In case of problems with the facial muscles, you will need to be examined by a neurologist; if any studies have been previously performed, be sure to take their results for consultation, incl. the pictures themselves. If studies have not been performed, they will be recommended and performed based on the results of the examination.
- Facial hyperkinesis.
- Facial hemispasm.
- Facial paraspasm.
- Blepharospasm.
- Examination for facial hyperkinesis.
- How to stop facial hyperkinesis. Administration of Botulinum toxin A.
- Treatment of facial muscle spasms.
Facial hyperkinesis
Facial hemispasm and paraspasm, blepharospasm are diseases associated with uncontrolled contraction of facial muscles. They are very similar to neuropathy, neuritis, and facial nerve paresis.
Facial muscle control is structured as follows:
- Nerve cells of the cortex and subcortical nuclei of the brain send nerve impulses to the brain stem, to the control centers of the facial nerve;
- These centers distribute impulses along the nerve fibers and send them along the nerve, like an electrical cable, directly to the facial muscles;
- Each tiny nerve fiber causes its own microscopic section of muscle to contract.
Causes of facial hyperkinesis:
- An error in the functioning of the subcortical nuclei of the brain, as a result of which excess uncontrolled nerve impulses are sent to the facial muscles, which lead to spasm;
- Excessive stimulation of the facial nerve centers in the brain stem;
- Irritation of the facial nerve itself after it leaves the brain.
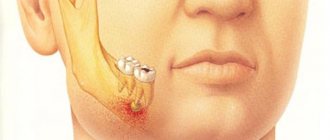
In the first and second cases, this is the result of damage to the nucleus or center due to neuroinfection, multiple sclerosis, blood supply deficiency or tumor. In the third case, the disease occurs even with slight compression of the root of the facial nerve in the area of its exit to the base of the brain by an altered vessel (entanglement of the nerve by an artery), a tumor, or compression in the thickness of the parotid salivary gland in some of its diseases.
Even doctors often confuse facial hyperkinesis with neuropathy, neuritis of the facial nerve. We will definitely understand the causes of the disease and provide the necessary treatment.
Facial hemispasm
Facial hemispasm (hemifacial spasm, Brissot's disease) is a symptom complex of unilateral hyperactive dysfunction of the facial nerve, which develops as a result of compression of the facial nerve root in the area of its exit from the brain stem. It is characterized by the appearance of moderate and intermittent painless convulsions (tonic or clonic) in the orbicularis oculi muscle, gradually progressing in frequency and strength of contractions with the gradual involvement of all facial muscles. The duration of the attack can reach several hours. As the disease develops, a tonic half-mask appears on half the face: narrowing of the palpebral fissure, tightening of the nasolabial fold, tension of the subcutaneous muscle of the neck. Sometimes the attack is interrupted by pressing on the brow ridge or other part of the face. There are typical hemifacial spasms (starts in the orbicularis oculi muscle and then involves all the underlying facial muscles of half the face) and atypical (starts from the muscles of the cheek and gradually involves all the overlying facial muscles). Hemispasm can be combined with trigeminal neuralgia, and unilateral dysfunction of the auditory nerve is possible.
The prevalence of the disease is 8 patients with hemifacial spasm per 1 million population. Women are 2 times more likely to get sick.
Pathogenesis
Typically, the cause of facial muscle twitching is compression of the facial nerve root by a vessel. Most often this is the anterior inferior cerebellar artery, less often - other intracranial arteries. In isolated cases, compression by vascular malformations or veins is possible. With hemifacial spasm, the vessel compresses the complex of the facial and auditory nerves. Rare causes of hemifacial spasm are considered to be benign tumors or cysts of the cerebellopontine angle, multiple sclerosis, cicatricial adhesions of various origins, and bone deformities of the temporal bone pyramid. An even rarer cause of hemifacial spasm is Chiari malformation.
Diagnostics
The diagnosis of hemifacial spasm is made based on the patient’s complaints and the clinical picture of the disease. Hemifacial spasm usually begins from the lower eyelid on one side of the face, and as the disease progresses, it gradually spreads to the muscles of the cheek, chin and neck; At the beginning of the disease, convulsions are clonic, then they acquire a tonic-clonic character.
The value of instrumental research methods is insignificant, and only allows one to exclude or confirm the presence of a space-occupying formation of the cerebellopontine angle: the area in the cranial cavity where the root of the facial nerve is located. MRI allows us to identify the close location of the vessel and the facial nerve, while the neurovascular conflict in patients suffering from facial hemispasm is not always detected.
Treatment
Traditionally, vascular and anticonvulsant drugs are used, the effect of which is observed in approximately 20% of patients. At the onset of the disease, it is often possible to conduct courses of acupuncture, which in some cases provide a short-term positive effect.
Recently, symptomatic treatment through regular (2-3 times a year) injection of botulinum toxin into the facial muscles has become increasingly common. The therapeutic effect of botulinum toxin injections of varying severity lasts up to 18 weeks, so patients need to repeat them. In this case, the time intervals between injections, during which there are no twitches of the facial muscles, can gradually decrease.
If conservative treatment of hemifacial spasm is ineffective, surgical treatment is used: vascular decompression of the facial nerve root using microsurgical techniques, which in most cases eliminates the cause of the disease and achieves significant relief of symptoms or recovery.
Examination for facial hyperkinesis
The success of treatment directly depends on an accurate diagnosis of the location and cause of damage to the pathways and brain centers of the facial nerve. Therefore, we carefully examine each patient. Your doctor will determine the cause of excessive stimulation of the facial muscles, and based on the data obtained, select the most effective treatment.
MRI and X-ray computed tomography of the brain and facial skull. On tomograms, especially if they are performed with preliminary contrast, the brain centers of the facial nerve and its area of exit (root) to the base of the brain, blood vessels, and skull bones are visible. They help to see the cause of compression of the facial nerve root and evaluate the structure of the salivary glands. Circulatory disorders, cysts and tumors are easily recognized.
Blood tests to check for infections and biochemical changes that damage the brain and facial nerve. The suspicion of the presence of a neuroinfection and its activity can be easily verified using a blood test.
Electromyography, Blink reflex - electrophysiological techniques based on measuring the electrical potentials of the facial muscles. They help assess the function of impulse transmission along the facial nerve, the degree of its impairment, judge the effectiveness of treatment, the presence of complications, and help in choosing the correct treatment tactics.
Symptoms
Involuntary movements of the facial muscles are the only symptom of hemifacial spasm. Fatigue, anxiety or reading can speed up movements. Spontaneous hemifacial spasm involves facial spasms, which are myoclonic spasms and are similar to segmental myoclonus, which can occur in other parts of the body. Postparalytic hemifacial spasm, such as after Bell's palsy, manifests as facial synkinesis and contracture.
There are a number of conditions similar to hemifacial spasm.
Spasm of the masticatory muscle
Hemispasm of the masticatory muscle is similar to hemifacial spasm and occurs when the motor trigeminal nerve is irritated. This is a rare condition that is segmental myoclonus, and is manifested by unilateral involuntary contractions of the muscles innervated by the trigeminal nerve (mastication). As with hemifacial spasm, hemispasm of the masseter muscle is well treated with medication and botulinum toxin. In addition, there is evidence that surgical treatment may be effective in some cases.
Myoclonic movements
Myoclonic movements in the facial muscles can also occur with lesions of the brain or brain stem. They differ from hemifacial spasm in the distribution of abnormal movements (more generalized, possibly bilateral), and can be diagnosed by neurophysiology. Imaging techniques can reveal deeper causes. Central myoclonus responds well to anticonvulsant therapy.
Oromandibular dystonia
Oromandibular dystonia is a muscular dystonia that affects the lower musculature of the face, primarily the jaw, pharynx and tongue. When oromandibular dystonia occurs in combination with blepharospasm, it is called Medge's syndrome.
Botulinum therapy is most effective in the treatment of oromandibular dystonia. Medications are also used to a certain extent for oromandibular dystonia.
Craniofacial tremor
Craniofacial tremor may be associated with essential tremor, Parkinson's disease, thyroid dysfunction, and electrolyte imbalances. This condition rarely occurs in isolation. Focal motor seizures sometimes need to be distinguished from other facial movement disorders, particularly hemifacial spasm. Postictal weakness and increased involvement of the lower face are hallmarks of focal motor seizures.
Chorea of the face
Facial chorea occurs in the context of a systemic movement disorder (eg, Huntington's disease, Sydenham's chorea). Chorea is an episodic complex of movements without a pattern. A similar condition, spontaneous orofacial dyskinesia, occurs in older edentulous people. As a rule, the installation of prostheses gives a good effect.
Tiki
Facial tics are short, repetitive, coordinated spontaneous movements of grouped muscles of the face and neck. Tics may occur physiologically or due to diffuse encephalopathy. Some medications (eg, anticonvulsants, caffeine, methylphenidate, antiparkinsonian drugs) may cause tics. Single, repetitive, stereotypical movements are characteristic of tics.
Facial myokymia
Facial myokymia manifests itself as worm-like twitching under the skin, often with a wave-like distribution. This condition is distinguished from other abnormal facial movements by the characteristic EMG discharges, which are short, repeated bursts of motor unit potentials in the range of 2-60 Hz, with periods of silence of up to several seconds. Facial myokymia can occur with any process in the brain stem. Most cases of facial myokymia are idiopathic and resolve on their own within a few weeks.
How to stop facial hyperkinesis. Administration of Botulinum toxin A
Botulinum toxin A (Botox, Dysport) is a means of reducing the excitability of the muscles involved in hyperkinesis. The drug is one of the most convenient options for the symptomatic treatment of spasms of the muscles of the face and eyes, and other hyperkinesis. We inject Botulinum Toxin A using a syringe with a very thin needle directly into the affected muscle, after which the muscle stops engaging in tics or other hyperkinesis. The effect develops within 3-5 days and lasts up to 4-8 months. During this time, a course of treatment of the causes of the disease and rehabilitation procedures (massage, gymnastics, physiotherapy, psychotherapy, cosmetic procedures) are carried out.
Treatment of facial muscle spasms
Depending on the detected causes of the disease, your doctor will choose the appropriate combination from a wide range of treatment methods:
- Prescription of drug therapy aimed at reducing irritation of the facial nerve root, restoring blood supply, eliminating infection if it is detected;
- Injection of Botulinum toxin A into muscles subject to involuntary contractions;
- Acupuncture, massage, gymnastics;
- Special neuropsychological gymnastics, which allows you to normalize the relationships between different parts of the brain;
- Carrying out neurosurgical intervention to eliminate contact between the modified vessel and the root of the facial nerve (microvascular decompression) or remove the tumor.
Facial nerve paralysis
With facial paralysis, movement in the right or left side of the face is usually impaired. Main causes of the disease:
- Infections: chickenpox, herpes, cytomegalovirus infection, rubella, influenza and other acute respiratory viral infections;
- Meningitis and meningoencephalitis - inflammation of the brain and its membranes;
- Traumatic brain injuries. Most often, facial nerve paralysis develops after a brain contusion or a fracture of the base of the skull;
- Brain tumors;
- Otitis media is an inflammation of the middle ear (tympanic cavity).
If the cause of the disease cannot be determined, the doctor will diagnose idiopathic facial paralysis, which is also called Bell's palsy. It occurs in approximately 50%-80% of cases. Typically, Bell's palsy begins suddenly, and disturbances worsen over 2 days (48 hours). May cause headaches, weakness, pain behind the ear, decreased taste sensitivity and increased sensitivity to sounds.
With facial nerve paralysis, facial expressions are weakened, usually on one half of the face. When the patient tries to smile, bare his teeth, open his mouth or close his eyes, the face becomes asymmetrical and distorted. The eye on the affected side is constantly open.
At the appointment, the neurologist interviews and examines the patient. It is important for the doctor to understand when and how the disorders appeared, what preceded them, and what other diseases the patient has. During the examination, the neurologist identifies dysfunctions of the facial and masticatory muscles.
After this, the doctor prescribes an examination. This may include:
- Electromyography. A study during which a special device records electrical impulses from facial muscles;
- Magnetic resonance imaging (MRI). This study helps identify the pathological changes that led to paralysis.
Treatment
- Exercises for facial muscles;
- Face massage;
- Physiotherapy;
- Anti-inflammatory therapy: glucocorticosteroids are used - hormonal agents that suppress immune and inflammatory reactions;
- Antiviral and antibacterial agents, if paralysis occurs due to infection;
- Eye protection on the affected side. With facial paralysis, the patient cannot close his eyes. To protect it, moisturizing drops (“artificial tears”), eye ointments with antibiotics, and a special “glass” bandage are used.
What is the risk of the disease?
If you immediately consult a doctor and begin treatment, the function of the nerve can be restored completely or at least partially. If treatment is not carried out on time, then paralysis can last a lifetime. The eye on the affected side will suffer the most. Due to the fact that the patient cannot close his eyelids and blink, the conjunctiva and cornea are not moistened with tears, they dry out. Vision decreases to the point of complete blindness.