Chronic periodontitis: description and symptoms
Unlike acute periodontitis, chronic periodontitis is often practically asymptomatic, that is, it is not accompanied by severe swelling and severe pain. That is why many patients come to the doctor when conservative treatment of chronic periodontitis is impossible, and to eliminate complications they have to resort to more radical measures. Chronic periodontitis in the acute stage has much more pronounced symptoms.
Symptoms of chronic periodontitis
- pain
- soft tissue swelling
- tooth mobility
- enlarged lymph nodes
- weakness
- temperature increase
Exacerbation of chronic periodontitis is often associated with concomitant diseases, as well as hypothermia, decreased immunity and other factors.
Symptoms
In the acute form of the disease, the symptoms manifest themselves most clearly:
- there are pain sensations in the area of the injured tooth (intensified by the slightest external mechanical influence - closing teeth, touching, chewing load);
- the tooth becomes mobile - with traumatic periodontitis, mobility can change towards decreasing or increasing;
- a change in the color of the tooth is observed - but the tissues are not always stained, but with extensive hemorrhage due to rupture of the vessels that pass through the apical opening of the root.
The chronic form of the disease does not have such severe symptoms. A person may experience slight pain when tapping on the causative tooth. In an advanced state of traumatic periodontitis, tooth mobility progresses - it can tilt or shift.
Causes of chronic periodontitis
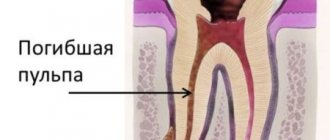
Chronic apical periodontitis (chronic apical periodontitis, chronic root periodontitis) is so named because the inflammatory process occurs in the area of the apex of the tooth root. This type of disease is often the next stage of the acute form, but it can also develop independently. Based on their origin, experts distinguish two types of chronic periodontitis.
✔
Infectious chronic periodontitis. Occurs as a result of the activity of pathogenic bacteria in the oral cavity. The presence of foci of infection contributes to the penetration of bacteria into periodontal tissue and the development of the disease.
✔
Non-infectious chronic periodontitis. It can be caused by trauma and mechanical damage to the teeth, including due to doctor errors during therapeutic treatment. Another reason may be an allergic reaction to medications (in particular, arsenic and anesthetics), as well as the toxic effects of pulp decay products.
Causes of periodontitis
The etiology of periodontitis in most cases is associated with advanced forms of caries. When the pulp is damaged, the inflammation spreads to the root of the tooth and then spreads through the canal to the periodontium. In addition, the causes of the disease can be:
- tooth trauma - fracture or crack of the root, bruise, chipped crown with subsequent penetration of infection into the pulp;
- violation of the root canal treatment technique with tissue injury with sharp instruments;
- violation of the root canal filling technique with filling material extending beyond the root apex;
It is important for the dentist to find out the cause of periodontal inflammation in order to select the optimal treatment regimen for the tooth and prevent relapse.
Diagnosis of chronic periodontitis
Unfortunately, without the necessary equipment, it is very difficult to identify chronic periodontitis. A visual examination performs a purely formal function, since even in the presence of symptoms (pain, swelling, etc.), it is necessary to determine the type and stage of periodontitis in order to draw up the most effective treatment plan. Today, diagnosis of the disease is carried out in several proven ways.
- X-ray examination. The most popular type of diagnostics. All types of chronic periodontitis can most often be detected on a regular targeted X-ray. In case of fistula formation, a narrow-profile X-ray examination - fistulography - is often prescribed.
- Radiovisiographic examination. A more modern and gentle x-ray examination, during which the image is transferred to a computer screen.
- Electroodontodiagnosis (EDD). Diagnosis of inflammatory processes in the dental pulp by monitoring its response to electric current.
- In the case of periodontitis, specialists use differential diagnosis to distinguish it from other dental diseases with similar symptoms.
Diagnosis of the disease
To establish a complete clinical picture, the dentist-therapist conducts an initial survey of the patient and collects a complete medical history. Then a visual examination is carried out, which makes it possible to determine whether there are ulcers and inflammations in the oral cavity, as well as to determine the color of the gums, the angle of displacement and/or inclination of the tooth, the integrity and color of the enamel.
Additional examination may include the following methods:
- Radiography is used to diagnose the chronic form of traumatic periodontitis. The diagnosis is made based on the detected changes in the tissues surrounding the diseased tooth and the condition of its roots.
- Electroodontodiagnosis - helps to assess the condition of the pulp in order to ensure a reliable and effective treatment result, to avoid inflammation and other complications.
Chronic forms of periodontitis
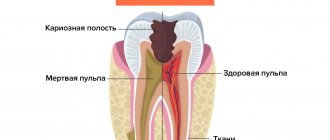
Chronic fibrous periodontitis
Periodontal tissues are gradually replaced by connective tissue, and the inflammatory process is usually mild. One of the most common types of periodontitis, which is most often asymptomatic. With exacerbation, pain, enlarged lymph nodes and fever are possible. When diagnosed on an x-ray, you can notice an expansion of the periodontal fissure.
Treatment of chronic fibrous periodontitis is usually easier compared to other forms.
Chronic granulating periodontitis (chronic granular periodontitis)
In the apical region of the root, granulation tissue is formed, which actively replaces bone. In terms of symptoms, this is the most pronounced type of chronic periodontitis, which manifests itself in the form of pain, especially when pressing on a tooth or biting. During an exacerbation, the pain intensifies, and fistulas with purulent discharge may occur. On an x-ray, it is quite easy to notice dark, irregularly shaped areas: clear evidence of the development of granulating periodontitis. It is advisable to treat chronic granulating periodontitis quickly enough to avoid the spread of granulation tissue.
Chronic granulomatous periodontitis
A type of periodontitis in which a purulent sac forms near the tip of the root, which, as it grows, first turns into a granuloma, and then into a cyst filled with dense epithelial tissue. The diameter of the cyst can exceed 1 centimeter. In the early stages it hardly manifests itself, but in later stages pain occurs, and the color of the tooth may also change. On x-ray it appears as a dark round spot. Treatment of chronic granulomatous periodontitis in some cases requires surgical intervention, since it is often not possible to get rid of the cyst using conservative methods.
Classification of periodontitis
Periodontitis occurs in different forms: with virtually no symptoms, mild or with severe inflammation.
Depending on how the disease develops, chronic
and
acute periodontitis
. Each has its own characteristics.
Chronic periodontitis
It is not easy to identify chronic periodontitis, since there are either no signs of pathology at all or they are difficult to distinguish. If a person does not visit the dentist regularly, there is a high probability of developing the disease.
Signs that may indicate chronic periodontitis:
- discomfort when eating or drinking hot food;
- pain, moderate or weak, when affecting the tooth: brushing, tapping, biting hard foods (for example, apples).
The final verdict will be made by the doctor during the examination. He will take an x-ray and use the image to determine the form of chronic periodontitis. There are three in total:
- granulomatous.
Pus accumulates inside the tissues and periodically comes out through the resulting fistula. If left untreated, the following may form at the site of inflammation:
- granulomas (inflamed nodules) with a diameter of up to 5 mm;
- cystogranulomas with diameters from 5 mm to 1 cm;
- cysts from 1 cm in diameter.
This form is one of the most dangerous and requires prompt medical intervention.
- granulating.
It develops quickly and is characterized by the destruction of bone tissue around the apex of the tooth root. The source of inflammation resembles a blurred candle flame without clear contours.
Some of the characteristic signs are: pliable gums (if you press on it, the hole will not disappear immediately), a feeling of heaviness inside the gums, tooth pain when eating.
- fibrous.
The most hidden type of the disease, since in most cases it is asymptomatic. Later, an unpleasant odor (gangrenous, or the smell of decomposition), discoloration of the tooth and death of the pulp may appear.
X-rays help determine fibrous periodontitis.
Chronic periodontitis can worsen, taking the form of acute periodontitis. The causes of complications are, as a rule, diseases that have reduced immunity, or hypothermia.
If the accumulated pus comes out from the source of inflammation, periodontitis will again take a chronic form. But not for long - after some time the exacerbation will repeat.
Treatment is carried out in several stages and begins with removal of pus
Acute periodontitis
The acute form of periodontitis occurs clearly, forcing the patient to think about dental treatment. Signs can be both external and internal. The most characteristic ones include:
- swollen or swollen cheek;
- swollen gums;
- wobbly crown;
- pain in the tooth and gum;
- pain when eating;
- drowsiness, malaise, fatigue;
- poor sleep;
- elevated temperature;
- passing pain: from aching to throbbing.
Suppuration occurs at the root of the tooth, visible only on an x-ray. During the initial examination of the oral cavity, the affected tooth almost always shows: caries, reddened and inflamed gums, mobility of the diseased area (the feeling that the tooth has moved out of the jaw).
Treatment of chronic periodontitis on teeth
Despite the fact that acute and chronic periodontitis are similar in many ways, treatment of chronic forms of periodontitis is usually more difficult and takes longer than the acute form. Treatment of acute chronic periodontitis is most often carried out using conservative methods and may require endodontic intervention: opening the tooth cavity to drain purulent exudate, filling the canals. Antiseptic drugs and antibiotics are also actively used. In the case of chronic periodontitis, the treatment method depends on the stage of the disease and the presence/absence of complications. Based on this, a conservative or surgical treatment plan is drawn up.
Treatment methods for chronic periodontitis
✔
Conservative treatment of chronic periodontitis. It implies a whole range of measures to eliminate the source of the disease. First of all, the tooth canals are cleaned, antiseptic medications are administered, and anti-inflammatory drugs and antibiotics are taken if necessary. After sanitation, the canals are filled with medicinal filling paste, after which it is necessary to wait for the restoration of periodontal tissue for 1 to 3 months. After this period is completed, a permanent filling is performed. In the treatment process, techniques such as electrophoresis, laser and UHF therapy are often used.
✔
Surgical treatment of chronic periodontitis. Surgical methods for treating chronic periodontitis one way or another involve invasive intervention in periodontal tissue. Typically, this technique is used in advanced stages of periodontitis and when complications develop (cysts, fistulas, etc.). Modern dentistry has a number of surgical techniques that allow you to save part of a root or tooth. These include: tooth root resection (removal of part of the root along with a pathological formation), cystectomy (operation to remove cysts and granulomas), and hemisection (removal of the crown part of a multi-rooted tooth along with the root). Despite the fact that chronic periodontitis of permanent teeth is most often tried to be cured with the help of tooth-preserving manipulations, in the most severe cases complete tooth extraction is indicated.
Treatment of periodontitis
Treatment of periodontitis
Treatment of periodontitis is determined by the development of the clinical picture. As a rule, it includes several stages with x-ray examination, a combination of medication and surgical intervention.
In advanced forms, a course of antibiotics may be prescribed, and physiotherapeutic procedures are also recommended.
The standard course of treatment consists of the following stages:
- Preliminary examination, identification of the form of the disease and the extent of damage.
- Cleaning of dental canals, treating them with antiseptic preparations.
- If necessary, dissection of the gums to drain the pus.
- Repeated cleaning of the canals, control x-ray or panoramic tomography.
- Installation of a temporary filling with a medicinal composition to eliminate the effects of inflammation.
- Removing the filling after 1-2 days, cleaning the cavity with an antiseptic. The procedure is repeated until the dentist is sure that all traces of suppuration have been removed and the possibility of relapse is minimized.
- Installation of a capital seal.
Even an experienced dentist will not give specific treatment dates in advance. Some cases of periodontitis are treated in one to two weeks, sometimes treatment lasts several months. It is most difficult to treat chronic forms, when it is impossible to do without surgical intervention, and symptoms may not manifest themselves for a long time.
It must be remembered that curing periodontitis in one visit is not only impossible, but also potentially dangerous. Dental canals that are not completely cleaned of pus can lead to extensive sepsis, which will spread to the internal organs and lead to hospitalization.
It is very important to follow the doctor’s instructions throughout the entire treatment period - rinse your mouth with medicinal compounds, make special baths, use antibacterial and analgesic ointments.
As an additional measure in the treatment of periodontitis, physiotherapy can be prescribed: UHF and electrophoresis.
Repeated treatment of chronic periodontitis
Sometimes specialists have to re-treat chronic periodontitis. This is usually due to the fact that previous treatment was ineffective. This could be poor cleaning and filling of canals, defects during surgical procedures, non-compliance by the patient with rehabilitation rules, as well as an initially incorrectly selected treatment plan. Secondary treatment almost always takes longer and is more difficult. In this case, it is still possible to do without tooth extraction or carry out repeated conservative treatment, however, quite often the patient comes with already developed complications that require surgical intervention.
Complications
If untimely or incorrectly treated, periodontitis can lead to extensive purulent inflammation and the appearance of multiple ulcers, abscesses and fistulas.
As a result, there is a very serious risk of developing dangerous diseases such as:
- periostitis (flux);
- dental cyst;
- osteomyelitis;
- blood poisoning.
The consequences of each of the complications can be very serious, often accompanied by hospitalization and surgery. Therefore, it is very important to diagnose periodontitis in a timely manner and begin its treatment.
Chronic periodontitis: treatment at home
Any form of periodontitis cannot be cured at home: this should only be done by a professional doctor. The only option is antibiotic therapy, which in the vast majority of cases is prescribed as an addition to complex treatment. The same applies to traditional medicine. In medical practice, there have been cases when a cyst or granuloma resolved without any intervention, but this should not be attributed to miraculous natural decoctions and tinctures. Much more important are preventive measures that will help improve oral health and avoid problems with teeth and gums. In this case, some traditional medicine can really help, but the main measures to prevent periodontitis are good hygiene, proper nutrition and regular visits to the dentist.
Prevention
Traumatic periodontitis is easier to prevent than to endure pain and risk serious complications. It is necessary to avoid any dental injuries and contact a dentist at the first sign of overload due to improper installation of a filling or orthopedic structure. Those who like to bite thread with their teeth, open bottles, crack nuts, bite a pencil, etc. These habits should be abandoned, especially if the teeth are pulpless. Without a nerve, teeth become more fragile than living ones, and even a small load is enough for chipping to occur at the gum level and traumatic periodontitis developing.
Still have questions?