach implantation, citing cases of many years of good results. Without denying such observations, we must note that sooner or later the implant will be rejected. This is a biological law, therefore the use of intraosseous implants should be limited to strict indications, which should be further clarified... Therefore, implantation should be recommended in cases where other methods are ineffective.”
Today, hardly anyone would undertake to say this. The results of competent orthopedic rehabilitation of patients using implants are stable and characterized by a high rate of clinical success. Modern dentistry is experiencing an implantological boom. Nevertheless, prosthetic restoration techniques using artificial crowns, bridges on natural supports and various removable structures still remain relevant.
As already noted, throughout life, a person’s dentition is subject to destruction as a result of caries and its complications. In addition, loss of dentition integrity may be associated with the progression of periodontal disease, pathological abrasion and other non-carious lesions. The clinical picture is complicated by primary and secondary occlusal deformities, as a result of which myofunctional disorders develop in some patients. The pathogenetic chain often includes diseases of other organs and systems of the body. Assessing the overall clinical picture, the dentist must decide whether a conformative or reorganizing approach is necessary.
A reorganizing approach to prosthetics involves changing the patient’s occlusal scheme within the compensatory capabilities of the dental system, taking into account individual anatomical and physiological characteristics. In other words, this is a reconstruction of the dentition in the central relationship of the jaws.
The following are the factors that determine the long-term favorable outcome of reconstructive prosthetic rehabilitation:
- Comprehensive diagnostics before the start of treatment with the mandatory production of diagnostic models of the jaws, allowing one to study the individual characteristics of static and dynamic occlusion. Determination and recording of the posterior contact position (centric relation). If myofunctional disorders are present, develop a strategy for their correction.
- X-ray diagnostics. It is difficult to overestimate the importance of an orthopantomogram for making a competent diagnosis and drawing up a treatment plan. In addition, according to indications, TRG and computed tomography data should be studied.
- Forecasting the need for special surgical, therapeutic and orthodontic training with the involvement of related specialists.
- Compliance with the principle of staging of treatment measures with analysis of the results of each stage of therapy.
- Following the concept of completeness of treatment. Dynamic observation lasts until the doctor is convinced that the patient is accustomed to the orthopedic structure, takes regular food, speech and aesthetics are restored, the tissues of the prosthetic bed (mucous membrane, supporting teeth) are healthy, the functions of the temporomandibular joint and masticatory muscles are balanced.
- Agreeing with the patient on a preventive action plan.
To illustrate possible options for implementing the described postulates of orthopedic treatment, I will give a description of two clinical cases of repeated prosthetics from my own practice. The first of them traces the principle of conformativity, while the other uses a reorganizing approach.
Clinical case No. 1
Patient K. came to the clinic with complaints of a fracture of the 22nd tooth, dissatisfaction with the aesthetics of her smile due to the failure of orthopedic restorations in the frontal part of the upper dentition (Fig. 1).
Rice. 1. Appearance of the upper frontal teeth of patient K. before treatment: fracture of the 22nd tooth, disharmony of color and shape.
The general somatic anamnesis is not burdened. Previously, at different times, endodontic treatment was carried out on the 12th, 11th, 21st and 22nd for complicated caries. The 12th and 11th teeth were restored with photopolymer fillings; a veneer was made using CAD/CAM technology on the vestibular surface of the 11th tooth to improve aesthetics. The 21st tooth was restored using a stump pin insert and a metal-ceramic crown.
Upon examination, the coronal part of the 22nd tooth was missing, the fracture line passed at the level of the gum, and the presence of filling material was determined at the mouth of the root canal. The crown parts of the 11th and 21st teeth looked disproportionately large in relation to the adjacent teeth. This was confirmed by an analysis of the aesthetics of the frontal area of the upper dentition. The color of the restorations of the 11th and 21st teeth was monochrome and opaque. The tissues of the devital 12th tooth had a grayish tint, and a zone of hypoplasia was visualized in the cervical area. The fit of the metal-ceramic crown of the 21st tooth was disrupted, and therefore the patient sometimes felt an unpleasant odor.
The radiograph showed incomplete obturation of the root canals of the 12th, 21st and 22nd teeth; in the periapical region of the 12th and 21st teeth, foci of bone tissue destruction without clear boundaries were identified. In the area of the apex of the 11th tooth, a zone of volumetric removal of the sealer was visualized (Fig. 2, 3).
Rice. 2. Orthopantomogram of patient K. before treatment. Rice. 3.
Based on complaints, medical history and examination, the patient was diagnosed with the following: fracture of the crown of the 22nd tooth, discoloration of the 12th, 11th, 21st teeth, chronic periodontitis of the 12th, 11th, 21st and 22nd teeth
.
After discussing various treatment options, a decision was made to repeat endodontic treatment of the 12th, 11th, 21st and 22nd teeth, manufacturing core pin inlays and temporary crowns with subsequent replacement with permanent ones.
The endodontic treatment protocol included unsealing, mechanical and medicinal treatment of the root canals with filling with a mixture based on antibiotics and corticosteroids, and temporary filling with a calcium hydroxide suspension. Permanent obturation was performed using a combined technique of condensation of gutta-percha with AN+ sealer.
Temporary structures were made in the oral cavity from quick-hardening plastic using a wax model and a silicone key (Fig. 4-6). At the stage of immediate prosthetics, the nuances of aesthetics were discussed in detail with the patient and the necessary correction was made. During the treatment process, based on the analysis of pink and white aesthetics, electrosurgical correction of the marginal gum line in the neck of the 12th tooth was performed. The stump pin inlays were made using models made of self-hardening plastic.
Rice. 4 Fig. 5 Fig. 6
After a period of periodontal tissue adaptation, an A-silicone impression was taken from the upper dentition using a one-step method (Fig. 7, 8). All-ceramic permanent crowns on a metal-free frame were made on the master model.
Rice. 7 Fig. 8
The results of prosthetics are presented in Fig. 9-11. The function and aesthetics of the frontal area of the upper dentition have been restored.
Rice. 9 Fig. 10 Fig. eleven
Discussion
For patients with an active social status, camouflage of aesthetic defects in the process of manufacturing permanent orthopedic structures is of great importance. This especially applies to the frontal area of the upper dentition. In this case, in our opinion, the optimal option of immediate prosthetics was chosen, which leveled the emotional discomfort associated with the absence of front teeth.
The direct method of manufacturing core pin inlays allows taking into account the anatomical features of the root, statics and dynamics of occlusion and increases accuracy due to the absence of a transfer laboratory stage.
Repeated prosthetics of the frontal part of the dentition, especially in the presence of failed pins, is associated with the risk of irreversible root destruction during the process of removing the structure. The patient should be warned about this in advance and, if possible, his informed consent should be obtained.
For the restoration of aesthetically significant defects in the dentition, the advantages of metal-free structures are obvious: high biological compatibility, absence of ionic load, excellent optical characteristics.
Planning prosthetic reconstruction of the upper anterior dentition involves a thorough analysis of form and function, including the study of spatial relationships, color scheme, balance of pink and white aesthetics.
The aesthetic result of prosthetics in this situation is quite satisfactory. However, when analyzing the relationships between the ridges of the marginal gum in the area of the central incisors, some asymmetry is revealed. In this regard, the patient was offered the option of aesthetic correction using the electrosurgical method. But at her request, this intervention was postponed for the purpose of dynamic observation. It should be noted that, according to a number of authors, within a year after the manufacture of permanent orthopedic structures, an adaptive restructuring of the keratinized gum occurs. Therefore, the final decision on the need for correction can be postponed.
Clinical case No. 2
Patient A. came to the clinic with complaints about the mobility of the metal-ceramic bridge prosthesis, which replenishes the integrity of the frontal portion of the upper jaw dentition, and the associated sensation of unpleasant odor. The bridge was made about a year ago in another clinic, mobility began a few months later. In addition, the patient was periodically bothered by spontaneous pain in the area of the upper lateral teeth on the right, which was aggravated by irritants. The general somatic anamnesis is not burdened.
An external examination revealed no signs of pathology. Examination of the dentition showed the presence of secondary carious lesions on the 16th, 15th and 14th teeth. In the 15th tooth, the secondary carious cavity communicated with the pulp cavity, probing and the cold thermal test were painful, the aftereffect symptom and percussion test were positive. Clinical signs of damage to the pulp of the 16th and 14th teeth were not determined.
One tooth was missing in the lower incisor group. Considering the presence of a slight trema between the canine and the left incisor, the increased distance between the roots of the teeth in this area on the orthopantomogram and the high frequency of edentulous lateral incisors, it was concluded that the left lateral incisor was absent. The cause of adentia could not be determined from the anamnesis.
The fixation of the metal-ceramic bridge supported by the 13th, 21st and 22nd teeth was disturbed, the greatest mobility was detected in the area of the 13th tooth. On the intermediate part in the area of the medial corner of the artificial 11th tooth, a chip of the ceramic coating was visualized.
Stamped-soldered bridges, which filled the integrity of the lateral sections of the upper and lower dentition, were untenable due to a violation of the marginal fit and a change in the classic signs of the occlusal scheme. The largest number of occlusal contacts was identified in the frontal area. In the lateral region on the right, secondary occlusal deformation was detected: the 16th tooth was in infraposition. When studying occlusion in dynamics, a decrease in the trajectory of the sagittal incisal path and the absence of canine protection or group guiding function on the right and left were determined in the presence of balancing and protrusive supercontacts in the molar area.
The identified violations of the occlusal scheme were due to the reduction of the anatomical zones of the lower teeth: the cutting edges of the incisors, the cusps of the canines and the buccal cusps of the premolars - as a result of abrasion. In addition, previous prosthetics played a certain role in this: errors in modeling restorations and iatrogenic changes in the profile of the Spee curve (on the right - excessive deepening associated with the Popov phenomenon in the area of the 16th tooth, and on the left - flattening).
It is likely that the mismatch of the occlusal scheme was also one of the reasons for the chipping of the ceramic coating and the decementing of the bridge.
There were no signs of TMJ dysfunction.
Based on the clinical examination data and analysis of the results of additional research methods (Fig. 12-17), the patient was given the following diagnosis: partial secondary edentia of the upper jaw - class II and the lower jaw - class III according to Kennedy, filled with a metal-ceramic bridge in the frontal region and stamped - soldered bridges in the lateral sections; complications of the underlying disease - secondary occlusal deformation (infraposition of the 16th tooth); increased abrasion, horizontal shape; chronic pulpitis of the 15th tooth, chronic periodontitis of the 13th, 21, 22, 24, 36, 45th teeth, secondary dentin caries of the 14th, 23rd and 16th teeth; mild chronic generalized periodontitis.
Rice. 12 Fig. 13 Fig. 14 Fig. 15 Fig. 16 Fig. 17
The treatment plan included professional hygiene measures, sanitation of carious lesions, removal of bridges, endodontic preparation of abutment teeth and restoration of the integrity of the dentition with fixed orthopedic structures. For financial reasons, the patient rejected the treatment option using implants.
After an attempt at endodontic treatment of the 36th tooth, a decision was made to remove it due to obliteration of the apical third of the canals and the presence of signs of internal resorption. In addition, on the orthopantomogram, in the area of the apex of the medial root of the 36th tooth, a focus of bone tissue destruction with fairly clear boundaries was visualized.
Endodontic preparation of the supporting teeth was carried out using routine methods using mechanical root canal treatment and delayed obturation with temporary filling with a calcium hydroxide suspension and, if indicated, an antibiotic and corticosteroid-based gel. During the treatment, the failed stump pin inlays were removed from the 13th and 22nd teeth. There was a silver pin in the canal of the 21st tooth, which was also removed (Fig. 18-21).
Rice. 18 Fig. 19 Fig. 20 Fig. 21
Reinforcement of the stumps of the 13th, 21st, 22nd, 23rd, 24th, 25th, 35th and 45th teeth was performed using inlays. A special composite was used to fill the endodontic access cavities in teeth 27, 38 and 48.
In order to correct secondary occlusal deformation, endodontic treatment and selective grinding of the 16th tooth were performed.
After determining and recording the central ratio, we began to restore the functional integrity of the dentition. Orthopedic treatment was carried out in two stages. At the first stage, orthopedic structures were performed in the lateral sections, using a silicone key, the cutting edges of the lower incisors, cusps of the canines and premolars were restored, and a temporary bridge was made in the frontal area of the upper dentition (Fig. 22-24).
Rice. 22 Fig. 23 Fig. 24
In order to improve the aesthetics of the soft tissues, plastic surgery of the frenulum of the upper lip was performed. The gum profile in the area of the missing 11th and 12th teeth was formed using the electrosurgical method with correction of the intermediate part of the temporary bridge using a composite. After the epithelization process was completed, a metal-ceramic bridge prosthesis was made taking into account the individual characteristics and wishes of the patient (Fig. 25, 26).
Rice. 25 Fig. 26
After completion of treatment measures, an orthopantomogram was performed to monitor long-term results over time (Fig. 27).
Rice. 27
Discussion
The presented clinical case clearly demonstrates the importance of including the production of diagnostic jaw models in the routine dental examination.
In this situation, before the start of treatment, the patient complained of pain associated with the pathology of the pulp of the 15th tooth. In addition, she was not satisfied with the aesthetics of the metal-ceramic bridge prosthesis in the frontal area of the upper dentition and was concerned about the discomfort caused by the decementation of the orthopedic structure.
During the diagnostic process, the feasibility of comprehensive dental rehabilitation, which included the replacement of failed orthopedic restorations in the lateral regions, was shown and justified. The purpose of this intervention was to correct the occlusal pattern with improving the profile of the curve of Spee and creating a group guiding function during eccentric movements of the lower jaw.
This approach is dictated by the need to extend the service life of the metal-ceramic prosthesis in the frontal part of the upper dentition by reducing the risk of chipping and functional load on the tissue of the roots of abutment teeth. A sufficient length of the intra-root parts of the pin inlays should also ensure optimal distribution of internal stresses.
It should be recognized that a longer-lasting result of the reconstruction of the dentition of this patient would have been ensured by the use of implants in the positions of the 11th, 12th, 36th, 37th, 46th and 47th teeth. When discussing a treatment plan, it is always necessary to emphasize the advantages of replacing missing teeth with artificial crowns on implants, which include improved hygiene, elimination of overload of natural teeth and the ability to replace individual elements without damaging the structure as a whole.
Numerous experimental data and long-term clinical observations suggest that the use of bridges supported by natural teeth is a compromise method of orthopedic treatment.
However, with strict adherence to the technological requirements for the manufacture of artificial crowns and bridges on natural supports, and protocols for special therapeutic and surgical preparation, this method provides a stable and long-lasting treatment result.
Kinds
Completely removable dentures are preferably placed if absolute adentia is diagnosed in the dentition or contraindications are identified during diagnosis that do not allow the installation of fixed dentures (crowns, bridges). Removable structures are attached either to the gum (lower jaw) or to the gum + palate (edentulous upper jaw). There is another way of fixation: on implants.
They are classified according to the principle of fastening:
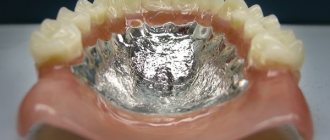
- partial removable dentures (fixed in the oral cavity with the help of hooks that cling to the “native” teeth or implants. Nylon and plastic are used to make the prosthesis, sometimes a metal base is added. Such dentures are called clasp dentures);
- complete (installed when there is a complete absence of teeth in a row. The design is not reliable in terms of fastening, since there is no base for fixation. It is made of plastic. Removable dentures also include conditionally removable ones - they are attached to small implants implanted in the jaw).
In addition to the materials already mentioned, removable dentures are made of acrylic - a fairly reliable material, which, when installed correctly, looks quite aesthetically pleasing, and if the parameters are correctly selected, the design does not cause severe discomfort during adaptation.
For fastening the prosthesis, beam fasteners are often chosen. The beam is designed to carry a vertical load. The issue of load distribution is especially acute if “natural” teeth or implants are chosen for support. This fixation is reliable due to special recesses in the beam and locks in the structure. This device is used for complete and partial edentia.
Types of edentia
Adentia is the absence of teeth in the oral cavity. There are several types:
- Primary: when the patient initially did not have a permanent or baby tooth germ.
- Secondary: the tooth erupted, but after some time was removed (due to injury or caries and its complications).
Also distinguished:
- complete edentia: all teeth in the mouth are missing;
- partial (incomplete): one or more were removed.
Treatment and dental prosthetics are carried out only after diagnosis. It is important for the doctor to assess the condition of the gums and bone tissue. The treatment and prosthetic plan will depend on this.