Sometimes the pain that occurs after recently treated pulpitis is a natural phenomenon, but it may also be that the cause of the pain is mistakes made by the dentist. Statistics are not on the side of dentists: according to it, in approximately 60% of cases, treatment of pulpitis is carried out with gross violations, leading to not the most pleasant consequences.
To avoid problems in the future, after treatment it is necessary to take an x-ray: from the image it will be possible to immediately determine whether the doctor filled the root canals properly. But, again, according to statistics, in more than half of the cases, doctors, seeing the shortcomings of their own work, do nothing, and the absolute majority of patients do not know how to read x-rays. Why does this happen? Firstly , treating pulpitis is a troublesome and lengthy task, and secondly , errors will not manifest themselves immediately, but only towards the end of the treatment guarantee, when the patient will no longer have the right to make claims.
Tooth hurts after pulpitis treatment due to injured tissue near the root
The first stage of treatment for pulpitis is the removal of the inflamed pulp, after which the canals are sealed so that subsequently the inflammatory process does not begin to develop in them again. During the procedure, minor tissue trauma occurs, which simply cannot be avoided.
Pain may occur due to:
- separation of a bundle of nerves located near the upper part of the root, which often occurs when removing pulp;
- mechanical treatment of the canals with special tools (very often the tool can extend beyond the canal, causing injury to the tissues located near the apex of the tooth root);
- penetration of antiseptic agents used to flush the canals outside of them, which can cause irritation.
In all of the above cases, pain is a natural reaction of the body. After proper treatment, pain will stop within a maximum of 3 days.
Acute pulpitis
- Focal
Pulpitis, in which inflammation affects only part of the pulp; manifested by severe paroxysmal pain every 5-7 hours for 10-15 minutes; the patient can pinpoint the tooth that is the source of the pain.
- Diffuse
Pulpitis, in which inflammation covers the entire pulp; attacks of pain last up to one hour, and sometimes longer; the pain radiates to neighboring teeth and gradually covers the entire jaw and head.
- Purulent
With this form of the disease, irreversible dissolution of the pulp tissue occurs, the pain becomes unbearable; A characteristic sign of purulent pulpitis is dulling of pain when exposed to cold, so the patient often spends time waiting for a doctor with a bottle of cold water applied to his cheek.
- Traumatic
Occurs after trauma to the jaw, after treatment or fracture of a tooth, when the pulp is exposed and causes acute pain when breathing, touching and at rest.
A tooth hurts due to a poorly filled canal
A feeling of pain and swelling of the gums are the first signs that the tooth treatment was performed poorly. However, there are situations when the inflammatory process develops slowly, and it is possible to understand that something is wrong with the tooth only by taking a picture.
As mentioned above, filling canals is a common procedure, often performed with errors: if they are not corrected, then after some time inflammation and, consequently, pain will begin.
There are the following options for unsatisfactory filling:
- The canal was not sealed to the entire length of the root. The pulp becomes inflamed due to microorganisms that have entered it. After its removal and thorough treatment of the canal with drugs, some part of the microflora still remains. When the canal is not filled along its entire length or the filling material is not compacted tightly, the infection multiplies and affects the tissue surrounding the tooth. Eventually, a sac filled with pus appears at the apex of the root. If the doctor has not completely filled the canal, then the tooth must be re-treated (the sooner this is done, the greater the chances of saving it). Usually, a complete unfilling of the canal and its re-sealing is required. When the canal is unsealed only in the area of the upper part of the root, the doctor can perform a resection, which allows the canal not to be unsealed.
- Exit of filling material beyond the root apex. One of the causes of pain is the removal of the material used for filling beyond the upper part of the root. There is no universal method for eliminating the deficiency: a preliminary examination by a doctor is required. If little material has been removed, the pain will subside over time (in some cases you will have to wait up to 2 months). In this case, the patient is given a choice: either tolerate a slight reduction in pain, or agree to re-treat the tooth. If a lot of material has been removed, surgical intervention will be required: the doctor will make a small hole in the bone through which he can remove excess material (a simple operation takes about half an hour).
- Leaving a broken part of a medical instrument in the canal. When processing the canal, the instruments used by the doctor may break off. There may be several reasons for this: careless actions of the dentist; curved channels. Sometimes it is possible to get a fragment out, but if a piece of the instrument remains in the upper third of the root, it becomes very difficult to remove it. The broken part does not allow filling the entire length of the canal. There is a risk of infection multiplying, which can provoke the development of an inflammatory process in the tissues surrounding the tooth.
- Root perforation. Perforation is a small hole that appears in the root either due to natural causes (excessive curvature of the canals, but this happens rarely), or due to the actions of a doctor. Today, perforation is a very intractable problem in dentistry. Most often, perforation occurs when a pin is installed, when it is not fixed in the canal, but is brought out through its wall directly into the bone. If the canal is very curved or difficult to navigate, then working in it requires great precision from the doctor. But even extreme accuracy does not guarantee that mistakes will be avoided. Often, high-quality treatment of curved canals becomes a difficult task for an experienced doctor.
Perforation can be corrected, but it is difficult to do. To properly close the hole, expensive materials like Pro Root MTA are used. Sometimes filling with this material can be done from the inside of the tooth, sometimes surgical access to the area where the perforation has occurred is required. If the doctor is to blame for its appearance, then the hospital must correct the shortcomings at its own expense.
Consequences of pulpitis
Consequences of pulpitis
The biggest mistake that some patients make when experiencing toothaches is the desire to endure them, drowning them out with painkillers. This often leads to the development of dangerous complications of pulpitis, acute or chronic periodontitis. In addition to unbearable throbbing pain, high body temperature and complete loss of ability to work are added. Seeing a doctor at this stage of the disease is accompanied by increased psychological and physical discomfort for the patient, and after treating the tooth cavity, where the pulp was previously located, purulent contents with an unpleasant odor come out.
When periodontitis that arises against the background of pulpitis enters the chronic stage, fistulas with purulent contents form on the gums. This stage of the disease is considered the most dangerous to human health. Patients who have passed this stage remember for the rest of their lives the terrible picture of hanging “pus pockets” from their newly extracted teeth. Whenever at this moment it becomes clear that sometimes it is better to prevent than to treat. However, complications of pulpitis can lead not only to tooth loss, but sometimes serious diseases develop that threaten the patient’s life: phlegmon, abscess and sepsis.
Phlegmon leads to the fact that the patient’s general well-being sharply deteriorates, body temperature rises to a critical level, the shape of the face is distorted, and in addition to pain, a feeling of fullness in the jaw occurs. Sepsis is a blood poisoning and the most dangerous complication of untreated pulpitis, in which death cannot be ruled out.
Are you still wondering whether to see a dentist?
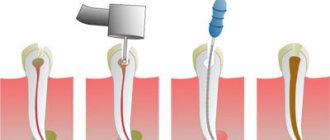
How is canal filling performed?
High-quality filling is the key to the absence of complications in the future. Before filling, the canals must be prepared: widen them slightly and ensure patency along the entire length.
Preparation consists of the following steps:
- elimination of tissues on which carious formations have appeared (removal of healthy tissue is allowed in order to gain access to the orifices);
- complete removal of the pulp;
- correct determination of the channel length (they are different in length);
- high-quality mechanical processing (includes expanding the diameter of the channel along the entire length);
- filling with gutta-percha.
The quality of the filling depends on:
- Correct determination of the channel length. In case of a dentist’s mistake, the canal may be either underfilled, which subsequently leads to the formation of cysts, or overfilled when the material extends beyond the boundaries of the root (consequences - pain, inflammation).
- High quality machining. The purpose of the procedure is to widen the canal so that it can be filled with filling material to its full length. Treatment can be carried out either using hand instruments, which the doctor rotates in the canal with his fingers, or using an endodontic tip (rotating in the canal, they remove a thin layer from the walls, gradually expanding it). This option is the most preferable, since the quality of processing increases and safety increases (the tip cannot break off due to automatic control of the load level).
- The chosen filling method and the doctor’s competence.
The patient can understand without the help of a doctor how well the canal was filled. To do this, you need to carefully look at the x-ray:
- The filling material will appear as a rich white color. This color should fill the channel throughout its entire length;
- in a properly sealed canal there should be no voids or gaps.
Symptoms
Inflammation of the pulp is not difficult to differentiate already at the stage of examining the oral cavity and interviewing the patient. This disease is characterized by:
- sudden onset of pain and its intensification at night;
- a gradual increase in pain intensity and duration in the first 3-5 days from the onset of the disease;
- irradiation (spread) of pain to the ear, eye, chin, depending on the location of the diseased tooth.
A characteristic feature of pulpitis, which makes it possible to distinguish it from caries and other dental pathologies, is a sporadic increase in pain, which is not associated with thermal, mechanical or other effects on the tooth.
Brief conclusions
The main consequences of poor treatment of pulpitis are as follows:
- flux, formation of cysts in cases where the canals are not completely filled, periodontitis;
- prolonged pain and neuralgia during repeated canal filling.
One of the most unpleasant consequences for the patient is tooth extraction. It cannot be avoided if:
- the doctor during the treatment broke the root or caused a perforation, which was not eliminated as soon as possible;
- A periodontal abscess formed at the root apex, and the patient delayed its treatment.
How does pulpitis occur?
The occurrence of pulpitis
It is generally accepted that caries, especially in an advanced stage, is the most common cause of pulpitis. However, the development of the disease can also be a consequence of tooth trauma, and a consequence of improper treatment by an unqualified dentist.
There are several ways of infection of the pulp and, as a consequence, the occurrence of pulpitis:
- through the crown of the tooth, when the carious cavity grows, becoming a gateway for the penetration of microbes and pathogenic bacteria into the dentin and further into the pulp;
- through the apex of the tooth root (retrograde pulpitis).
Due to its specific pathogenesis, retrograde pulpitis is a rather rare occurrence. The following factors can provoke it:
- infection of the pulp through the blood in systemic viral diseases such as rubella or herpes;
- infection of tooth roots through the maxillary sinuses during sinusitis.
At the same time, one of the most common causes of pulpitis are dental errors:
- a poorly treated carious cavity is untreated caries, which leads to re-infection of dentin and the development of caries already under the filling;
- thermal burn of the pulp due to insufficient water cooling or overdrying of the tooth cavity during treatment;
- chemical damage to tooth tissue during treatment.
! You can protect yourself from the consequences of treatment by an unscrupulous dentist in advance by contacting a well-known dental clinic with a name and reputation. High-tech equipment, the availability of modern equipment and a staff of professional dentists will allow you to undergo a full diagnosis and receive timely, qualified treatment.
When there is no need to see a doctor
Why does a tooth hurt after pulpitis? The appearance of pain is due to the increased trauma of the entire procedure, which consists of opening the tooth, removing pulp from the root canal and filling the empty space with artificial material - a filling.
How long does a tooth hurt after pulpitis in normal condition? Without pathologies, the pain persists for 5-10 days, and it gradually subsides. It is considered normal when:
- after pulpitis, the tooth hurts without increasing pain;
- there is no bleeding, swelling, swelling or redness, general weakness, or fever.