Dentistry / Dentistry for pregnant women / Pain relief during pregnancy
One of the most common questions that specialists from SCNT “NOVOSTOM” have to answer is the possibility of using painkillers by pregnant women. Alas, it is impossible to answer unequivocally.
Pregnancy provokes hormonal changes in a woman’s body. And problems with teeth against this background are not uncommon. In this case, the body works on the principle “all the best goes to the child,” which is why women often experience a lack of nutrients, including calcium, which is necessary for teeth. In addition, if the oral cavity has not been sanitized, during pregnancy the process of reproduction of harmful bacteria is activated.
Dentists at the NOVOSTOM clinic recommend seeking professional orthodontic treatment immediately after the first symptoms occur. The discomfort a woman experiences due to toothache has a negative impact on the fetus. Therefore, it is better to immediately contact a specialist. But if this is not possible, you may need to take painkillers.
Introduction
Migraine is a common primary form of headache (TH), which manifests itself in the form of repeated attacks, often accompanied by nausea, vomiting, photo- and phonophobia.
The prevalence of migraine, according to various estimates, ranges from 2.6% to 21.7%, and the average rate is 14.7% [1]. In Russia, the prevalence of migraine reaches 20.8%, which is approximately more than 30 million people [2]. The prevalence of migraine in women is more than 2 times higher than that in men, and the highest prevalence of migraine within the female population occurs during reproductive age [3]. For this reason, issues of tactics for managing patients with migraine during pregnancy are of high relevance. Issues of pregnancy planning, as well as rules for taking medications for pain relief and approaches to preventive treatment of migraine during pregnancy are discussed very often.
Directions for use and dosage during pregnancy
During pregnancy, with uterine hypertonicity, it is permissible to take 6 drotaverine tablets per day. The drug is taken three times a day: two tablets in the morning, afternoon and evening. The safety of the drug for pregnant women has been confirmed by clinical trials: an experiment was conducted in Hungary in which a group of 30 pregnant women regularly taking No-Shpu was examined. No pathologies were identified in newborns; in addition, taking No-Shpa allowed the heart rhythm of children with tachycardia to be normalized.
The course of migraine during pregnancy
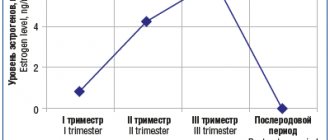
In 50–70% of women during pregnancy, migraine without aura improves [4]. Migraine attacks become mild, extremely rare, and in most patients in this group the migraine completely disappears. Improvement occurs after the first trimester, starting from the 12th–14th week. pregnancy. This is due to the fact that by the beginning of the second trimester, the level of estrogen stabilizes and begins to increase, and its fluctuations stop (Fig. 1). Migraine with aura stops less often during pregnancy, in approximately 40% of patients.
At the same time, if headache persists during this period, it is necessary to carry out differential diagnosis and determine the form of headache. Alarming symptoms during pregnancy are:
the appearance of a new, unusual headache;
a sharp increase in migraine attacks;
the addition of new, unusual symptoms of hypertension, including visual impairment, sensitivity, aphasia, paresis of the limbs;
the appearance of migraine aura in patients with previous migraine without aura;
increased blood pressure during hypertension;
convulsions.
The presence of active migraine during pregnancy does not affect the course of pregnancy itself and the development of the fetus, but increases the risk of preeclampsia and gestational hypertension. Moreover, the persistence of active migraine, especially migraine with aura, during pregnancy increases the risk of acute cerebrovascular accidents (ACVA) by 15–17 times [5]. The prevalence of stroke during pregnancy and the early postpartum period is 34.2 cases per 100,000 births [5].
Pain relief without drugs
So, if a woman is in good health and there are no complications during labor, then you can try to avoid painful sensations using various physiological methods: massage, water procedures, gymnastics and special breathing. All processes in the body are interconnected: if a woman is afraid, then a muscle spasm occurs, causing oxygen deficiency in the blood vessels and acute pain. Tension of the facial muscles causes a response spasm of the uterine uterus and delayed dilation of the cervix. Based on these data, when contractions occur, you need to relax and calm down, feeling that the pain is going away every minute.
Of course, it is not easy to immediately master such a technique, so during pregnancy it is necessary to attend special courses for expectant mothers, which teach the correct breathing tactics at different stages of childbirth, show basic relaxation techniques and exercises to relieve pain. Such courses can and should be attended with a partner, since many exercises are based on teamwork.
For physical exercise, you don’t need any special devices, you just need to listen to yourself and change positions more often, since physical activity makes labor easier and reduces pain. If the doctor has not prescribed bed rest, you need to walk more, preferably lying only on your side. Sitting is undesirable, as this creates pressure on the perineum.
Many women benefit from water procedures, but they can only be carried out if the water has not broken, since the risk of infection is very high. A warm bath with hydromassage is a great way to relieve tension and help you relax, but either a partner or someone from the medical staff must be present during the procedure. You can also use a shower cabin, directing streams of water to your back and lower abdomen. The water should be at a temperature of about thirty-six degrees so as not to cause bleeding. Aromatherapy, self-hypnosis and other techniques, including massage, are also quite effective in relieving severe pain. If desired, you can resort to a variety of techniques to minimize pain, but before using them, you should definitely talk with the doctor leading the birth.
Stopping attacks
The selection of drug therapy for patients with migraine during pregnancy poses significant difficulties. The severity of migraines can be especially high during the first trimester. Full-blown, unrelieved migraine attacks are often accompanied by nausea, vomiting and lead to unnecessary suffering and dehydration, especially in patients suffering from early toxicosis. Despite the desire to avoid taking medications (especially in early pregnancy) to minimize the risk of fetal developmental disorders, many patients with hypertension begin to take analgesics uncontrollably. Therefore, the importance of preliminary counseling and education of patients on the proper control of hypertension cannot be overemphasized.
Non-pregnant women are recommended to take medications to relieve migraine attacks as early as possible, no later than 1 hour after the onset of the attack. This approach allows you to speed up relief and completely stop a migraine attack in a short time. Pregnancy is the only period in a woman’s life when this recommendation can be temporarily ignored. For patients seeking to minimize drug use, a stepwise approach may be recommended, in which treatment of mild to moderate attacks begins with non-drug methods.
If the patient decides not to use analgesics, control of nausea becomes a priority to avoid dehydration. Patients should avoid strong odors and drink more fluids, such as juices diluted 1:1 with water. Feelings of nausea can also be reduced by eating easily digestible foods, such as crackers, applesauce, bananas, rice, and pasta. Metoclopramide or ondansetron can also be used [6].
Neurostimulation methods play a major role in non-drug approaches to the treatment of migraine. The only device registered in Russia for non-invasive transcutaneous stimulation of the supraorbital nerve - Cefaly (Cefaly®) - is specially designed for the treatment of migraines and can be a good alternative to medications for relieving migraine attacks. Using the Cefaly device at the very beginning of an attack allows you to reduce the intensity of headaches and in some cases completely stop the attack. Thus, the intensity of migraine pain decreases by 4.3 points after 1 hour [7]. Cefaly can also be used in conjunction with pain medications to increase their effectiveness.
Despite the fact that, in general, paracetamol is less effective for relieving an acute attack of migraine than acetylsalicylic acid and nonsteroidal anti-inflammatory drugs (NSAIDs), its safety during pregnancy is higher [6]. Caffeine, which has the ability to enhance the analgesic effect, is an important addition to painkillers. Adding 100 mg of caffeine to the analgesic increases its effect by 1.5 times.
The safety of NSAIDs is controversial [6]. Prescribing NSAIDs in the first trimester may be associated with an increased risk of miscarriage and the development of congenital anomalies. Taking NSAIDs and aspirin in the third trimester can lead to premature closure of the ductus arteriosus
. For these reasons, the use of NSAIDs should be limited to the second trimester. It is especially important to stop taking them after the 32nd week. Taking high doses of aspirin may also increase the risk of bleeding.
Triptans are the most effective analgesics for the relief of migraine attacks. The safety of triptans during pregnancy is assessed through pregnancy registries, where a huge amount of data has now been accumulated for sumatriptan, for example. Despite the prohibition of its use during pregnancy indicated in the official instructions for the use of sumatriptan, there is no evidence of an increased risk of congenital malformations when taken by pregnant women [8]. Patients who took triptans in early pregnancy (without knowing they were pregnant) should be advised that the likelihood of adverse effects of this drug on the fetus is extremely low. Women who experience severe, disabling migraine attacks that cause vomiting may be advised to use triptans during pregnancy. To date, this information has not been included in official recommendations for the treatment of migraine, but the safety of sumatriptan is confirmed by the analysis of a huge number of observations and expert recommendations.
It should be borne in mind that the safety of triptans varies. Sumatriptan, as the most hydrophilic of the triptans, has difficulty penetrating the placental barrier, while other triptans (including eletriptan) are lipophilic.
Prednisolone can only be used as an “ambulance” remedy in the event of a prolonged and severe migraine attack [9]. The use of prednisolone is preferable to dexamethasone, since the latter penetrates the placenta better. Nuchal nerve blocks with lidocaine, bipuvacaine and/or a corticosteroid can be used as an ambulance to relieve severe attacks.
What drugs are dangerous for pregnant women?
The group of non-steroidal anti-inflammatory drugs is not recommended for use during gestation. However, if your headache is very severe and other medications do not help, then you should adhere to the following rules:
- Avoid the use of analgin-based products as the most toxic of all drugs in this group.
- It is not recommended to take combined analgesics that contain several components that relieve pain. These include: “Pentalgin”, “Caffetin”, “Solpadeine”.
- It is better to give preference to medications with one active ingredient (preferably paracetamol-based).
- Try not to take two or more tablets in one day, and also avoid long-term use.
- If possible, avoid taking pills in the first trimester, when the formation of fetal organs and systems occurs.
Preventative treatment
The attending physician must promptly identify the group of patients in whom preventive treatment of migraine will be most successful. While most pregnant women begin migraine remission at the end of the first trimester, others experience migraine remission by the 10th–12th week. Frequent attacks may persist, which will most likely indicate the persistence of headache throughout pregnancy. Refusal to treat such patients can lead to malnutrition, dehydration, the development of affective disorders and a significant decrease in quality of life.
Preventive treatment of migraine is necessary in the following cases:
high frequency of attacks (more than 3 days a week);
the presence of severe or prolonged attacks;
significant disability;
dehydration and malnutrition;
poor response to analgesics.
The current frequency of headaches and the effectiveness of the analgesics used should be monitored using a headache diary. For patients who require preventive treatment, it is necessary to select the optimal combination of drug and non-drug approaches.
There are a number of non-drug methods that can effectively manage hypertension during pregnancy and are an important addition to pharmacological methods; when combined, the amount of drugs used during pregnancy and lactation is reduced. Relaxation techniques, cognitive behavioral therapy and biofeedback can be used during pregnancy.
Trigeminal neurostimulation also plays a major role in the preventive treatment of migraine during pregnancy. Regular use of Cefaly daily for 20 minutes, preferably in the evening, leads to a 2-fold reduction in migraine headache attacks in 38% of patients with episodic migraine and 35% of patients with chronic migraine [10, 11]. The high safety of this method (the probability of adverse events is 2–3%) allows it to be used without fear during pregnancy. It is also important that the Cefaly device has a mild sedative effect [12] and is not prohibited for use during pregnancy.
Information about the safety of drugs is collected through clinical trials of their use in the treatment of other diseases, including mood disorders, cardiovascular diseases and epilepsy. The safety of most drugs during pregnancy has not been directly assessed, but accumulated data have allowed these drugs to be assigned a certain safety category. In addition, the choice of drugs for the treatment of migraine in pregnancy may be based on additional information about the safety of a number of drugs that are used in pregnancy to treat hypertension, depression and epilepsy.
If it is necessary to prescribe drug therapy to reduce migraine attacks, it is recommended to start with the use of β-blockers. Due to its widespread use in the treatment of arterial hypertension during pregnancy, propranolol (anaprilin) is considered the drug of first choice for the preventive treatment of migraine [13]. At the same time, taking β-blockers is associated with a risk of hypoglycemia, hypotension, bradycardia and respiratory disorders in the newborn. The drug should also be used with caution in patients with bronchial asthma, a tendency to arterial hypotension and bradycardia. In the absence of propranolol or if there are contraindications to it, metoprolol can be used. It is recommended to gradually reduce the dose of beta-blockers during the last weeks of pregnancy (starting from the 36th week) and discontinue them at least 2-3 days before delivery.
No adverse effects on fetal development have been demonstrated with the use of calcium channel blockers, but insufficient data and the low effectiveness of verapamil do not allow it to be recommended for widespread use for the preventive treatment of migraine during pregnancy [13].
Lisinopril exhibits a teratogenic effect when used in the 2nd and 3rd trimesters and should be discontinued. Candesartan, which has a mechanism of action similar to lisinopril, should also not be used to treat migraine in pregnant women [14].
Despite the high effectiveness of antiepileptic drugs in the treatment of migraines, their use during pregnancy is prohibited. Valproic acid preparations are absolutely contraindicated during conception and pregnancy due to their teratogenic effect (disrupting the development of the fetal neural tube) and blood clotting disorders in the mother and fetus. In addition, data have accumulated on the possible teratogenic effects (development of hypospadias, cleft lip and palate) of topiramate [14].
Gabapentin has low effectiveness in the preventive treatment of migraine; the safety of its use during pregnancy has been poorly studied. Its use should be stopped in the third trimester due to its possible effect on bone development [6].
Tricyclic antidepressants are highly effective in the preventive treatment of migraine. Amitriptyline is relatively safe during this period and is the second choice drug for the preventive treatment of migraine [6, 13, 15].
The use of the serotonin and norepinephrine reuptake inhibitor venlafaxine in the third trimester increases the risk of developing behavioral syndrome of newborns by 3 times. Symptoms are usually mild in severity.
The safety of botulinum toxin type A preparations for the treatment of migraine during pregnancy has not been studied. At the same time, data have accumulated on the absence of teratogenic and embryotoxic effects of botulinum toxin type A in pregnant women who reported using the drug for various indications [16]. At the same time, the use of botulinum toxin for the preventive treatment of migraine during pregnancy is not recommended.
New drugs for the preventive treatment of migraine - antibodies to calcitonin gene-related peptide - erenumab and fremanezumab have not been studied for use in pregnant women and are not recommended for the treatment of migraine.
In addition to the above medications allowed during pregnancy, various vitamins and minerals can be mentioned. In particular, there is evidence of the benefits of magnesium for the preventive treatment of migraine during pregnancy [13, 15]. Pyridoxine (vitamin B6) at a dose of 80 mg/day alone or in combination with other drugs at a dose of 25 mg/day, for example with folic acid, can have a mild preventive effect against migraine.
Table 1 summarizes the safety data of the main groups of drugs used for the preventive treatment of migraine during pregnancy.
Non-drug methods
Given the small choice of medications for relieving headaches during pregnancy, it is worth giving preference to alternative methods.
Massage
It has been proven that running your fingers from the frontal part of the head to the back of the head (in one direction only) helps eliminate stagnation of venous blood in the sinuses of the brain. This is explained by the presence of perforating veins on the surface of the head, which are connected to the venous sinuses.
Such a massage for 15 minutes can significantly reduce pain, even eliminating it completely.
For more information on how to get rid of headaches with massage, watch the video:
Neck massage
It is especially effective if your head hurts due to osteochondrosis of the cervical spine. After all, the vertebral arteries pass through the cervical region, compression of which can cause excruciating pain in the head.
Reflexology
Impact on certain points of our body leads to the activation of certain physiological processes. So, for headaches, light pressure on the temporal areas on both sides is effective; you can use light massaging movements in a clockwise direction.
Doctor's advice
Neck massage can only be done in the form of light pressure on the muscles, stroking, and in no case too much. Firstly, movements with intense pressure will cause muscle pain. Secondly, there is always the possibility of a hernia, massage in which is done very carefully.
Victoria Druzhikina Neurologist, Therapist
Pressing on the following points will help relieve headaches: at the base of the inner edge of both eyebrows, the center of the superciliary arches (the exit point of the supraorbital nerve), the middle of the bridge of the nose, the point between the base of the 1st and 2nd fingers of both hands. You need to gently press on each point for 2-3 minutes.
Drinking strong tea with sugar
It is effective to drink a cup of strong tea for headaches associated with low blood pressure. Coffee drinks should not be consumed during pregnancy, as caffeine can cause increased heart rate. Use caution in case of diabetes mellitus and gestational diabetes mellitus, which is common among pregnant women.
Normalization of the daily routine
If a pregnant woman often has headaches, she needs to adjust her daily routine. Normalizing sleep and rest is very important. For example, walking for 15 minutes before bed is very beneficial. Pain will become much less of a problem if you pay due attention to rest.
Taking a warm shower
Promotes relaxation and improves blood circulation in the body.
You should not get carried away with aromatherapy, as some essential oils can cause an allergic reaction.
There are currently at least 50 known reasons why a headache may occur. During pregnancy, the most common are tension headaches, as well as headaches that occur when pressure rises (for example, with severe gestosis).
Despite such a wide range of drugs available on the pharmacological market, during pregnancy their choice is extremely limited. Therefore, during the period of bearing a child, before taking this or that medicine, it is necessary to find out the cause of the headache.
Unsystematic use of pills can negatively affect the baby's development. We must not forget about the serious causes of headaches (vascular aneurysm, pathological tortuosity, space-occupying brain formations). A consultation with a gynecologist and therapist will help you understand the mechanisms of pain, as well as prescribe the necessary medication.
This article has been verified by a current qualified physician, Victoria Druzhikina, and can be considered a reliable source of information for site users.
Bibliography
1. https://www.mediasphera.ru/issues/zhurnal-nevrologii-i-psikhiatrii-im-ss-korsakova/2015/11/downloads/ru/591997-729820151118 2. https://journals.eco-vector .com/RFD/article/viewFile/1431/1051
Rate how helpful this article was
3 5 people voted, average rating 3
Did you like the article? Save it to your wall so you don’t lose it!
Causes of pain and its consequences
Pain during pregnancy is usually caused by mechanical stretching of the uterus and compression of surrounding tissues with sensitive nerve fibers.
In addition, in a vertical position, the static and dynamic load on the musculoskeletal system increases. This can cause pain in the spine, as well as muscle and joint pain.
In this regard, pain, as a rule, appears in the later stages, in the third trimester, when the volume and weight of the pregnant uterus reach their maximum.
However, pain syndrome may not necessarily be associated with pregnancy. Although gestation is accompanied by changes in metabolism and hormonal changes.
All this can provoke an exacerbation of pre-existing chronic diseases of the joints, peripheral nerves, and internal organs. And an exacerbation, as you know, announces itself with pain. Changes in vascular tone and fluctuations in blood pressure (BP) often occur with a headache, which often takes on the character of a migraine.
Pain syndrome sometimes occurs for reasons independent of pregnancy. For example, toothache can affect anyone at any time. The same applies to injuries and emergency operations. Sometimes there are even dramatic situations when gestation (gestation of the fetus) coincides with the beginning of the formation of tumor formations. But this happens extremely rarely.
Basically, towards the later stages of gestation, the pain threshold increases - the woman tolerates pain more easily. Brain structures intensively produce endorphins and endorphins, the so-called. pleasure hormones responsible for positive emotions and pain tolerance. This is how nature helps a woman endure future birth traumas.
But for some expectant mothers, everything happens a little differently. Due to mental changes and metabolic disorders, hyperesthesia or increased sensitivity develops. Hyperesthesia is usually accompanied by emotional instability, irritability, and sleep disturbances. In these cases, even a small stimulus is perceived as severe pain.
Considering that analgesics are potentially dangerous to the fetus, the easiest thing would be to avoid them altogether. The problem is that even moderate but constant pain does not have the best effect on a woman’s condition. And it’s not just negative emotions and insomnia.
Pain provokes the release of catecholamines (adrenaline, norepinephrine). These substances cause vasospasm. As a result, blood supply to internal organs deteriorates. But the worst thing is that placental blood flow worsens. And this is fraught with fetal malnutrition, and, as a result, frozen pregnancy, stillbirth or miscarriage.
Classification of painkillers by release form
Hemorrhoids are a well-studied problem, so prevention and treatment methods always guarantee a good result. Despite the wide selection of drugs in pharmacies, only the attending physician can prescribe complex therapy after a thorough diagnosis of the problem. The form of release of drugs is selected depending on the individual preferences of the patient and the complexity of the symptoms. The most effective and acceptable forms of drug release are suppositories, ointments and tablets.
Candles
In an acute inflammatory process, it is extremely difficult to anesthetize a pronounced pain syndrome, because First you need to stop the swelling. Many proctologists advise the use of local anesthetics, which simultaneously relieve inflammation, relieve pain and promote the regeneration of anal fissures. The main advantages of local drugs:
- Minimum contraindications and side effects;
- Acts directly on the source of inflammation;
- Effective rate of absorption and symptom relief.
Unlike tablets, suppositories are used only for internal hemorrhoids. The neurotropic principle of action of the drug allows you to relieve pain by blocking the conduction of nerve impulses from the location of the “bumps” to the neurons of the brain.
Ointments and gels
Used for external and internal hemorrhoids. The main advantages of the drugs are ease of use, uniform distribution of the active substance and high absorption rate. The analgesic effect is achieved by relieving swelling and inflammation, narrowing the vessels of varicose veins, regenerating cracks and the antibacterial effect of the ointment. Among the names of popular products are Proctosan, Relief Advance, Proctosedyl.
Painkillers for hemorrhoids
Efficient and effective systemic drugs in the fight against the symptoms of hemorrhoids are venotonic and agnioprotective tablets. According to the principle of action, drugs can be divided into 2 types:
- Tablets that have only an analgesic effect. Their action is aimed at reducing painful symptoms. Painkillers have many contraindications, and the course of treatment cannot exceed several days.
- Systemic tablets with a dose-dependent effect can not only relieve attacks of pain, but also have a beneficial effect on the general condition of blood vessels. They affect the cause of the disease, increase venous tone, improve lymphatic drainage, increase vascular stability, thereby reducing inflammation of the nodes. Effective healing of cracks and microtraumas of the anal mucosa is achieved due to its regenerating properties. The most recommended tablets from this group are called “Phlebodia” and “Detralex”.
Before diagnosing yourself and treating the symptoms of the disease, you should consult a proctologist. Many drugs have contraindications and a special dosage regimen, without taking into account which you can harm your health and aggravate the course of the disease.
Nuances of dental treatment for pregnant women
The period of gestation in itself is not a contraindication to dental treatment. But when visiting a doctor, he must be warned about pregnancy, and also tell the due date. In this case, the following features arise during dental treatment:
- Bleaching is not allowed.
- Local anesthesia is required.
- It is possible to treat caries, pulpitis, periodontitis and gum inflammation.
- Under no circumstances should general anesthesia be used.
- Chemical and photo-curing materials can be used for filling. Polymer lamps do not harm the child.
Advice to expectant mothers - try to treat your teeth and gums before pregnancy or between the 3rd and 6th months of pregnancy, and also review your diet. If you have carious cavities, you will pass on a bouquet of microbes to your unborn child, and the destruction of your own teeth will accelerate several times.
Lyubomskaya Olesya Alekseevna, Dental surgeon-implantologist, dental therapist, dentist-orthopedist (K.M.N.) (Candidate of Medical Sciences), work experience 12 years