From this article you will learn:
- causes of fissure caries,
- How is fissure caries treated?
Fissure caries is a carious lesion of tooth tissue, which is localized in the fissures of chewing teeth. Fissures should be understood as natural depressions on the chewing surface of large molars, which look like grooves. Human teeth usually have 3 favorite areas for caries to appear - tooth enamel is affected primarily in the cervical area, in the interdental spaces, and in the fissure area of large molars (since this is where food debris and plaque accumulate due to irregular oral hygiene) .
Therapy of fissure caries is not a complicated procedure, and most often problems arise only when diagnosing caries in narrow, deep fissures. In dentistry, fissures are usually divided into “open” and “closed”. Open fissures should be understood as depressions, the bottom of which is visually clearly visible. Closed fissures resemble a bottle in shape. From the outside, upon examination, only a narrow groove (bottleneck) is visible, but in the depths the fissure expands, forming a cavity.
Fissure caries: photo
In Fig. 3 (cut of a tooth) you can see what caries looks like in closed-type fissures - the entrance hole to the fissure is very narrow, but underneath there is a massive carious lesion. Diagnosing caries in such closed fissures can be very difficult.
What is fissure caries?
Fissures - this professional term refers to the natural pits and grooves that exist on the surfaces of chewing teeth. In these recesses, food debris clogs and accumulates, and therefore the fissures of the chewing teeth are vulnerable to caries. Therefore, it is so important to thoroughly brush your teeth and clean the fissures of your chewing teeth from plaque and food debris.
Fissure caries is clearly visible on the surface of the tooth, but only if the tooth has open fissures, that is, those natural depressions, the bottom of which is completely visible visually. But chewing teeth also have closed fissures: the structure of this type of fissure is very similar to the structure of a bottle. In closed fissures, only the upper narrow groove is clearly visible upon examination, but in depth it expands and forms a cavity. Diagnosing caries with closed fissures is a difficult task and, of course, you won’t find such caries on your own; you will definitely need to visit a doctor’s office.
In order to prevent fissure caries and begin its treatment in a timely manner, you need to undergo regular preventive examinations at the dentist’s office. Our VENSTOM dental clinic in Moscow uses the most modern diagnostic equipment and techniques to detect and treat caries on time!
Calculate the cost of treatment by taking a short test in 20 seconds!
Do not delay your treatment, because in this matter time plays against us.
Causes and symptoms of caries formation on fissures
The fissure surface is an ideal environment for the accumulation and reproduction of pathogenic microorganisms. It is for this reason that caries begins to form in such areas and develops dynamically. That is why the main cause of fissure caries in patients is insufficient oral care.
The first symptoms of the disease are pain from hot drinks and foods. The grooves on the teeth gradually darken, the sensitivity of the teeth increases, and there is slight pain.
Why does fissure caries occur?
Fissure caries occurs for only one reason - poor dental and oral hygiene. If after eating you do not brush your teeth, do not rinse your mouth and perform dental hygiene less than 2 times a day, fissure caries will not keep you waiting, because plaque and food debris quickly accumulate in the pits and depressions on the surfaces of the chewing teeth. This environment is extremely favorable for the development of carious bacteria.
Bacteria will multiply, their vital activity will lead to weakening of the tooth enamel and when it becomes thinner to a certain extent, fissure caries will begin.
Prevention of fissure caries at home
It is important to observe prevention not only at dental appointments, but also at home. Oral hygiene is a complex procedure. It includes:
- Individual cleaning with a medium-hard brush. The necessary components of toothpaste are active calcium (ROCS, Colgate, etc.) and fluoride (President Classis, Splat, etc.);
- Using dental floss to clean the interdental spaces;
- For more thorough hygiene, it is recommended to use an irrigator;
- After traditional brushing, do not forget to rinse your mouth with sodium fluoride solutions. The optimal fluorine concentration in the solution is 250 ppm.
The prognosis for fissure caries is favorable. Thanks to planned treatment, oral sanitation and good hygiene, relapse can be prevented and complications can be avoided. To improve the condition of your teeth, you need to take care of them, as well as adhere to a balanced diet and exclude carbohydrates from your diet. Remember: healthy teeth are the guarantee of a snow-white smile.
Make an appointment with a therapist by phone+7(985)532-21-01
Acute traumatic pulpitis treatment in the clinic on Tverskaya, Chekhovskaya
Tetracycline teeth treatment, whitening, veneers
Retrograde pulpitis: diagnosis, causes, treatment, complications
Removal of a wisdom tooth cyst
Hypoplasia of dental enamel, diagnosis and treatment
Tooth root caries treated or removed
Caries in the white spot stage
Signs of fissure caries
By what signs can you recognize the development of fissure caries? Fissure caries has the same symptoms as other forms of the disease:
1. With fissure caries in the staining stage on the chewing surfaces of the teeth, you can see a change in the shade of the enamel - it becomes whitish. Apart from whitish spots, fissure caries does not show itself in anything at this stage of development - the tooth does not hurt.
2. With superficial fissure caries, the spots become larger and darker, acquiring a distinct contour. Tooth sensitivity to hot/cold, sour/sweet foods may occur.
3. Average fissure caries already affects the dentin, so the destruction of the tooth will be clearly visible - a cavity will appear on the surface of the crown, which is popularly called simply “a hole in the tooth.” Unpleasant sensations may occur when eating, but usually they pass quickly - you just have to stop chewing on the affected tooth and rinse your mouth well.
If fissure caries is not treated, it will turn from medium to deep and the destructive process will reach the pulp (nerve) of the tooth. If the infection penetrates into the pulp, the dentist will no longer have to treat fissure caries, but its complication - pulpitis.
Any person can notice rare and deep fissure caries on their teeth during dental hygiene, but the diagnosis of fissure caries in the spot stage and fissure superficial caries requires a visit to the doctor’s office. Small specks of demineralized enamel may not be noticed under plaque, which is actively accumulating in the fissures, and even more so it will be impossible to independently detect caries if the fissures are closed.
Anatomy of fissures of the chewing group of teeth
Fissures are anatomical depressions and grooves between the cusps on the chewing surface of the crowns of the lateral teeth (premolars and molars). They provide food chopping and grinding. Depending on their structure, fissures are divided into four types:
- Cone-shaped;
- Grooved;
- Teardrop-shaped.
The deeper and narrower their shape, the greater the likelihood of developing cariogenic microflora. Food particles remain in natural cavities even after thorough brushing. This contributes to the active spread of the pathological process.
Diagnosis of fissure caries: basic and auxiliary methods
The main diagnosis of fissure caries will consist of visual inspection and probing. If caries has affected the fissures, they will noticeably darken, the tissue in them will soften and the probe that the dentist uses during the examination will get caught on them. But if the caries is still in the staining stage or the tooth has deep and narrow fissures, additional diagnostic measures can be carried out:
- X-ray of a tooth. A fairly effective diagnostic method that allows you to detect fissure caries at the earliest stages of development, since carious lesions will be clearly visible on the pictures;
- Fissurotomy. A specific study that helps to see how deep the carious damage has gone in the tooth. Fissurotomy is carried out as follows: using a drill, the doctor opens the fissures to a small depth (up to 1 mm) and looks at how much caries has managed to destroy the tooth.
Diagnosis of fissure caries can be carried out using a laser. This is the most modern and effective method for diagnosing caries at any stage of its development: the laser is reflected differently from healthy and diseased tooth tissues. The difference in the reflections of the laser beam is noted by the device, which immediately sounds a sound signal. But laser diagnostics of fissure caries is carried out only in those clinics that have the appropriate equipment.
Indications and contraindications
Since every person has fissures, their sealing can be recommended for all patients. As mentioned earlier, most often such preventive measures are prescribed in childhood. This is due to the fact that the milk and newly emerged radical units are very weak and not resistant to the aggressive effects of bacteria. The enamel of such teeth still lacks the minerals that are necessary to protect against caries.
For patients over 20 years of age, sealing may be recommended for deep and very narrow grooves. They are almost impossible to clean well during daily hygiene procedures.
Unfortunately, like any treatment, this technique has some contraindications. Sealing is not carried out when caries or pulpitis is detected, when a unit has partially erupted above the gum tissue, as well as when the unsatisfactory general condition of the teeth and gums is diagnosed due to a lack of daily hygiene procedures.
previous post
What to do if a dental implant is loose?
next entry
How will fissure caries be treated?
After diagnosing and diagnosing “fissure caries,” a method of treating it is selected. Since patients usually come to dentists with moderate fissure caries, below we will describe all stages of its treatment.
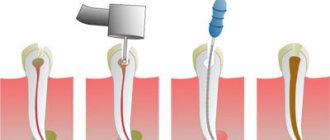
1. Pain relief. When treating medium fissure caries, the doctor will need to remove all affected and destroyed tissue with a drill. This can be unpleasant for the patient, so local anesthesia is given before treatment begins.
2. After the anesthetic has taken effect, a rubber dam, a special latex overlay, is installed on the area where fissure caries is treated. The rubber dam reliably isolates the area of treatment from saliva and moisture from the oral cavity, which may contain bacteria. In addition, careful isolation of the tooth from moisture is important for high-quality filling. If moisture gets into the cavity at the time of placing the filling, the adhesion between the filling materials and the natural tissues of the tooth will deteriorate and this can lead to the filling falling out.
3. After installing the rubber dam, the dentist will begin working on the tooth. When treating fissure caries, it is extremely important to remove all destroyed and damaged tissue. If this is not done, caries will continue to develop directly under the filling.
4. By removing tissue damaged by fissure caries, the dentist will form a cavity in the tooth for installation of a filling. This cavity is treated with a special etching solution that cleans the tissue, and then an adhesive composition is placed into it.
5. The dentist will restore >the crown of the tooth
The process of treating fissure caries is completed by grinding and polishing the installed filling.
If a tooth is severely damaged by fissure caries, then it is better to restore it not with a filling, but with a special restorative inlay, which can be made of different materials: gold, ordinary metal, ceramics.
Inlays are fixed in the tooth using special cement and differ from fillings in having a longer useful life, and in addition, in reduced risks of developing secondary fissure caries. In addition, fillings even made from the highest quality composites darken over time, but ceramic inlays retain their aesthetic appearance throughout their entire service life. Of course, restoring a tooth with an inlay after treating fissure caries will cost more, but the high cost will be justified by the durability and reliability of the restoration.
Remineralizing therapy
If caries is in the spot stage, local remineralizing therapy is carried out as a preventive measure and treatment, which compensates for the loss of mineral components of the enamel resulting from demineralization. This method accelerates the mineralization of enamel after tooth eruption, saturates the enamel with mineral elements, which increase its resistance to acid attack, and also helps restore early carious damage.
Indications for remineralization are:
- single and multiple stains on the surfaces of teeth, mainly in the cervical area;
- prevention of caries in patients who have an increased risk of developing this disease (for example, those who wear braces).
Remineralization is carried out in stages; during the procedure, the surface of the teeth is thoroughly cleaned with brushes and abrasive paste, treated with a solution of hydrogen peroxide, dried with air or a cotton swab, and a remineralizing solution is applied to the surface. The final stage is to re-dry the teeth and apply cotton swabs soaked in sodium fluoride solution to them, or coat the enamel with preparations containing fluoride.
Remedies for remineralizing therapy can be solutions of calcium gluconate, calcium phosphate, Remodent, as well as Lukomsky fluoride paste rubbed into the affected areas.
Borovsky-Volkov method
The essence of this method is to carry out applications of a two-component composition, including a solution of calcium nitrate and a solution of ammonium acid phosphate, as a result of which brushite is formed on the surface of tooth enamel and in the spaces of the subsurface layer - a substance that is a source of phosphorus and calcium ions, which play an important role in remineralization .
Application of GC Tooth Mousse
An innovative remineralizing agent is GC Tooth Mousse, a component of which is casein phosphopeptide extracted from cow's milk. Thanks to the “stickiness” of this element, there is a good bond with dental tissues, mucous membranes, plaque and microorganisms, resulting in the formation of a depot of remineralizing ions. GC Tooth Mousse is used to prevent caries, treat demineralization of tooth enamel in individual lesions, as well as to eliminate dentin hypersensitivity and prevent this pathology after a number of dental procedures. The only contraindication is an allergic reaction to milk protein.
Author Khachak M.A.
Is it possible to cure fissure caries without drilling the tooth?
Fissure caries can be cured without drilling a tooth, but to do this you need to regularly visit the dentist’s office and undergo preventive examinations. If fissure caries is detected at the spot stage, it is treated without drilling the tooth, through remineralization or Icon technology.
From here we can draw a simple conclusion - if you want to treat your teeth without pain and drilling with a drill, you need to pay close attention to the prevention of caries.
Calculate the cost of treatment by taking a short test in 20 seconds!
Do not delay your treatment, because in this matter time plays against us.
Prevention
Every six months a person should come to the dentist for a preventive examination, even if he is not bothered by any symptoms. Also, to prevent the development of caries, it is recommended:
- brush your teeth at least twice a day;
- rinse your mouth after every meal;
- use mouth rinses;
- carry out additional cleaning of teeth with an irrigator;
- stop smoking;
- eat less sweets.
Dental treatment is expensive, so it is better to make every effort to avoid dental diseases. When the first signs of caries appear, consult a doctor immediately.
How to prevent fissure caries
The best prevention of fissure caries is regular and high-quality oral hygiene, as well as periodic professional teeth cleaning in the dentist’s office.
If you have deep, closed fissures, fissure sealing can be an effective method of preventing fissure caries. This is a simple event during which the fissures are sealed with a special sealing compound. Fissure sealing is carried out in both children and adult patients and helps to significantly reduce the risk of developing fissure caries.
An excellent method of preventing fissure caries is a course of remineralizing therapy. The essence of the procedure is to treat teeth with special compounds based on fluoride and calcium, which strengthen tooth enamel.
Do you still have questions about the treatment of fissure caries? Ask them in the chat on the website of our dentistry in Moscow - VENSTOM, or even better - come for a consultation with our specialists!
Preliminary sealing of fissures as a method of preventing caries of erupting teeth
Pit and fissure sealant is used as a means of both primary and secondary prevention of caries on the chewing surfaces of teeth.
After almost four decades of use in clinical practice, pit and fissure sealing is recognized as one of the most effective and convenient methods for preventing the development of caries on chewing surfaces in children.
According to statistics, caries of the pits and fissures of permanent molars is the main dental problem in school-age children, and there is reason to believe that up to 20% of caries cases are initiated during teething.
However, in older children and young men, caries develops according to a different pattern, in which the proximal surfaces of the teeth are more often affected.
At the age of 13 years, proximal caries accounts for approximately 30% of the annual increase in caries incidence, and at the age of 27 years it increases to 50%.
The article discusses the method of preliminary sealing of fissures to protect the chewing surfaces of permanent molars and proposes a new method for the prevention of caries of proximal surfaces using sealing materials.
Localization specifics: open and hidden surfaces
The appearance of white spots is associated with excess acid production by bacteria and the accumulation of plaque over time. The specificity of the localization of open surfaces is that they are less susceptible to adverse effects due to good mechanical cleansing and salivation.
Hidden tooth surfaces, on the contrary, are poorly cleaned mechanically, are less accessible to chemical protection with saliva and fluoride and, accordingly, are more susceptible to caries. It is important to remember that in different situations the risk of developing the disease for the same surfaces may change up or down.
Example 1: A large white spot that forms on the proximal surface of a tooth while it is hidden may be arrested or remineralized after loss of the adjacent tooth (Figure 1).
Rice. 1
Example 2: The distal and mesial surfaces of the first permanent molar can be said to be open during the change of teeth, when the second primary molar has already fallen out and the second permanent molar has not yet erupted. We suggest protecting these surfaces in high-risk children before they become hidden again after the eruption of the second permanent molar and premolar.
These surfaces must be sealed with a thin, wear-resistant sealant while they are still open and therefore accessible for treatment. This applies to any surfaces considered to be at risk of developing caries.
Example 3: The occlusal surface of an erupting tooth can be defined as hidden as long as it is covered and inaccessible to the toothbrush. It becomes open after eruption and receives all the positive qualities of the self-cleaning effect during physiological occlusion.
In a slowly erupting permanent molar, plaque usually accumulates under the shell, which requires professional prophylaxis during eruption.
An increase in eruption time is accompanied by the accumulation of a large amount of plaque under the shell, and the area of demineralization is not limited only to pits and fissures, but, as a rule, extends to a significant part of the enamel under the shell (Fig. 2).
Rice. 2
There is a big difference between the accumulation of plaque on the chewing surfaces of erupting and fully erupted molars, which is that an unerupted or partially erupted tooth does not function, and is also covered with a membrane. In addition, there is a risk of food debris getting into the space between the enamel and soft tissues of the tooth (Fig. 3).
Rice. 3
The length of the eruption period is another risk factor, since teeth with a long eruption time are more likely to be affected by caries. For example, caries of chewing surfaces develops much more often on molars with a relatively long period of eruption (from 12 to 18 months) - compared to premolars, which erupt within only a few months.
Caries of the chewing surfaces of molars, as a rule, begins to develop during eruption as a result of conditions favorable for the accumulation of plaque. In a study in which children with erupting molars were taught proper dental care and had their teeth professionally cleaned for three years, the incidence of dental fillings was significantly lower. The authors concluded that “professional care of erupting teeth has long-lasting effects on chewing surfaces.” Their results suggest that temporary protection of partially exposed surfaces will also have a good effect.
Preliminary fissure sealing: controlling the risk of caries development in erupting permanent molars
Hyatt first suggested the need to protect emerging teeth from caries on chewing surfaces in 1923. He suggested coating the chewing surfaces of erupting teeth with zinc phosphate cement as early as possible.
However, he also suggested placing Class I amalgam as soon as the teeth have erupted sufficiently to prevent the development of fissure caries. Fortunately, his technique did not gain popularity, even though the issue of eliminating enamel fissures was once again raised by Bodecker in 1929.
It is currently believed that to prevent the development of caries, it is important to engage in prevention from the beginning of the eruption of the first permanent tooth.
The immature enamel surface remains vulnerable to carious processes for a relatively long time - until tooth eruption is completed.
There are few measures that can be taken during this time to reduce the risk of tooth decay. Among them:
1. Brushing your teeth twice a day with fluoride toothpaste and a soft toothbrush to remove plaque from the chewing surfaces of your teeth.
2. Daily rinsing with a 0.2% fluoride solution will reduce the risk of developing caries in the future. In addition, you need to review your child’s diet and reduce the amount of sugar consumed. However, the main risk factor that should be remembered is the fact that the enamel under the shell, due to difficulties in accessing it, cannot be properly cleaned - neither by the child himself nor by those who care for him.
Since it is impossible to isolate a partially erupted tooth from saliva, the only material that can be used for this purpose is a fast-curing fluoride-releasing glass ionomer cement. It is insensitive to humidity, and, moreover, can release additional amounts of fluoride, the reserves of which, in turn, can be replenished with the help of fluoride-containing toothpastes and rinses. After the tooth has erupted, the need for long-term sealant placement may be reconsidered.
The procedure for applying glass ionomer cement under the shell is called “fissure pre-sealing” and is intended to provide protection to the permanent molar for the entire period of eruption. An alternative to this procedure is regular visits to the dentist and repeated applications of fluoride-containing products, which is more expensive and requires more effort from the patient.
The treated tooth can be seen in Figure 3.
The treatment used a fast-hardening (90 sec.), increased fluidity, and high fluorine release glass ionomer. It is pink in color, so the treated surface is easily identified, and it also serves as a marker for a temporary treatment method. After tooth eruption is completed, a decision is made on the need for further treatment.
Sealing protocol
The area should be isolated using cotton swabs and a high-yield saliva ejector. Foreign bodies are carefully removed from under the shell. The tooth surface is treated with conditioner using a microbrush. Glass ionomer cement is applied to all exposed surfaces of the erupting tooth, as well as to the space under the shell. Now it will remain in place until the tooth has fully erupted. Excess material will be removed when brushing your teeth after implantation.
Sealing proximal surfaces: a new technique
The methodology was based on the proposal to protect caries-prone surfaces by sealing accessible surfaces.
The high effectiveness of sealants in preventing caries of pits and fissures has been proven in randomized clinical trials and analysis of the ratio of treatment costs and results obtained.
However, the effectiveness of these measures in preventing the development of caries at the spot stage has not been studied. Of all the surfaces of the teeth, the proximal surfaces have the highest risk of developing caries because, due to the presence of contact areas, plaque accumulates on them and is difficult to reach with a toothbrush; Hygiene can only be achieved with dental floss.
In high-risk children, white spots on the proximal surfaces are visually detected approximately 12 to 18 months after the establishment of posterior tooth contacts.
Traditional methods of preventing the development of stains on proximal surfaces, such as flossing or rinsing with a fluoride solution, are not always effective, since they largely depend on the patient's willingness to perform the necessary measures.
More often, the treatment of proximal caries concentrates on isolating caries at the initial stage using low-viscosity composites. Although the method is quite effective, it requires access to the proximal surfaces of the tooth, which in turn requires tooth separation.
An alternative method is to coat the tooth with sealant before the contact surfaces with adjacent teeth are established. The eruption of primary and permanent teeth occurs in several stages, between which it is possible to gain free access to the proximal surfaces of the posterior teeth.
Sealing protocol
The opportunity to protect the proximal surfaces of the first molars appears at the end of the tooth change period. As described below, the premolars are already fully erupted but relatively easily accessible from all proximal surfaces.
The white spot formed at a time when the primary molar had not yet fallen out. A rubber gasket was applied, then the exposed surfaces were cleaned using an abrasive strip. A 20-second application of 37% phosphoric acid was made to the proximal surfaces, after which they were washed and dried with a three-function gun.
A wear-resistant nanocomposite sealant was applied and light-cured. It is important to ensure that there is no excess material left after placing the sealant.
Conclusion
In this article, we expanded the traditional technique of using sealants and proposed a technique for pre-sealing fissures and proximal surfaces of molars in the “window of accessibility” that appears between partial tooth eruption and the establishment of contacts with adjacent teeth.
Together with established prevention techniques such as fluoride applications, the new sealant application technique will contribute to reducing the incidence of dental caries in children. Sealants should be part of an overall prevention strategy that includes both population-based and individual risk assessment.
Darkening of the fissures of baby teeth
Why are children especially susceptible to fissure caries?
- The enamel of newly emerging primary and molar teeth has not yet been fully mineralized and is not strong enough.
- Children do not practice oral hygiene very carefully.
The lower molars are at risk - they are the first of all permanent teeth to erupt. Since they do not have antagonists (paired teeth on the other jaw), self-cleaning does not occur during chewing - the lower crowns do not contact the upper ones.
Parents are advised to pay special attention to caries prevention and regularly visit the pediatric dentist from the moment the child's first tooth emerges. Even if caries affects a baby tooth, it should not be left untreated. It has been proven that the disease can affect the rudiments of molars.