Secondary caries is a new pathological process that occurs in the tissues of a tooth that has previously been subjected to dental treatment. Often, it appears due to insufficient antiseptic treatment of the carious cavity or poor-quality filling, but there may be other reasons, which we will discuss below.
Dental caries under a filling is characterized by a long asymptomatic course. The first symptoms may appear 2-3 years after the filling is installed: discoloration of the enamel and increased sensitivity of the tooth. In severe cases, pulpitis can develop, which can lead to serious consequences, including tooth loss and osteomyelitis of the jaw bone.
Causes of caries under fillings
As a rule, secondary caries is the result of a whole complex of different factors. Only a dentist can name the exact cause, based on medical history and examination of the unfilled tooth - after he sees what caries looks like under the filling and determines what factors could cause it.
Of particular importance in the formation of secondary pathology is the individual susceptibility of tooth tissue to caries, the composition of the filling material, as well as compliance with oral hygiene.
The main causes of caries under fillings:
- Application of high shrinkage fillings. Over time, such fillings reduce their volume in the carious cavity, which provokes detachment of the filling material from the edges of the hard tissues of the tooth. Bacteria penetrate into the spaces unfilled with a filling, provoking a new stage of caries development. Sometimes, caries damage can be seen with the naked eye along the edges of the filling, especially on the front teeth;
- Poor-quality cleaning of a carious cavity is a direct mistake by the doctor when filling: the affected tissue remains inside, in which bacteria are concentrated, continuing tooth destruction;
- Poor processing of the filling - rough grinding and polishing contribute to increased adhesion, which leads to accelerated plaque formation on the surface of hard tooth tissues, as well as the formation of chips of the filling material and microcracks.
Caries is a systemic disease that can occur not only due to the above reasons, but also due to general factors. For example, in regions of Russia with low fluoride content in the soil, more than 97% of the population (all age groups) suffer from primary and secondary caries. Also, the development of caries under a filling can be triggered by the patient’s refusal of immunomodulatory therapy during the treatment of concomitant diseases.
What determines the result of filling?
A tooth after filling can be destroyed by secondary caries for several reasons.
- When consuming cold and hot food and drinks at the same time (for example, cold ice cream and hot coffee or hot kebab and cold beer). In such cases, under the influence of a significant temperature difference, microcracks form in the tooth enamel and in the places of contact of dental tissues with the filling material.
- The seal may shift slightly when chewing on too hard, tough foods. This will be enough for a microcrack to appear.
- Malocclusion and pathology such as bruxism are accompanied by excessive friction of teeth against each other and cause accelerated abrasion of the filling composition and dental tissues.
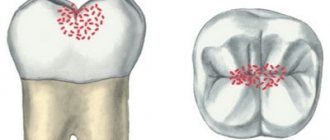
- An insufficient level of hygiene leads to the settling of food particles and the formation of a significant amount of soft plaque in the fissures (tubercles on the chewing surface of the teeth) and in the interdental spaces. This accelerates the development of a bacterial infection.
Key differences between secondary caries and recurrent caries
Unlike secondary caries, recurrent caries occurs only at the site of treatment already performed. If lesions appear on the same tooth, but nearby, this is repeated caries. It is almost impossible to find out the cause of the development of recurrent or repeated caries. Only a doctor, based on examination data, can suggest why caries appeared under the fillings.
When diagnosing secondary and recurrent caries, the doctor must remember that both types can develop in combination due to a combination of various factors.
Lifestyle
If you have learned about the risk group for root caries (older age), this does not mean that you can relax. Caries has many causes and can occur at any age if basic precautions are not followed.
Those at risk include smokers, diabetics, pregnant women and even children. The provoking factors in this case are:
- smoking and lack of oral hygiene;
- infrequent brushing of teeth and lack of fluoride;
- poor nutrition with preference for desserts;
- frequent stress;
- alternating hot and cold;
- structural features of the oral cavity;
- alcohol abuse - alcohol breaks down into sugars and acids;
- abuse of coffee and strong tea, which creates an acidic environment in the oral cavity;
- lack of water intake, and therefore lack of saliva;
- gum injuries.
Symptoms of caries under a filling
In the vast majority of cases, secondary caries is asymptomatic. The first signs, with rapid development, may appear only 3-6 months after the filling is installed. If symptoms appear 2-4 weeks after filling, this is recurrent caries. It occurs due to improper treatment and can pose a serious threat to the tooth. To eliminate it, it is necessary to replace the old filling with repeated cleaning and disinfection of the carious cavity.
Classic symptoms of caries under a filling include:
- Darkening of the enamel near the edge of the installed filling - pigmentation can be located either at one edge or along the entire rim of the filling;
- The causative tooth acquires a gray tint, through the enamel you can see what caries looks like under the filling - it will have a dark tint;
- Chips of the filling and tooth enamel appear, microcracks form (not always);
- The mobility of the filling increases. With prolonged development of caries, it may fall out;
- There is an unpleasant odor from the mouth, caused by the proliferation of bacteria in the formed microcracks;
- Increased sensitivity of teeth to cold, hot, sour and sweet;
- Aching pain appears, which intensifies during the process of biting;
- Acute tooth damage by secondary caries develops, accompanied by pain, swelling and bleeding.
Causes of the disease
There are 3 main provoking factors that must act in a complex manner; none of them acts independently:
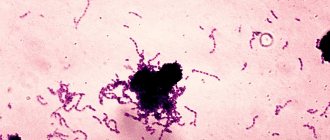
- Cariesogenic microflora - this includes Mutans streptococci, actinomycetes and certain types of lactobacilli. They should dominate the oral cavity. Bacteria produce organic acids from food carbohydrates, which cause demineralization of cement.
- Consumption of simple carbohydrates is the most cariogenic. Their breakdown produces glucan, which contributes to the appearance of plaque.
- Reduced caries resistance is a deterioration in the resistance of tooth tissue and the body as a whole. This is facilitated by a decrease in calcium content in hard root tissues, bad habits, and lack of saliva.
In addition, the anatomical features of the mouth can also have an effect - a small vestibule, a short frenulum, and bite pathology.
Gum disease, pocket formation
Gum pocket or otherwise periodontitis is a common occurrence in many patients. Many people do not treat it because it does not bother anyone for a long time.
The first manifestation of pathology is bleeding when brushing teeth, although outwardly they may look healthy. Dental pockets or depressions are normal, but their anatomical size should not exceed 3 mm.
Then the pocket is able to self-clean from food debris and epithelial particles. Reservoirs of bacterial accumulations form in deep gaps. This is accompanied by bad breath. Conventional treatment with antibiotics and brushing teeth with toothpaste have no effect.
Causes of periodontitis:
- insufficient hygiene;
- poor quality fillings;
- abnormal position of the dentition, malocclusion;
- hereditary predisposition;
- deficiency of vitamins and minerals;
- immunosuppression.
Consequences of secondary caries
The lack of timely diagnosis and proper treatment leads to the development of complications in the form of acute or chronic tooth pulpitis with aching pain and all the ensuing consequences. At this stage, replacing the old filling with a new one, while simultaneously cleaning the carious cavity, will not help - preliminary treatment of pulpitis is necessary.
Delaying the treatment of pulpitis under a filling leads to partial or complete destruction of the hard tissues of the tooth. It is accompanied by the development of infection affecting the periodontal tissues with subsequent progression to periodontitis. In particularly severe cases, periodontitis affects the jaw bone - this can result in osteomyelitis of the jaw bone.
Types of ceramic inlays
- inlay tab - restores the “cavities” of the tooth crown
- onlay tab - restores most of the chewing surface of the tooth crown
- overlay tab - restores the chewing surface and side walls of the tooth crown
The service life of the inlays is more than 10 years, while the filling will require replacement after an average of 5 years.
Now, when a dentist suggests restoring a tooth with an inlay, you know what benefits this will provide in the future.
Methods for diagnosing and treating caries under fillings
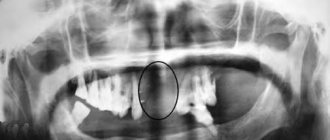
It is quite difficult to determine the presence of secondary caries in the initial stages, due to the absence of symptomatic and visual manifestations. The disease is diagnosed during a follow-up appointment using diagnostic equipment (hardware diagnostics).
Diagnostics includes two stages:
- Anamnesis and initial examination of the causative tooth in order to detect visible structural changes in hard tissues;
- Hardware diagnostics (physiography) is aimed at detecting hidden changes in the structure of dental tissues.
If a pathology is detected, treatment is prescribed taking into account the individual characteristics of the patient.
What to do to protect your gums
If the gum is not treated, inflammation will remain and all treatment will become meaningless. The gums are protected by diathermocoagulation and retraction.
Diathermocoagulation
Diathermocoagulation – excision of excess areas of periodontitis with a coagulation knife. The knife immediately cauterizes the bleeding edges. The procedure is performed when there are severe changes in the gums. In such cases, filling is postponed until the soft tissue is completely regenerated.
Retraction
If the condition of the gums is advanced, treatment of caries becomes impossible - the mucous membrane bleeds and interferes with tooth treatment. This gum is excised or a special device is applied to move the gum back. But more often, retraction is performed - lowering the gingival contour or moving apart the overhanging edges of the gums using special hemostatic threads. A temporary filling is placed until complete healing.
Features of treatment of secondary caries
The use of one or another treatment regimen for secondary caries directly depends on the location of the lesion, its depth and the condition of the causative tooth. Treatment may include two options for developing the situation:
- Re-filling or replacing part of the filling in the affected area is performed only after treating the tooth and eliminating the carious lesion. In some cases, it may be necessary to remove the nerve and fill the canals.
- Surgical tooth extraction is used in extreme cases when the damage is too large and the doctor cannot save the affected tooth.
What is the danger of this disease?
Caries is dangerous because there are no symptoms for a number of years. It is detected more often in an advanced stage, when tooth extraction becomes the solution.
Visual diagnosis is difficult because all destructive processes occur inside the tooth. Pronounced plaque or tartar hides any stains on the enamel.
The root is hidden under the gum and external irritants do not affect it until a certain time. On the other hand, the root walls are thin, so they are destroyed quickly and with complications.
Methods for preventing caries under a filling
High-quality prevention of secondary caries involves the elimination of complications at the stage of initial installation of a filling - the doctor must ensure the correct method of caries treatment, antiseptic treatment of the hole for the filling and installation of the filling.
On the patient’s side, the most effective prevention of secondary caries under a filling is maintaining proper oral hygiene, as well as systematic examinations in a dental clinic: a month after the filling is installed and at least 2 times a year thereafter.
Cleaning in dentistry from stone and plaque
1243900247100
Professional teeth cleaning involves removing the accumulation of all pathogenic microflora around the root.
It involves not only removing plaque, but also stones. This elimination of negative factors protects teeth for a long time.
Antiseptic treatment of affected areas
Treatment of root caries involves drilling out all affected areas with a drill and treating the carious cavity with antiseptics and special preparations. A 2% chlorhexidine solution or a gel based on it is used as an antiseptic for the treatment of carious cavities.
Description of the pathological process
The development of secondary (recurrent) caries is said to occur when the pathological process begins to develop under a recently fixed filling, inlay or crown. That is, after any treatment. As a result, the tooth gradually changes its color, and the most common reason for this is poor quality treatment. A relapse of the disease occurs, which in the vast majority of cases is the result of leaving a gap between the dental tissues and the filling material. Or poor quality cleaning of the cavity from inflamed tissues.
Secondary caries - how does it manifest?
Currently, high-quality modern materials are used in dentistry, but even they are characterized by limited strength indicators, which primarily concerns chewing teeth. Gradually, the material wears out, breaks down and falls out. Another common reason for the development of secondary caries is the abrasion of the filling - over time it decreases, exposing the walls of the carious cavity and provoking the re-development of inflammatory processes.
Continued action of the etiological factor that caused tooth decay
In case of caries, a filling not only restores lost tissue, but also prevents its further progression (if placed correctly). With a wedge-shaped defect, this does not always happen. Nevertheless, often a filling is the optimal way to solve the problem for some time with this disease. This is exactly the case when the dentist may not be at fault, and such a nuisance should be taken calmly. For more details, see Treatment of wedge-shaped defect.
Is it always possible to replace an old filling with a new one?
Depending on the degree of tooth decay and aesthetic requirements, restoration can be done:
1. Filling made of composite material. As a rule, if the tooth decay is less than 50%
2. Veneer or componir in case of restoration of the anterior group of teeth - Veneer - the thinnest porcelain plate made in a dental laboratory using an individual impression - Componir - a budget analogue of a veneer, made in a factory from composite materials
3. Inlay made of composite material or ceramics. In case the tooth is destroyed by more than 50%. An inlay is a “large” filling that is made in a dental laboratory. It is much stronger than a filling and better conveys the anatomical features of the teeth and matches the color
4. A crown made of metal ceramics or zirconium dioxide. A crown is installed in case of significant tooth decay
If the crown part of a tooth is completely destroyed, then a crown will be the best solution to preserve it, since under heavy chewing load the wall of a tooth covered with a filling may break off, and if the crack goes under the gum, then the tooth will have to be parted with.
Symptoms and signs
Recognizing signs of tooth decay by caries is not so easy; a filling and the inconvenience of self-examination do not allow one to detect darkening of the enamel or the beginning destruction of bone tissue. However, there are symptoms by which you can recognize the presence of the disease:
- pain on individual teeth and the lower part of the jaw;
- inflammation of the gums in the area of the filled tooth, swelling;
- an unpleasant odor emanates from the mouth (if the tooth is rotting under a filling);
- the appearance of blood on the gums when brushing the mouth or as a result of a minor collision with blunt objects.
Bleeding from the gums of the affected tooth and aching in the jaw area are often observed. Carious lesions of bone tissue can also be detected visually. It is worth paying attention to the seal. Often it changes color or a dark brown rim appears along its edges. The formation of cracks and chips of tooth enamel is also observed.