Symptoms
In patients with a violation of the continuity of the series, certain groups of masticatory organs are overloaded, chewing function is impaired, as well as diction, and the temporomandibular joint unit does not function properly. If there is no therapy, secondary malocclusion develops, in which the masticatory muscles are seriously affected. If the absence of frontal units negatively affects the appearance, then the terminal defect of the dentition leads to disturbances in the functioning of the gastrointestinal tract. The following groups of units are gradually formed:
- Chewing organs with preserved functions;
- Incisors, canines, premolars, molars with lost ability to act;
An uneven load causes displacement of the arch as a whole or the incisors, and deformation of the occlusal zones also occurs. Sometimes apraxia of speech is diagnosed, and incomplete atrophy of bone tissue is possible. Subsequently, areas with high loads shift more strongly from the normal axis. With the loss of units, the interalveolar distance often decreases, and the lower part of the face is shortened, wrinkles appear, soft tissues sink, and folds form on the skin. Aesthetic defects and incorrect speech lead to the patient’s reluctance to communicate with others.
Classification of defects of the lower jaw
The classification of defects is influenced by the clinical characteristics of the lower jaw, how many fragments of the lower jaw there are, the presence or absence of teeth in the areas, the location of the defects, etc.
Defects are classified according to their size:
- small (up to 2 cm);
- medium size (2-6 cm);
- subtotal (up to 10-12 cm);
- up to half the length of the jaw;
- total, can be with preservation of continuity of the bone tissue of the lower jaw (cavitary, perforated, cystic and marginal).
Based on the condition of the adjacent soft tissues, defects of the lower jaw can be divided into two types:
- defects without damage to soft tissues;
- defects with loss of soft perimandibular tissue (most often occur during removal of a tumor of various etiologies or as a result of a gunshot wound).
All these defects can be located in different places of the jaw.
Diagnostics
To successfully treat patients, a thorough examination must be performed. When initial signs appear, patients should consult a dentist. He will examine the oral cavity, assess the condition of the gums and chewing organs. If necessary, the patient will be referred for additional studies. According to indications, instrumental diagnostics are prescribed. If consultation with an endocrinologist, therapist, or gastroenterologist is needed, the patient is referred to these specialists. Consulting an orthodontist is important for drawing up a correction and prosthetic plan.
As a rule, the pathology has a specific severity, so it is diagnosed during a visual initial examination. Establishing provoking factors most often requires additional diagnostic procedures. In order to make a final diagnosis, as well as determine therapeutic methods, doctors may refer the patient for radiography. It will allow you to obtain complete information and create the correct treatment plan.
Prosthetics of dentition defects with removable dentures
Content
1.Introduction…………………………………………………………………………………3
2. Classification of partially missing teeth………………………………..4
3. Indications for the use of removable denture structures in case of partial absence of teeth………………………………………………………………..5
3.1. Contraindications to the use of removable denture structures with partial absence of teeth………………………………………………………6
4. Justification of the boundaries of a removable denture………………………………………………………7
5. Methods of fixing removable dentures………………………………………………………11
6. Conclusion………………………………………………………………………………27
7. References……..…………………………………………………….26
Introduction
One of the pressing problems of orthopedic dentistry is the prosthetics of dentition defects with removable dentures. Patients with partial loss of teeth over 50 years of age make up the largest group of people in need of this type of orthopedic treatment - 40.2%. At the same time, in younger people, removable dentures are also used quite often - from 15 to 20%. This is due, first of all, to the early loss of part of the front teeth as a result of trauma, destroyed by caries, periodontal diseases, etc., when, in order to preserve healthy teeth bordering on a defect, preference is given to a removable denture, which allows achieving the maximum level of aesthetics.
1. Classification of partially missing teeth.
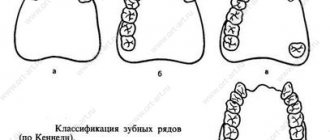
In clinical practice, partial absence of teeth in the upper jaw and lower jaw is not distinguished. The classification principles are the same for both jaws. Kennedy's classification of partial secondary adentia (dentition defects) is most widespread and practically used:
- Bilateral distally unlimited defect (end defect);
- Unilateral distally unlimited defect (end defect);
- Unilateral distally limited defect (included defect);X
- Absence of front teeth (defect in the anterior region) (included defect).
Another well-known classification of dentition defects is the classification of E.I. Gavrilova. It identifies four groups of defects:
- End one-sided and two-sided;
- Included (lateral - one-sided, two-sided and front);
- Combined;
- Jaws with single teeth preserved.
Close to this classification is the Wilde classification of defects, which distinguishes the following main categories (classes) of partial secondary edentia:
- Unilateral or bilateral terminal defect of the dentition;
- One or more included defects;
- A combination of terminal (terminal) and included (included) defects of the dentition.
2. Indications for the use of removable denture structures in case of partial absence of teeth.
1. Defects in the dentition that cannot be restored with bridges in order to normalize chewing function.
2. Removal of a large number of teeth (direct denture).
3. Violation of the occlusal relationships of the dentition (the prosthesis serves as a bite plate - orthodontic treatment).
4. The need for extensive traumatic treatment of teeth for proposed bridges.
5. The need for horizontal unloading (splinting prosthesis).
6. The need for extensive traumatic treatment of teeth for proposed bridges.
7. Absence of even one tooth (aesthetic prosthesis).
8. Severe condition of patients in need of prostheses.
9. Refusal of the patient to undergo prosthetics with fixed structures.
10. Replacement of an old, functionally ineffective prosthesis with a new one.
11. Galvanosis, allergic reaction to metal prostheses.
2.1. Contraindications to the use of removable dentures in the case of partial absence of teeth.
1. In case of an allergic reaction to plastic and its components.
2. For diseases of the oral mucosa, if they cannot be cured therapeutically.
3. Patients with schizophrenia, epilepsy, alcoholics, people whose work activity is related to a certain profession (lecturer, announcer, singer, military man, etc.).
3. Justification of the boundaries of the removable denture.
Planning the boundaries of a removable laminar denture in case of partial loss of teeth is carried out
- taking into account the severity of the alveolar ridges,
- conditions of the mucous membrane,
- topography of dentition defects,
- number of missing teeth
- the state of the supporting tissues of the remaining teeth and antagonist teeth,
- as well as design features of the future prosthesis.
On the upper jaw, the border of the base passes in the area of missing teeth on the buccal and labial sides; the border runs along a transitional fold within the passively movable tissues, bending around the movable frenulum and cords of the mucous membrane of the vestibule of the mouth. On the palatal side, the base is adjacent to the necks of the teeth, covering 1/3 of the height of the crown (including palatal tubercles) of the anterior teeth and 2/3 of the lateral teeth. On the hard palate, the border of the prosthesis base runs along the posterior edges of the tubercles, which ensures the stability of the prosthesis, and reaches line A (goes through the blind fossae located between the hard and soft palate). If there is a torus, it is covered with a base, having previously insulated the jaw on a plaster model with tin or other foil. In such cases, a recess is formed on the palatal surface of the denture base. If there are large numbers of remaining teeth, it is possible to bypass the torus without covering it with a denture base. Reducing the size of the denture base is permissible in the presence of anterior teeth, when the anterior part of the hard palate can be freed. In the absence of front teeth and the presence of lateral teeth, the base can be reduced due to its distally located part. The boundaries of the prosthesis in the anterior section of the edentulous alveolar process of the upper jaw vary somewhat depending on the severity of the alveolar ridge and the length of the upper lip. With a short upper lip, part of the alveolar process is exposed when smiling. If it is covered with artificial gum, a serious aesthetic disadvantage arises. Therefore, with a short lip and a well-developed alveolar process, the front teeth are placed on the groove. With a long lip and large atrophy of the alveolar process, the front teeth are placed on an artificial gum. In this case, when you smile, the gum will be covered by the lip. It is impossible to place teeth on a groove if there is severe atrophy of the alveolar process. In this case, in order to avoid exposing the gums when smiling, it is necessary to use long teeth, which does not always correspond to the shape of the patient’s face. From the palatal surface, in the area of the preserved anterior teeth, the border of the denture base depends on the depth of the incisal overlap. However, it should not disrupt the incisal-tubercle contact.
On the lower jaw on the lingual side, the borders of the prosthesis run along the transitional fold, bending around the frenulum of the tongue. Moreover, unlike the upper jaw, the prosthesis base covers all remaining teeth to 2/3 of the height of the crowns. This eliminates the possibility of subsidence of the prosthesis and prevents injury to the mucous membrane. In case of terminal defects, the base of the prosthesis covers the tubercles of the lower jaw completely, if they are dense; by half - if they are movable, and thereby increase the boundaries and reduce the pressure on the underlying tissues. On the lingual side of the alveolar part in the area of the premolars there are bony protrusions (exostoses). They are isolated on the plaster model with tin foil, like a hummock on the roof of the mouth. In this case, the border of the base must necessarily pass below the bony protrusions and completely cover the exostoses. The edges of the prosthesis must be rounded and at least 2 mm thick. Thinned edges, gradually merging with the surface of the mucous membrane, are created on the palate and in the distal part of the lower denture on the lingual side.
Changes in the boundaries of the base will depend on the size of the dentition defect, the degree of atrophy of the alveolar ridge and the state of the supporting apparatus of the teeth of the opposite jaw. If the unilateral defect is terminal (Kennedy class II), then the base is placed on both sides of the jaw. In this case, on the side of the defect the base completely covers the prosthetic bed, and on the opposite side it reaches the level of the first molar. For bilateral terminal defects of the dentition (Kennedy class I), the prosthesis base is placed along the entire length of the prosthetic bed. In some cases, taking into account the individual characteristics of the development and condition of the tissues of the oral cavity, the border of the base can be shortened in the area of natural front teeth. In order to prevent injury to the gums in the area of the necks of the teeth, it is freed from contact with the base of the prosthesis. To achieve the greatest effectiveness of orthopedic treatment for partial loss of teeth, it is necessary to select artificial teeth that are similar in shape, color and size to the preserved natural teeth, to increase the support area of the prosthesis outside the prosthetic bed to prevent the prosthesis from falling off, and to use stabilizing elements that are hardly noticeable to others. The relief of the occlusal surface of the artificial teeth of a removable denture should imitate the morphology of this area and not reduce the volume of the oral cavity. The shape of the artificial gum is modeled similarly to the natural one, and the plastic is selected according to the color of the gum. Rational planning of the design of removable dentures for terminal defects of the dentition is associated with certain difficulties, since often in the oral cavity there are conditions for displacement of dentures in almost all directions. Options for combining terminal defects of the upper and lower jaws are varied. Orthopedic treatment for end defects is primarily aimed at restoring impaired chewing function, then at preventing tooth movement and reducing the height of the lower part of the face. Failure to comply with the above requirements in some cases leads to the fact that due to the lack of functional usefulness of prostheses, patients refuse to use them.
4.Methods of fixing removable dentures.
Anatomical retention. Anatomical retention is created by natural anatomical formations on the upper and lower jaws, whose shape and position can limit the freedom of movement of the prosthesis during conversation or eating. Thus, well-preserved alveolar ridges of the upper and lower jaws and a high arch of the hard palate prevent horizontal movements of the prosthesis, which weaken the adhesion force. The alveolar tubercles of the upper jaw prevent the prosthesis from sliding forward. In this regard, they act in collaboration with the anterior part of the palatine vault. The best conditions for fixing the prosthesis are when the vault of the hard palate is moderately pronounced, allowing both adhesion forces to manifest themselves and the action of resistance nodes that limit the lateral and anterior shifts of the prosthesis.
The use of adhesion (adhesion) and anatomical features of the prosthetic bed does not solve the entire problem of fixation, if only because with a small prosthesis base, the adhesion forces are negligible, and the anatomical conditions may be unfavorable. However, the latter are a great help in the prosthesis fastening system and cannot be ignored. Mechanical devices (fixators) play a decisive role in fixing removable dentures. Fixators are divided into direct and indirect. Direct retainers are located on the tooth and prevent vertical movement of the prosthesis. These include clasps, all attachment systems (lock connections). Based on their location, fixators are divided into intracoronal (intracoronary) and extracoronal (extracoronary). The first includes some types of attachments, the second - clasps.
Indirect clamps prevent rotation (tipping) of the prosthesis. Their role can be played by continuous clasps, extensions, overlays, etc.
Fixing a partial removable denture may seem like a purely technical task if it is considered only from the point of view of fastening the prosthesis and those devices and materials that are used for this purpose.
Currently, orthopedists have various clasp designs that allow them to strengthen the prosthesis in the oral cavity, even in difficult conditions, using natural teeth as support. The clasp (hook) was first used by Mouton (1764). The problem is to use a system of clasps that, while fixing the prosthesis, would not have a harmful effect on the supporting teeth, allowing the residual dentition to be preserved for a long time. At the same time, the issue of preventing rapid atrophy of the alveolar process must be resolved by correctly distributing the forces falling on the prosthesis between the supporting teeth and the tissues of the prosthetic bed. From this point of view, fixation of a removable partial denture appears as a complex biomechanical problem.
Most clasps have both advantages and disadvantages. Knowing where, when and in what order certain clasps are located is an art. It is comprehended by studying the clinical characteristics of the tissues and organs of the oral cavity, as well as the mechanical properties of the clasps themselves and the method of their interaction. Therefore, there are many different designs of clasps (Fig. 357), used according to the corresponding indications.
Before talking about the purpose of the clasp, it is necessary to decipher such concepts as supporting, stabilizing and fixing functions. The first function is understood as the transmission of chewing pressure through the supporting elements of the clasp to the teeth, preventing subsidence of the prosthesis and overloading the tissues of the prosthetic bed. By the second, we mean the prevention of lateral shifts and, finally, by the holding (fixing) function we mean the prevention of the prosthesis slipping from the prosthetic bed.
The most advanced types of clasps perform all three functions simultaneously, for example, a dispute-retaining clasp (three-arm, combined). For other clasps, one or another function predominates, for example, retention. This type of clasp is a regular wire retaining clasp.
Retaining clasps. In the design of any retaining metal clasp, there are three main elements, namely the shoulder, the body and the process (Fig. 357, 358).
In partial lamellar plastic dentures, round bent wire retaining clasps are most widely used (Fig. 357, 358).
The shoulder of the clasp is its springy part, covering the crown of the tooth and located directly in the area between the equator and the neck. It should fit tightly throughout the entire surface of the abutment tooth, repeat its configuration and have high elastic properties. Adhesion at only one point leads to a sharp increase in specific pressure during movement of the prosthesis and causes enamel necrosis. The death of the enamel of the supporting tooth is most often a consequence of uneven distribution of pressure due to poor fit of the clasp.
Clasps must be passive, that is, they must not exert pressure on the tooth being covered when they are not under tension. Otherwise, a constant unusual stimulus arises, which may be the cause of primary traumatic occlusion. The active pressure of the clasp is, in addition, the cause of enamel necrosis if the tooth is not covered with a metal crown. Therefore, it is important that the clasps are made from a material that has good elastic deformation and can acquire this quality with appropriate heat treatment. They are made from wire (stainless steel or gold-platinum alloy) of various diameters: 0.4-1.0 mm. The larger the diameter of the wire clasp, the higher its holding force.
The properties of the clasp arm depend on its length, diameter, cross-sectional shape, and material. The longer the shoulder, the more elastic it is.
The material and method of manufacturing the clasp also matters for its elasticity. Plastic clasps are less elastic, then in order of increasing elastic properties come cast gold, cast steel or chromium-cobalt alloys, but wire clasps have the greatest elasticity.
Clasp body. The body of the clasp is the part connecting the shoulder and the process, located above the equator of the abutment tooth, on its contact surface on the side of the defect. It should not be placed near the neck of the tooth. In this case, the clasp will prevent the application of the prosthesis.
It is necessary that the place of bending at the transition of the shoulder into the body of the clasp is 0.5 mm away from the surface of the tooth, which allows the doctor to grind off the plastic while fitting the prosthesis. Otherwise, contact of the clasp metal with the tooth surface will make it difficult to apply the prosthesis and eliminate the possibility of correction. The body of the clasp passes into a process that goes into the plastic base or is soldered to the metal frame of the prosthesis.
The extension is intended for attaching the clasp to the prosthesis. It lies along the toothless alveolar ridge, 1-1.5 mm away from it, under the artificial teeth. It is not recommended to place the process on the palatal or lingual side of the base, as this will contribute to fracture of the prosthesis. For better fastening in the base plastic, the end of the extension of round wire clasps is flattened, and for flat ones it is bifurcated, notches are created or a mesh is soldered.
The described parts are a mandatory accessory of any retaining clasp. These clasps, as the name suggests, are designed to hold the denture on natural teeth. When the prosthesis moves, the clasp slides along its surface, so the pressure from the prosthesis is transmitted mainly to the mucous membrane, and through it to the bone. The concentration of chewing pressure on a small area of the alveolar process enhances the phenomena of atrophy in it. Only with lateral shifts of the prosthesis do the retaining clasps take part in the distribution of the chewing load, transferring it to the tooth, and through it to the periodontium, in a less favorable (transversal) direction for it. In this case, two zones of tension and two zones of compression arise in the periodontium.
For fixation of the prosthesis, the number of supporting teeth and their location are of great importance.
Clasp line. The line connecting the supporting teeth on which the clasps are located is called the clasp line. Its direction depends on the position of the supporting teeth. If the supporting teeth are located on one side of the jaw, then the clasp line has a sagittal direction, and if the supporting teeth are located on opposite sides of the jaw, it is transversal or diagonal (Fig. 359).
When using one tooth as a support, the fastening of the prosthesis is called point, two teeth - linear, three or more teeth - planar.
The least advantageous type of fastening is point fastening, when all the shocks perceived by the prosthesis during functional load are transmitted to the periodontium of one tooth, leading to its overload.
The harmful effect of clasps on the periodontium of supporting teeth can be significantly reduced by using anatomical retention points (alveolar processes or parts, maxillary buffs, palatal vault, internal oblique lines) to fix the prosthesis.
From a static point of view, linear fastening is more expedient than point fastening. Only in the absence of a choice is it necessary to create a sagittal clasp line, which is disadvantageous from the point of view of the stability of the supporting teeth and the prosthesis itself. For example, in the upper jaw there are two teeth left on one side - the first molar and the first premolar. The clasp line in this case will be sagittal. In other words, when constructing a clasp line, it is necessary to strive to ensure that parts of the prosthesis are on both sides of it, that is, the clasp line should be an imaginary axis of rotation of the prosthesis (on the lower jaw - transversal, on the upper jaw - diagonal). However, even the most appropriate linear reinforcement has very significant drawbacks with regard to the impact on tooth stability. With chewing pressure, the denture moves lever-like in different directions. The force of this movement is measured by the length of the lever arm. The shoulder is equal to the perpendicular restored from the middle of the clasp line, that is, the line connecting the middle of the supporting teeth. The larger the lever arm, that is, the greater the force of chewing pressure, the greater the tipping effect on the supporting teeth.
Fig. 359. Types of direction of clasp lines: a-a and b-b - sagittal, b-c and c-c transversal, e-f - diagonal.
A clasp system can be considered satisfactory if it meets the following requirements:
- Provides fixation to the same extent on all supporting teeth;
- Eliminates tipping or rotation of the prosthesis;
- Does not increase the height of the bite (interalveolar) on occlusal pads;
- Minimally violates aesthetic standards.
- The clasp system should not create a traumatic occlusion. To prevent this, one shoulder must fix the prosthesis, and the other must counteract it, that is, prevent it from shifting in one direction or another (reciprocal “action”).
Types of clasps. Clasps are divided according to various criteria:
- by manufacturing method (bent, cast);
- according to the shape of the profile section (round, semicircular and strip);
- according to the degree of tooth coverage and their number (single-arm, double-arm, flip-over, double, multi-link);
- by function (holding, supporting and controversial-holding);
- according to the method of connection to the prosthesis base (rigid, semi-rigid or springy, hinged).
Wire loop clasp. The wire loop clasp arose as a result of the improvement of the single-arm wire clasp. The material for it is stainless steel wire with a diameter of 0.6-0.8 mm. The arm of the clasp is bent in the form of a loop so that one thread of the loop passes above the equator, and the other below it, parallel to the first. To hold the clasp in plastic, a mesh can be soldered onto its extension. The loop clasp cannot be used on incisors. On the upper incisors this is unfavorable for aesthetic reasons, and on the lower incisors due to the small area of the labial surface. Loop clasp is contraindicated for low clinically* crowns. In addition to the single-arm loop-shaped clasp, there is also a double-arm clasp (Fig. 357.3).
Approximal single-arm clasp. An approximate single-arm clasp is a type of retaining clasp and is used only on the front teeth. A more advanced design is the double-armed approximal clasp (Fig. 357.5). A variation of this clasp is a reversible clasp, often called a Jacksonian clasp. This also includes ring-shaped clasps.
Single-arm tape clasp. The single-arm tape clasp (Fig. 357.6) is made from stainless steel sheet 0.5 mm thick. The shoulder of the tape clasp is bent with special contour pliers, which allow it to be given the desired shape. Currently, this clasp is practically not used, since food debris accumulates under it and it is difficult to accurately fit it to the surface of the tooth.
Double-arm wire clasp. This clasp has two arms (Fig. 357.2), the first is located on the vestibular surface, the second - on the lingual or palatal surface, counteracting the first. The double-arm clasp is used in two common forms. In the first form, both arms of the clasp have a common body and process; in the second form, the arms of the clasp and the body are isolated from each other and only their processes are united by a common loop. Such a clasp could be called split.
If the clasp arm is extended through the interdental space by placing it on the buccal surface of the adjacent tooth, you will get a so-called extended clasp (Fig. 386). It is a mistake to think that lengthening the clasp improves its fixing properties. Only one extreme shoulder remains elastic in these clasps. The other links are essentially the body of the clasp. An elongated or two-link clasp is indicated for low stability of the outermost abutment tooth.
A continuous clasp (multi-link) is a type of extended clasp, but differs from it in that it forms a closed system (Fig. 357, 15). This clasp can be located on both the vestibular and lingual-palatal surfaces of the dentition. It can be bent from wire, but the best result is obtained by casting continuous multi-link clasps. Continuous clasp serves various purposes. It can be used as a retaining, splinting element and as a supported clasp.
Dento-alveolar clasps. The extensions of the denture base on the vestibular side, directed towards natural teeth, are called dento-alveolar clasps (Fig. 357). Possessing a certain amount of elasticity, they freely pass through the equator of the tooth and are installed under it. In this way, these clasps provide fixation of the prosthesis.
Plastic clasps are sometimes made reinforced, that is, containing metal wire inside. This is believed to make them more durable. This is unlikely to be correct. It is believed that the introduction of wire into the thickness of the plastic weakens its mechanical properties due to the difference in the coefficients of volumetric expansion.
For better fixation, the prosthesis is equipped with several clasps. But this causes certain inconveniences. So, on the upper jaw they protrude the lip forward and are visible when smiling. This drawback can be somewhat mitigated by making the clasp from white plastic.
Dento-alveolar clasps are used for high crowns of supporting teeth, and in cases where the teeth limiting the defect are parallel to each other. For low clinical crowns, the use of dento-alveolar clasps is contraindicated. They are also contraindicated in cases of overhanging alveolar process, since the latter complicates the insertion of the prosthesis. Plastic clasps have another drawback: they cannot be activated. This type of clasp was developed by the Hungarian dentist Kemeny.
The gingival clasp is a process of the base, located almost at the very transitional fold (Fig. 357.7). Its fixing properties are small, since the plastic from which it is made has low elasticity. A gingival clasp should be used only in cases where other methods of fixation are unacceptable and when the abutment teeth for some reason cannot be used to fasten the graft. They are indicated for fixing the prosthesis in the area of the front teeth for aesthetic reasons and for periodontal disease.
Most often, cheap clasps are used in complete dentures, when the front teeth are in the groove, as well as in cases of significant bone protrusions, which for some reason cannot be smoothed out. This class includes a clasp with pelotes, that is, the gingival clasp is connected to the base with a wire rod, but activation of the latter can cause bedsores on the mucous membrane (Fig. 361.6).
Support-retaining clasp is the most effective mass design, widely used at present. More information about these clasps is given in the description of clasp dentures.
Fixation of prostheses using locking fasteners.
Locking fasteners (attachments) are mechanical devices consisting of two main parts - a patrix (internal) and a matrix (external), the connection of which ensures the fixation of a removable denture on the supporting teeth. In most cases, one part of the locking fastening is located in the removable part of the prosthesis, the other is fixed on an artificial crown covering the supporting tooth. The connection of the two parts of the attachment occurs either in an artificial crown or inside the base of a removable denture, which allows you to obtain a highly aesthetic result. Modern locking fasteners consist of the same main parts as support-retaining clasps: occlusal stop, stabilizing part, retention part. If the design of the attachment includes all three parts (supporting, stabilizing and retaining), then such a locking mount will be a more rigid structure (rigid locking) than a support-retaining clasp, where the function of a masticatory pressure absorber is performed by the spring parts of the clasp. Therefore, when using such locking fasteners for terminal defects of the dentition, the load on the supporting teeth will always be higher than when using support-retaining clasps. In order to reduce the load on the supporting teeth and transfer part of the chewing pressure to the mucous membrane, the occlusal stop is excluded from the design of the locking fastening, i.e. “crushing” the chewing load, which can be used on teeth with weakened periodontium.
Fixation using telescopic crowns.
Telescopic crowns are a system of two crowns, one of which (internal - primary, or patrix) is cemented on a prepared abutment tooth, the other (external - secondary, or matrix) is located in the frame of the removable part of the prosthesis. Modern telescopic crowns can consist of the same main parts as support-retaining clasps and locking fasteners: occlusal stop, stabilizing part, retention part.
The tight contact of the occlusal parts of telescopic crowns serves as an occlusal stop. Stabilization of the prosthesis (protection of the prosthesis base from lateral shifts) is achieved by the vertical walls of the same telescopic crowns. Retention is carried out due to the friction force between the walls of the inner and outer crowns or with the help of special devices. The occlusal rest can be eliminated from the design of the telescopic crown. This is achieved by creating a gap in the resting position between the occlusal parts of telescopic crowns. In this case, most of the chewing pressure will be transferred to the mucous membrane, which can be effective with “weakened” supporting teeth.
Magnetic fixation.
Magnetic clamps have only two functions: support and retention.
The use of magnetic clamps has the following advantages:
• permanent retention;
• axial load;
• lack of activation;
• alignment of supports is not required;
• possibility of good hygiene.
Removable dentures with magnetic retainers, in addition to the mucous membrane, distribute chewing pressure on the supporting teeth, are securely fixed in the oral cavity, but due to the lack of a stabilizing part, they are unstable under horizontal load (lateral displacements of the denture base are possible). Therefore, a limitation for the use of magnetic fixators is the sharp atrophy of the alveolar ridges. Such clamps are used mainly as an additional element.
Fig. Fixation of dentures with magnets.
Conclusion
When prosthetizing patients with partial removable dentures, the doctor faces a number of tasks: firstly, the choice of the design of a partial removable denture - small saddle, arc, plate, with a plastic or metal base; secondly, solving the problem of fixation, which is complicated when there is an insufficient number of remaining teeth in the oral cavity, as well as the choice of fixing elements: retaining clasps, oro-retaining clasps, attachments, telescopic crowns, beam system, etc.; thirdly, identification of supporting teeth for fixing elements - analysis of the state of hard tissues and the supporting apparatus of the tooth; fourthly, assessment of the tissues of the prosthetic bed in order to identify a specific reaction to unusual conditions of transmission and perception of chewing pressure, represented morphologically by chronic reactive inflammation; fifthly, preventing a decrease in chewing efficiency in patients. An equally important task facing the doctor is the psychological preparation of the patient, since many of them perceive a removable denture as an attribute of old age.
Bibliography
- Kopeikin V.N., Demner L.N. Dental prosthetic equipment M.: “Medicine”. 2008;
- Orthopedic dentistry / S. D. Arutyunov; edited by I. Yu. Lebedenko, E. S. Kalivradzhiyan; Ministry of Education and Science of the Russian Federation. - M.: GEOTAR-Media, 2011.
- Guide to orthopedic dentistry edited by Corresponding Member of the Russian Academy of Medical Sciences Kopeikin V.N. M., "Triad-X". 2008;
- Orthopedic dentistry. Applied materials science. Trezubov V.N., Shteyngart M.Z., Mishnev L.M.. 2nd edition corrected and expanded. St. Petersburg, "Special Literature". 2006;
- Trezubov V.N., Shcherbakov A.S., Mishnev L.M. Orthopedic dentistry. Faculty course. Edited by Professor Trezubov V.N. 6th edition, St. Petersburg, “Foliant”. 2010;
- Trezubov V.N., Shcherbakov A.S., Mishnev L.M. Orthopedic dentistry edited by Trezubov V.N. St. Petersburg, "Spetslit". 2011.
- Zhulev E.N. Partial removable dentures, N. Novgorod, NGMA 2005.
- V.N. Kopeikin “Guide to orthopedic dentistry.”
- A.I. Doinikov, V.D. Sinitsyn “Dental materials science”.
- Markov B.P., Lebedenko I.Yu., Erichev V.V. Guide to practical training in orthopedic dentistry. Part 1., Part 2. M.: GOU VUMNTs Ministry of Health of the Russian Federation 2007.
- N.V. Kalinina, V.A. Zagorsky Prosthetics for complete loss of teeth. Ed. Medicine, Moscow, 1979, 2010.
- V.N. Kopeikin Errors in orthopedic dentistry. M., Medicine, 2006.
- M.G.Bushan, Kh.A.Kalamkarov Complications during dental prosthetics and their prevention. Chisinau "Shtiinta" 2004
- Orthopedic dentistry: textbook / ed. I. Yu. Lebedenko, E. S. Kalivradzhiyan. - 2011. - 640 p. : ill.
- Magazine "New in Dentistry"
Treatment
Preliminary treatment of the patient before dental implantation is performed includes sanitation of the oral cavity and special therapeutic measures. The pathology can be corrected with a bridge, plate or arch prosthesis. Depending on the size and nature of the anomalies, different types of structures are used:
- Non-removable bridges cover small flaws. Also, in such a situation, inlays and veneers are used.
- When large areas are damaged, correction is performed using bridge-shaped implants. Crowns can be metal-ceramic, metal, or other materials.
- Extensive lesions and edentia are treated with removable prosthetics. Implants are often made from acrylic.
- If there is no large group of units, it is practiced to install partially removable structures.
- For patients with an excessively deep bite and increased enamel abrasion, experts recommend clasp prosthetics.
Most clients note that modern designs and systems are convenient, practical, durable, and durable. Orthodontists are involved in prosthetics. High-quality materials allow you to achieve high aesthetic results. After selecting the structures, sanitation and removal of severely affected crowns and roots are performed. Professional cleaning of the oral cavity, removal of plaque and stone, and caries therapy are required.
The supporting units are prepared, after which a jaw cast is made. Using it, artificial crowns are created in the laboratory and their color is selected. The final prosthesis is made after fitting. It is fixed with cement. Removable structures are made by injection molding. After this, they undergo polymerization. When a whole group of units is missing and the patient does not agree to preparation, partially removable systems are used. Nylon structures solve minor pathologies, significant anomalies, and the problem of edentia. Ceramics is a popular material for prosthetics of the anterior group of teeth.
Preventative measures are very important. You should constantly observe the rules of oral hygiene and undergo systematic examinations by the dentist in order to promptly eliminate any resulting pathologies. It is easier to eliminate dental defects at the initial stage. This will help prevent serious complications.
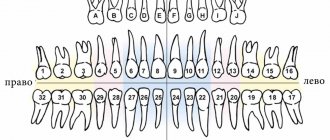
Kennedy classification
Edward Kennedy is an American dentist who was one of the first to perform quite complex operations to correct the bite.
Having extensive experience in practical work, he decided to divide all the most common dental anomalies into 4 classes, as well as three subclasses.
Kennedy proposed his system in 1921 and since then it has been the most frequently used and recognized by all world experts.
The first class includes defects when a person is missing chewing teeth on both sides of the arch. In addition to the main 1st class, there are 3 more subclasses:
- absence of teeth not only on the sides of the dental row, but also anywhere else in one place;
- absence of some teeth in 2 places (not counting lateral positions);
- absence of teeth in as many as 3 places in addition to the main lateral chewing ones.
The main option for a prosthesis for the treatment of deviations from the norm of the first group is the so-called labile fastening, which provides special devices for installing missing teeth, which should complement the damaged dental row.
Kennedy class 2 includes the presence of a unilateral defect coupled with loss of distal support. The subclasses here are exactly the same as in the previous version: 1st implies the presence of one lost tooth, in addition to the main defect, 2nd – two, 3rd – three.
The best method of correction is to use a prosthesis with palatal fixation on the side of healthy teeth, as well as labile type fastening on the side where the defect is located.
The third class includes unilateral disruption, but distal support is present. The subclasses are the same as in the previous versions. The best design for treatment is a special bridge prosthesis of a removable design using supporting clasps.
The fourth class has no subclasses and concerns the case when the front teeth located in the frontal part of the dentition are missing. The best treatment option here is the same as in the third class - installation of a bridge with supporting clasps.
What to do
End defects of teeth require immediate prosthetics to avoid serious problems with bite, appearance and health in general. It is important to understand that the displacement of adjacent teeth into the vacant space can lead to new difficulties, and it will be more difficult and expensive to install a denture.