Why do teeth rot in adults?
The development of caries and other dental diseases occurs under different circumstances, including:
- Insufficient oral hygiene or its complete absence.
- Poor nutrition, accompanied by the development of excess or deficiency of microelements and vitamins in the body.
- Failure to follow the rules of eating: chewing very cold or very hot food, combining hot and cold, biting into very hard foods.
- Disturbance of metabolic processes in the body.
- Endocrine diseases and temporary hormonal imbalances, due to which the protective properties of saliva are weakened.
- Pathological processes that occur during pregnancy and are associated with the outflow of nutrients from the mother’s body to the developing tissues of the fetus.
- Weak immune activity.
- Hereditary predisposition and improper formation of the dentofacial apparatus.
- The effects of nicotine and alcohol.
- The effect of toxic substances in unfavorable environmental conditions or harmful working conditions.
- Infectious processes due to injuries.
- The presence of untreated infectious processes in any part of the body.
When visiting a dentist, you rarely hear exactly why a particular dental disease has developed. Most often, unfavorable factors act on dental tissues in a complex manner and over a long period of time.
Why do children's teeth rot?
Teeth rot not only in adults, but also in children. In addition to the reasons described, children’s teeth are affected by additional factors that often arise due to the fault of parents:
- Improper nutrition of the mother during pregnancy, due to which the formation of bone and dental tissue of the fetus is abnormal.
- The effect of toxins and medications that enter the mother’s body through smoking, drinking alcohol or self-medicating.
- Long-term use of pacifiers and bottle nipples.
- Night feeding - at night, food particles linger in the mouth for a long time and rot due to the activity of bacteria.
- Late and incorrect teaching of children to maintain hygiene.
- Eating large amounts of sweets, the remains of which create favorable conditions in the mouth for the proliferation of microbes.
Symptoms of dental decay
A person may find out that his tooth has begun to rot too late - when the process of tissue destruction begins to develop in full force and will already cause great harm to the dentin and pulp. The main symptoms of a purulent process are:
- The appearance of stains on the top of the crown or in the cervical area if the root of the tooth rots. If a tooth rots from the inside (from the root canals), then the initial stages of necrosis can only be detected using x-rays: the visible surface of the crown turns black in the later stages of decay.
- Deformation of the tooth surface, the appearance of holes.
- Putrid, rotten odor from decaying tissues, caused by fetid waste products of bacteria that cause the process of decay.
- The appearance of an unusual, unpleasant taste in the mouth due to the entry of pus from the carious cavity or pulp chamber into the oral cavity.
- The appearance and gradual intensification of aching pain.
- Temperature increase.
- Increased accumulation of plaque with pathogenic microflora not only on the dentition, but also on the surface of the tongue or tonsils.
If a tooth has rotted to the root, its crown may completely crumble. Against the background of the destruction of the rotten tooth root, the patient may experience more frequent headaches.
Preservation of teeth with root fractures
Primary root fractures (PRF), traditionally referred to as “vertical root fractures,” are defined as “a complete or incomplete fracture that occurs in the root region of a tooth at any level, and is usually in a buccolingual direction.” It is logical that this definition of PPC is based on its anatomical location.
Since almost all teeth with PCD are pre-treated endodontically, it is reasonable to assume that there is some connection between the characteristics of endodontic intervention and the development of PCD. Based on the nature of the occurrence of PPC, the following definition was proposed: “a complication of endodontic treatment, which is characterized by complete or incomplete fracture of the dental tissues, begins in the root structure at different levels, and usually spreads in the bucco-lingual direction.” It is fundamentally important to understand that although PPC is a complication of endodontic treatment of a tooth, this does not indicate that PPC is directly related to any type of medical error during the procedure. And although treatment errors can lead to complications in the form of a fracture, not all root fractures are caused by procedural errors by the dentist, and some of the fractures develop even after completely adequate root canal treatment. Considering that PPC develops both among teeth after high-quality endodontic intervention, and in the structure of teeth after poor-quality canal treatment, we can conclude that the expanded definition of PPC includes both purely clinical and medical-legal aspects of assessing the quality of endodontic interventions.
The prevalence of PPC reaches 11-30%. A recent study by Yoshino et al in 2015 found that high prevalence of PPC was the leading cause of removal of endodontically treated teeth. In an analysis of 736 teeth from 24 different clinics, the authors were able to determine that 626 of them were extracted within 6 months after treatment, while 233 teeth were extracted as a result of the diagnosis of PPC (31.7%). Anatomically, RPCs often develop lateral to the root canal wall toward the outer root surface. Incomplete fractures extend only on one side of the root surface, while complete fractures extend in both directions, affecting two surfaces. Occasionally this leads to the root splitting into separate segments.
Timely diagnosis and proper treatment of such complications are crucial to prevent loss of alveolar bone, which can complicate further manipulations, including the possibility of dental implantation. However, the clinical and radiological diagnosis of PPC is quite difficult, and in some cases, the correct diagnosis can only be made through direct visualization of the root after surgical separation of the flap (Figure 1).
Photo 1. Diagnosis of tooth root fracture during direct imaging after flap separation.
Traditionally, teeth with PCD were considered hopeless from the point of view of functional prognosis. Possible treatment approaches for PPC have included tooth replantation after bonding the two fractured segments, but such approaches are not sufficiently evidence-based to be implemented in daily clinical practice. Therefore, the remaining treatment alternative was extraction.
For many years, there has been an ongoing debate among clinicians about whether it is worth trying to preserve a compromised tooth as much as possible, or whether it is better to remove it and immediately proceed to the dental implantation stage. In recent years, given the level of prevalence of peri-implantation complications, it has been suggested that the treatment of one’s own teeth, even those compromised by a fracture, is simpler and more predictable compared to the treatment of peri-implantitis, the problem of which continues to progressively increase in modern dental practice.
In recent years, a number of new algorithms have also been proposed, including promising alternatives for the treatment of teeth with PCD, which until now have traditionally been referred to extraction. These unique single-unit treatments for teeth with root fractures are in the early stages of development and refinement, and data on them are mainly based on single publications. However, modern endodontics offers a number of technical means such as devices for magnification and lighting, as well as a set of modern materials such as bioceramic cements, which expand the possibilities for the restoration of teeth with root fractures with the correct selection of appropriate clinical cases with a clear understanding of the difference between which tooth can still be saved and which can no longer be saved. This article will discuss modern possibilities for treating teeth with PPC.
The importance of choosing a clinical case for treatment
Modern endodontics provides many treatment options that can save compromised teeth. However, PPC still poses a diagnostic and therapeutic challenge for dentists, as root fracture is the reason why most endodontically treated teeth have to be removed. In addition, with the development of modern endodontic treatment options, new dilemmas have emerged regarding the functional prognosis of treated teeth. The topic of discussion remains the decision about the possible preservation of a compromised tooth with PPC or its extraction with restoration of the edentulous area using a dental implant. Traditionally, it was believed that the sooner a tooth with a root fracture is removed, the better, because the presence of one in the jaw provokes the development of inflammation, which, spreading to the periodontal area, provokes the formation of a destructive bone defect. Under such conditions, bone loss, in turn, compromises the prognosis of the future implant, which can be installed in place of the problematic tooth. However, each individual clinical case should be assessed objectively, since some data have shown that with an adequate selection of a suitable clinical situation, teeth affected by a root fracture with a limited distribution do not provoke the development of inflammation in the surrounding periodontium over a fairly long period of time. The selection of clinical cases of PPC suitable for conservative treatment should be based on evidence-based protocol data, taking into account the completeness of the diagnosis and available therapeutic options.
The dentist must also take into account the aesthetic needs of the patient, the duration of functioning of the treated tooth and the costs required for its restoration. When making decisions about possible conservative treatment of teeth with PCD, one should take into account not only endodontic aspects, but also periodontal, prosthetic and aesthetic components of the patient’s rehabilitation. Many factors, such as the location of the tooth, the presence of predisposing periodontal disease, the type of coronal restoration and the possibility of using modern endodontic materials and instruments, must be taken into account by the doctor when assessing the risks and benefits of conservative treatment of teeth with a root fracture.
In cases of development of PKD in multi-rooted teeth, there may be no need to preserve the root with a fracture, since it can simply be amputated. With single-rooted teeth, the situation is different, and the functional prognosis of such teeth depends on the adequate choice of treatment method. Predisposition to periodontal pathology negatively affects the prognosis of teeth with PCD. Thus, during the initial diagnosis of teeth with root fractures, it is necessary to carefully assess the presence and severity of possible adjacent periodontal lesions.
The inability to preserve a tooth (even if one with a root fracture) in the dentition significantly reduces the patient’s aesthetic profile. And although in most clinical cases implants take root absolutely without problems and serve successfully for many years, the long-term prognosis of such implants must also necessarily include the parameters of the achieved aesthetic rehabilitation. After all, if disintegration of the implant occurs in the frontal area, then the aesthetic profile of not only the immediate area of implantation is disrupted, but also the entire aesthetic profile, which is subsequently quite difficult to correct.
It should not be forgotten that in cases of preservation of teeth with PCD, gum recession and alveolar loss of surrounding bone tissue often develop in the area. Especially often, such symptoms develop in patients with a thin biotype of periodontal tissue. Thus, a thorough assessment of aesthetic and periodontal parameters should be a mandatory component of planning a comprehensive treatment algorithm for patients with PPC.
The long-term prognosis of the functioning of treated teeth with PCD is also influenced by prosthetic parameters: for example, the crown-to-root ratio, the amount of vital tooth structure and the presence/absence of tooth ferrule. In fact, adequate crown restoration is another of the most important factors affecting the survival of a tooth after treatment. In addition, due to the absence of pathognomonic radiographic signs or clinical symptoms of PPC, the prognosis of the future functioning of the compromised unit of the dentition can only be assessed after completion of the restoration of its coronal part with an appropriate superstructure.
Treatment Alternatives
If preserving a tooth with PCD is the initial goal of complex treatment of the patient, to achieve this goal, the doctor can use a number of surgical and conservative approaches, including root amputation or hemisection, apicoectomy with resection of the fractured root coronally relative to the fracture line, performing a replantation procedure, flap separation and restoration areas. Despite the variability of approaches over the past decades, there has been a change in the trend towards the subsequent effect after treatment: if previously the majority of treated teeth with PCD eventually had to be removed, now their survival rate has increased throughout the entire monitoring period.
Root amputation or hemisection
When diagnosing PPC in a multi-rooted tooth structure, the most logical treatment option is surgical amputation of the fractured root. About a hundred years ago in 1884, Farrar proposed a surgical approach that involved resection of one of the roots of the problem tooth and filling the endospace of the remaining one. At the same time, Farrar performed root resection at different levels in different clinical cases, thus sometimes leaving only a short “snip” of hard tissue in the gums (photo 2).
Photo 2. Root amputation procedure during endodontic surgery.
a. The patient had a fistula in the area of the upper molar. After diagnosis, a diagnosis of chronic apical abscess was made. b. During the surgical procedure, the mesiobuccal root was removed. c. Two years after the operation, the tooth showed no symptoms, and the presence of replacement hard tissue was noted in the amputation area.
In their study, Anitha and Rao (2015) reported that the root resection procedure to remove the cracked root fragment is completely predictive of the relative prognosis of the remaining tooth. But again, to achieve successful results of the intervention, you need to carefully approach the selection of a clinical case, taking into account the condition of the periodontium and the design of the future prosthetic structure. Depending on the specific clinical conditions, the resection procedure has several subtypes and modifications, for example, the resection can be extended to include part of the crown, and in some cases it is carried out together with orthodontic extrusion of the remaining part of the tooth. Root amputation, or hemisection, is more indicated for upper or lower molars in cases where only one of the roots is broken. Taking into account the condition of the periodontium and the location of the fracture line, resection can be performed at different levels, and sometimes it is possible to preserve even the coronal part of the root, which is subsequently filled. In cases of fused roots, amputation is not recommended. It should also be noted that although root amputation can be performed in mandibular molars, hemisection or resection is a more predictable procedure for these teeth. The large length of the root and the short distance between the teeth in the area of their furcation negatively affect the surgical prognosis of resection, since in such cases the implementation of this procedure is purely technically complicated.
Cementation of the root fracture area with further replantation
Many case reports have reported attempts to cement the root fracture site followed by tooth replantation, which have shown fairly variable results with long-term monitoring. Hayashi et al in 2004 described a case of treatment of PPC by restoring the fracture site with a composite bonded to the tooth wall, after which the latter was replanted back into the socket. In 18 of the 26 cases analyzed, the teeth continued to function successfully for another 4-76 months. At the same time, the authors noted that the treatment of teeth with a fracture that extended more than two-thirds of the length from the neck of the tooth to the apex area, as well as the restoration of distal teeth, is less successful compared to other clinical cases.
Nizam et al in 2016 evaluated the results of 21 replanted teeth that had been previously extracted and restored in the APC area with resin cement. After replantation, all teeth were splinted to adjacent teeth. The authors reported that out of 21 treated teeth, 2 were extracted within the first month after treatment. The values of periodontal indices (plaque index, gingival index, probing depth and clinical attachment level), as well as periapical index (PAI) in the area of the treated teeth 12 months after surgery were significantly lower compared to the initial situation. Taking into account the data obtained, the authors summarized that performing adhesive cementation and deliberate replantation of teeth with PPC can be relatively effective only in cases of treating single-rooted maxillary teeth.
Kawai and Masaka 2002 proposed a modified method for replanting teeth with PCD after restoring the fracture site by rotating the tooth 180 degrees from its original position. In this way, it is possible to reposition the fracture line below the level of the bone covering and periodontal ligaments, minimizing the risk of complications. Other authors (Hadrossek and Dammaschke 2014) have presented cases of retrograde root filling with fracture using calcium silicate cement (biodentine).
Although intentional tooth replantation may be considered a predictable treatment option in some clinical cases, restoring the fracture line with any material is itself a controversial therapeutic approach. Indeed, for such treatment, the tooth must first be extracted, without provoking any segmentation of it into parts during removal. The aspect of the development of resorption after replantation also remains problematic. Thus, a contraindication to replantation is a condition of the teeth in which they cannot be safely removed, or their periodontal status is compromised. Also, such manipulation is not recommended for patients with severe somatic diseases.
Cementation of root fracture after flap separation
More than two decades ago, Selden (1996) described the treatment of teeth with incomplete PCDs using glass ionomer cement and bone graft. Ultimately, however, the author reported that all six cases treated in this manner ultimately failed. At this time, using the capabilities of lighting and magnification, the doctor has a wide range of methods for working with the root system of the tooth, which allows achieving high accuracy of iatrogenic interventions. Modern endodontic materials, such as mineral trioxide aggregate (MTA), have been repeatedly used by doctors to restore root fracture sites. The protocol for this treatment involves creating a groove along the fracture line, which is subsequently sealed with MTA. Taschieri et al in 2010 analyzed the results of treatment of maxillary anterior teeth that were diagnosed with a root fracture. Teeth with deep periodontal pockets and radiographic evidence of periapical lesions were excluded from the study. During treatment, the flap was separated; a groove was formed along the fracture line with an ultrasonic instrument, which was then filled with MTA. The existing bone defect was filled with calcium sulfate material. After 33 months, 5 of the 7 initially treated teeth showed successful results, while the remaining 2 had to be removed during monitoring. Floratos and Kratchman in 2012 tried to treat 4 distal teeth with a similar intervention. After separation of the flap, the authors performed an oblique resection of the root, and its residual part was filled with MTA. The osteotomy area was covered with a collagen membrane, and the treated teeth were observed for 8-24 months. The results obtained were classified as successful (Floratos and Kratchman 2012). In a recent study, Taschieri (2016) reported a case of treatment of a maxillary left central incisor in which an incomplete root fracture was diagnosed. After separation of the flap, the doctor confirmed the presence of a fracture. The broken part of the root was removed and the defect area was filled with platelet-rich plasma. After 24 months, the tooth remained asymptomatic. The authors suggested that a similar surgical approach could be successfully used in the treatment of endodontic-periodontal lesions associated with incomplete PPC. Although most reports show promising results, flap separation itself carries the risk of possible gingival scar formation and the potential risk of further recession. Also, such manipulation can provoke excessive bone loss in the surgical area. Given such complications, before carrying out such manipulations, the potential risks should be carefully assessed, especially if the intervention is carried out in an aesthetically significant area.
conclusions
In order to decide what to do with a tooth that has a root fracture, you need to take into account a number of specific factors that affect the success of a possible treatment algorithm. The choice, in fact, is simple - the tooth can either be removed and the edentulous area can be restored with an implant, or the tooth can be tried to be saved. Despite the fact that extraction of teeth with root fracture remains the method of therapeutic choice, new endodontic instruments and materials allow the doctor to compete for the prognosis of the problematic unit of the dentition. To formulate any evidence-based conclusion about the algorithm for choosing an appropriate method of treating teeth with PPC, a number of additional studies are required that will make it possible to unambiguously assess the prognosis of the functioning of restored teeth in the long term.
Authors: Eyal Rosen, Ilan Beitlitum, Igor Tsesis
What are the dangers of rotten teeth, consequences for the body
Many people ignore the process of tooth decay unless it is accompanied by severe pain. But the consequences of the carious process can be unpredictable and dangerous. If you have rotten teeth, the following complications may develop:
- Destruction of bone tissue of the musculoskeletal system.
- Endocarditis is inflammation of the lining of the heart.
- Inflammatory pathologies of the kidneys.
- Infections of ENT organs.
- Psychological complexes due to discomfort during communication and dissatisfaction with the appearance of the dentition.
- Purulent-inflammatory diseases in the gums (abscesses, phlegmons) and, as a result, the spread of infection throughout the body, leading to general intoxication.
The health of baby teeth greatly affects the condition of the permanent buds. Therefore, if nothing is done about the decay of milk dental tissues, in the future the child may have big problems with the formation of a permanent dentition.
How to recognize a dead tooth?
When a tooth dies, many adverse reactions occur. With the necessary knowledge, you can easily recognize the problem. Due to irritation of the tissues around the tooth, gum abscess (in the form of a thick discharge consisting mainly of bacteria) and swelling may occur. A dead tooth can also be recognized by its dark, unnatural color, which is the result of cell death, and by its complete lack of response to any stimuli (heat, cold, or electrical stimuli). In the transitional stage preceding the death of the pulp, there may be increased sensitivity to heat and cold, as well as throbbing toothache.
In the last stages of tooth death, fever, chills and jaw pain may appear. Tarnishing of the enamel is also a warning sign. If any of the above symptoms appear, a visit to a specialist may be required to make a final diagnosis.
What to do if your teeth are rotting
Rot inside the tooth is dangerous for the entire body. Therefore, at the first signs of decay of dental tissues, you should go to the dentist.
Before providing first aid, it is recommended:
- Rinse your mouth with a herbal decoction that has anti-inflammatory and antimicrobial effects. It's better to take chamomile and sage.
- Rinse your mouth with a pharmaceutical antiseptic: Chlorhexidine, Miramistin.
- Thoroughly clean the surface of the dentition to prevent the accumulation of soft plaque and its transformation into hard tartar: bacteria multiply under its surface and spoil the enamel even faster.
- You should not try to remove pus yourself by picking at the enamel with a sharp object. This action will provoke even greater destruction of damaged tissue.
- On the side of the jaw where the rotten tooth is located, it is better not to chew anything so that food does not penetrate into the carious holes.
- After eating, you need to rinse the remaining pieces of food with a weak saline solution or boiled water.
Causes of depulpation
There are a number of indications for dental nerve removal. Depulpation is most often carried out in the following cases:
- with extensive carious lesions affecting the dental nerve;
- development of infection in the dental canal;
- mechanical damage to the pulp;
- In the process of preparing for prosthetics, even a healthy pulp may be removed; this is necessary to eliminate the risk of developing re-inflammation in the tooth after the installation of an orthopedic structure.
The procedure for removing pulp from a tooth is performed in the following sequence: 1. Based on an x-ray taken, the doctor determines the structure and size of the dental canals. 2. Local anesthesia is administered. 3. The pulp is removed first in the coronal and then in the root part of the tooth. 4. Dental canals without pulp are carefully treated with an antiseptic solution. 6. After treatment, the canals are sealed. 7. Most often, a temporary filling is subsequently placed on the tooth, which later must be replaced with a permanent one.
Treatment in dentistry
Whether a tooth can be treated depends on the severity of the carious process, so doctors first prescribe x-rays to patients. If the situation is not critical and the dentist can save the tooth from rotting, he carefully cleans it of accumulated deposits (plaque and stone) and begins treatment:
- Anesthesia is performed.
- All areas of enamel affected by the carious process are removed, and the rotting pulp must also be removed.
- The dental cavity is washed with an antiseptic.
- The integrity of the surface is restored with filling material. After the filling is installed and hardened, the patient must check the bite: if discomfort is felt, the excess layer of filling material must be removed.
Teeth that are rotting from the gums are treated in the same way, but photopolymer materials are usually used to fill them. They harden quickly, are characterized by increased strength and high aesthetics.
The dentist may prescribe an antibiotic to prevent the infection from spreading throughout the body. For severe pain, an analgesic is prescribed.
There are methods that can be used to prevent damage to dental tissues by cariogenic bacteria. Almost all dental clinics carry out remineralization - strengthening the enamel structure with special preparations. In a hospital or at home, you can perform fluoridation - saturating the enamel with fluoride.
Can a dead tooth hurt?
The appearance of pain in a dead tooth depends on the stage at which necrosis progresses. At the very beginning there is usually no pain. During the transitional stage, the already mentioned throbbing toothache may appear. It is a consequence of retention of purulent exudate and usually worsens in a lying position. After its cessation, complete necrosis of the dental pulp occurs.
Pain can also occur as a result of dental treatment. If a dentist places a prosthetic crown that is too large on a tooth, there is a high probability of overloading the tooth and causing periapical changes. In this situation, pain usually occurs during chewing. It can be easily eliminated at your next visit to the dentist by shortening the crown.
Do I need to remove rotten teeth?
If a tooth root or crown is completely rotted, it cannot be restored. Such a tooth cannot be left in the jaw so that its purulent contents do not spread to the surrounding tissues. If there is rot in the root canals, it is not possible to make artificial crowns, since they will not be able to fix on the destroyed tissues. Therefore, in advanced situations, dentists prescribe the removal of a rotten tooth, and this operation cannot be refused. After removal, a course of antibiotics may be prescribed.
To prevent your teeth from rotting, you need to regularly monitor their condition. To maintain dental health, you need to adhere to a nutritious diet and maintain oral hygiene, as well as promptly treat any dental and internal diseases. Purulent processes are extremely dangerous, therefore, if the carious process has reached an advanced stage, you should not refuse to remove the diseased tooth.
What are the causes of dead tooth formation?
The most common causes of dead tooth formation are primarily caries and mechanical trauma. However, the first reason is much more common. Bacteria that appear during the formation of carious cavities are responsible for tooth death. They produce many toxic substances. These substances then cause gradual and, over time, irreversible damage to the dental pulp. At the first stage, the pulp becomes inflamed and pulpitis occurs. Over time, with the constant deepening of carious cavities, the layer of dentin surrounding the pulp begins to shrink. And harmful bacteria have easier access to attack the pulp. In subsequent stages, pulpitis worsens, which eventually becomes irreversible, after which the pulp dies.
Another reason for the formation of a dead tooth is mechanical trauma. The most common ones include falls, impacts, and knocking out a tooth. This can result in reduced blood flow to the pulp, reducing the availability of all nutrients and oxygen. The cells die, and the pulp irreversibly dies along with them.
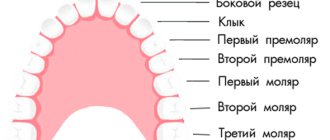
Types by localization of the pathological process
Caries of the anterior teeth is localized:
- Cervical: caries begins near the neck in the gum area or under it. The main reason for this is poor oral hygiene.
- Interdental: carious lesion is observed between two incisors. Often this type of disease occurs with a small gap between them. This is where food debris gets stuck, which decomposes and causes damage to the enamel.
- Fissure: affects the grooves on the tips of the teeth. Typically, this form of the disease develops on molars, rather than on incisors and canines.
Most often, caries of the front teeth is interdental. If left untreated, the stain spreads to both incisors. If the disease starts, a hole will form between the teeth, which will be difficult to repair. At any moment, enamel and hard tissues can split into several parts.
Treatment for severe crown lesions
If caries affects more than 50% of the incisor or canine tooth, it will not be possible to install a filling. After removing the carious areas, the patient is sent to an orthopedist for installation of an orthodontic structure: a bridge, crown, veneer or lumineer. They allow you to hide a cosmetic defect that appears after an illness.
If the tooth is completely destroyed by caries, but the root remains, the doctor installs a pin and a crown. If a tooth is completely lost, an implant will be required. This is one of the most expensive dental procedures.