Neuritis
is an inflammation of the peripheral nerve trunk.
The peripheral nervous system refers to the nerve structures outside the brain and spinal cord (which are in turn called the central nervous system). Excitation (signal) is transmitted along the nerves, allowing the central nervous system to receive information about the state of all organs and systems of our body and control muscle contractions. The tissues of various organs are penetrated by nerve endings, which are connected to the brain, and in most cases to the spinal cord using bundles of nerve fibers enclosed in a sheath of connective tissue. Such bundles are called nerves, and large nerves are called nerve trunks.
With neuritis, nervous tissue is involved in the inflammatory process. This leads to the fact that the signal in some part of the nerve passes worse or does not pass at all. Accordingly, the sensitivity of any area may be lost and the mobility of the muscles innervated by the affected nerve may decrease.
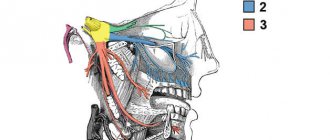
Trigeminal and facial neuralgia
Neuralgia is a disease in which damage or compression of the trigeminal nerve and/or its branches occurs. This causes a sharp piercing pain that occurs suddenly and brings physical and psychological discomfort to the patient. Despite the fact that the term “neuralgia” can be literally translated as “nerve pain,” the matter is not limited to pain. Trigeminal and facial neuralgia are radically different in symptoms. The facial nerve contains mostly motor fibers, so neuralgia leads to dysfunction of the facial muscles (the degree depends on the severity of the disease), and can also cause lacrimation, dry eyes and partial loss of taste. Pain in facial neuralgia is usually concentrated in the area of the parotid gland (the patient complains that the pain radiates to the ear), but there may be no pain at all. It is because of the lack of pain that some experts use the term “neuropathy” when talking about damage to the facial nerve. With the trigeminal nerve it’s exactly the opposite, since it contains many sensory fibers.
Neuropathic pain: causes and symptoms
Contents Causes of occurrence
Component or disease
Stages of pain
Nerve restoration after damage
Neuropathic pain is a companion to many diseases. The cause of its appearance may be damage to various parts of the nervous system.
Such damage affects very different levels: from small nerves located deep in the tissues, to nerve trunks, plexuses, and even individual sections of the spinal cord and brain. Since a person is riddled with nerves, damage to them at any level and site can lead to neuropathic pain.
If you've ever bumped your elbow or had a dentist hit a nerve with a drill while working on your teeth, you understand what neuropathic pain is. People with chronic neuropathic pain experience this feeling on a daily basis. At the first manifestations, patients describe this pain as discomfort, burning, “shooting”.
Causes
Neuropathic pain can be caused by a variety of factors, including fractures, metabolic disorders, and nerve damage during surgery. It can also be caused by a stroke, limb amputation, or spinal cord injury.
Neuropathic pain results from disruption of nerve structure and function. And it’s worth mentioning separately about nerve compression, for example, when a benign neoplasm puts pressure on the walls of nearby organs and brings pain due to overstretching of these walls.
Neuropathic pain: stages of development and diagnosis How to determine the cause of neuropathic pain and in what cases it can be treated
Component or disease
Neuropathic can occur as an independent disease or accompany other diseases, for example, diabetes mellitus or coronary heart disease - then doctors talk about the neuropathic component.
Several types of pain can occur simultaneously. For example, neuropathic and nociceptiveXnociceptiveNociceptive pain is a medical term used to describe pain from physical injury. For example, this is pain from an injury or during a dental procedure. Most often, people experience nociceptive pain. It goes away when the affected part of the body recovers. * together.
If a person breaks his arm, events can develop according to different scenarios. The first case, when a fracture occurs and a sprain of muscles and ligaments occurs nearby, the person feels only typical nociceptive pain, which he describes as sharp, aching and throbbing. Another case is when, during a fracture, the nerve bundle is stretched or the nerve is torn.
Even when the bone heals and the person has no external reasons to worry, he may experience pain from this damaged nerve. If the area of damage was large, it is likely that the nerve will remain damaged forever and the person will deal with chronic neuropathic pain.
Pain terminologyWe explain the main terms and definitions in the topic of pain syndrome
Stages of pain
With damage to the nervous system, pain develops quite slowly and gradually. Typical situation –
the appearance of tunnel syndrome: nerves are compressed in narrow places by tendons, muscles or other structures located nearby. This can happen on the neck, arms, legs due to awkward posture, tight shoes or clothing. Carpal tunnel syndrome often occurs in office workers who work in one position at a computer.
Pain relief by ambulance What to do if the ambulance refuses to go to a person with breakthrough pain
Editorial Board
Anesthesia
Another situation is nerve irritation due to a herniated intervertebral disc, which is usually accompanied by aseptic inflammation and edema. At this stage, the nerve is only irritated or slightly compressed, but these effects do not go unnoticed and can cause severe pain and discomfort.
the second stage occurs . The nerve is compressed so that it ceases to perform its functions. Numbness appears in the area of innervation of the compressed nerve, and the person’s surface sensitivity is impaired.
The third stage is loss of deep sensitivity. Muscle weakness appears; muscles innervated by damaged nerves refuse to work. As a result, muscle atrophy occurs.
You may have heard the phrase “the leg is withered” or “the arm is withered” - this, in fact, is muscle atrophy.
When a doctor observes a deficiency of nerve function in a patient, he understands that emergency release of this nerve is necessary - decompression. The longer a person goes without treatment, the less chance there is of restoring nerve function after decompression. And even if the doctor performs an excellent technical intervention, a person who has endured this pain for a long time may remain with it for life if the nerve is not restored.
“There is no need to endure pain” Branch manager of the First Moscow Hospice named after V.V.
Millionshchikova Arif Ibragimov about what patients should know about pain, painkillers and a pain diary Arif Ibragimov
Anesthesia
Nerve restoration after damage
The nervous system is a very delicate, delicate and complex structure. Its imbalance is quite easy to cause, and self-healing of this structure occurs slowly, if at all. The regenerative capacity of the nervous system is severely limited, and any damage to the nerves is difficult to treat.
Most often, doctors are faced with a situation where a complete cure is impossible, and we are talking only about controlling symptoms, in fact, adapting to neuropathic pain. In this case, the task is to ensure an acceptable quality of life for the person and relieve pain as much as possible so that the person can sleep, communicate, and lead a social life.
Damage to a nerve usually leads to its restructuring. Secondary changes occur around the site of damage itself, and then further and further affect the overlying parts of the nervous system. If this pain in the immediate focus of damage is not dealt with in the early period, then there is a very high risk that the changes will go higher and lead first to peripheral sensitization (a pathological process in the nervous tissue) and then to central sensitization with the formation of a certain level of excitation in the central sensory neurons . Because of this, weak painful and non-painful stimuli begin to be perceived by the brain as severe pain.
If the source of damage affects the structures of the brain, in fact, an autonomous, separate disease develops.
Patients are forced to take medications throughout their lives that affect the regulation of neurotransmitters in the brain. Patients with chronic neuropathic pain may lose 1 cm³ of cerebral cortex per year.
With neuropathic pain, there is a rapid growth of the lesion, and therefore, when the first symptoms appear, you need to consult a doctor, otherwise it is quite difficult to treat it later.
How to treat neuropathic pain Read the article by algologist Alexey Voloshin about the four main methods of treating neuropathic pain, as well as what targeted therapy and neuromodulation are
You might be interested in:
Chronic pain: causes and manifestations
Many people, including some doctors, think that chronic and acute pain differ only in duration: acute pain is a short-term condition, chronic pain is one that does not go away for a long time. Chronic and acute pain are similar in appearance, but they have different principles of origin. Algologist Andrei Danilov explains why chronic pain is difficult to treat.
Simple Ways to Reduce Chronic Pain
Algologist Andrey Danilov on how sleep, positive emotions and meditation affect the perception of pain.
Pain Relief Guide
Answers to the most common questions that arise from patients and their loved ones when prescribing strong analgesics
“Pain is determined by how the nervous system perceives damage.”
Neurologist Maxim Churyukanov on the biopsychosocial model of pain, features of pain scales and shortcomings of the medical education system
Pain and dementia
Why is it important to learn to recognize pain and not ignore it?
Reprinting material on the Internet is possible only if there is an active hyperlink to the original material on the website
Symptoms of neuralgia
- Facial pain (prosopalgia). A characteristic sign of neuralgia. Sharp and sudden, reminiscent of an electric shock. Usually lasts from 5 to 15 seconds, is paroxysmal in nature and can occur at any time. During periods of remission, the number of attacks decreases. Most often, pain occurs in the area of the cheekbones and lower jaw (both right and left), and can be localized in almost all areas of the face.
- Impaired sensitivity. A severe form of neuralgia can lead to partial or complete loss of sensitivity of the skin.
- Nervous tic of the eyelid (nystagmus), spasms and twitching of facial muscles.
- Loss of coordination and motor skills are rarer manifestations of severe forms of the disease.
- Headaches, fever, chills and weakness are syndromes caused by viruses and infections.
Symptoms of neuritis
The main symptoms of neuritis are:
Pain along the nerve
The most common symptom of neuritis is pain along the affected nerve. The pain, as a rule, is dull in nature and intensifies in the cold, with physical activity or uncomfortable body position.
Sensory impairment
Sensory loss in the area of the affected nerve is common. It can manifest itself in the form of numbness, tingling, or “pins and needles.”
Decreased muscle activity
There is a partial decrease in muscle strength (paresis), a decrease or loss of tendon reflexes, and in some cases, muscle paralysis (complete cessation of muscle activity).
Vegetative and trophic disorders
With neuritis, there may be such vegetative and trophic disorders as depigmentation of the skin, the acquisition of a bluish tint, local hair loss, increased sweating and dry skin, swelling.
Causes
Unlike neuritis, neuralgia is not an inflammatory disease. Fever, fever, swelling and other symptoms of the inflammatory process are not associated with this disease. However, if the trigeminal nerve is damaged due to neuritis, pain sensations that fit the description of neuralgia may well occur. To avoid confusion and differentiate the two pathologies, it is necessary to consider their etiology.
The cause of neuritis (like any other inflammatory disease) is viruses and infections that cause gradual destruction of the membrane and nerve trunk, and classical neuralgia in the vast majority of cases occurs due to mechanical effects on the nerve. Today, experts identify dozens of factors that provoke the development of the disease.
Main causes of neuralgia
- Head injuries leading to changes in the cranial structure and displacement of bones.
- Benign and malignant tumors that, as they grow, compress the trigeminal nerve.
- Various bite pathologies and other dental anomalies.
- Pathologies of the structure and diseases of blood vessels located in close proximity to the nerve (atherosclerosis, aneurysm, vasodilatation, etc.).
- Sinusitis and otitis in chronic form.
- Trigeminal neuralgia after tooth extraction. Occurs during a traumatic or incorrectly performed extraction procedure.
- Damage as a result of infection resulting from a number of diseases: periodontitis, periodontitis, stomatitis, herpes, syphilis.
Trigeminal neuralgia from hypothermia occurs rarely. However, this factor contributes to the development of the disease and complicates treatment. The same can be said about decreased immunity, metabolic disorders, neurosis, diabetes and other complicating factors.
Classification of the disease
Due to the occurrence
- Primary (idiopathic) trigeminal neuralgia. A classic type of neuralgia, so to speak. Occurs due to compression of the trigeminal nerve.
- Secondary trigeminal neuralgia is a consequence of other diseases and viruses.
By coverage
- Unilateral (one branch of the trigeminal nerve is affected).
- Bilateral (more than one branch is affected).
Neuralgia can affect the 1st, 2nd, 3rd branches of the trigeminal nerve. The first branch is responsible for the orbital zone, the second for the median zone (including the nose and upper lip), and the third for the lower jaw. Most often, damage to the third branch is diagnosed, so the pain affects the area of the lower jaw, and an attack often occurs during hygiene, eating or shaving.
Classification and diagnosis of pathology
Facial nerve injuries are divided into the following types:
- neuropraxia (cured in 3-5 weeks);
- axonotmesis (moderate nerve damage, requiring up to six months of therapeutic treatment);
- neurotmesis (irreversible changes in the structure of nerve fibers. Cannot be treated with medication. Surgical intervention is required).
This neurological pathology is diagnosed using two methods:
- mechanoceptive (brush test - the patient is carried out on the lip, and the patient says the direction of movement and irritation with two points - a device resembling a mathematical compass is applied to the lower part of the face. In this case, the distance between the legs of the device is constantly increasing. As soon as the patient stops feeling each injection separately, the result is recorded and the degree of nerve damage is determined);
- nociceptive (pin prick, temperature test).
Taste buds are tested by dipping a cotton swab in salty or sweet water.
Treatment
Pain in the area of the inferior branch of the trigeminal nerve requires the use of 3 treatment methods.
Drug therapy. The doctor prescribes blockers and painkillers to reduce symptoms. The dentist will also recommend anti-inflammatory therapy. This treatment usually lasts 5-7 days.
Removing the artificial root. 1-1.5 days after implantation of the rod (if symptoms occur), dentists recommend immediately removing the implant, since such a decision increases the chances of a favorable outcome of therapy. Further treatment is carried out with medication.
Surgical intervention. Indications for a radical method are considered to be the failure of removal of the implant and treatment with medications.
Important! Removing the implant is not always the key to successful treatment of the nerve, but this action increases the chances of a quick recovery and reduces the risk of tumor formation in the area of the nerve bundle.
Treatment tactics are agreed upon with the patient, who signs consent for the operation.
Predictions and prevention
| Click to sign up for a FREE consultation |
Neuropraxia and axonotmesis are quite treatable. Statistics show that more than half of patients completely cure the disease. With neurotmesis, complete recovery does not occur.
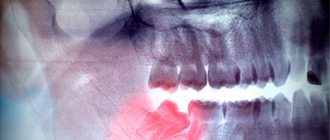
Dentists call the main preventive measure a comprehensive study of the performance of the dental system before implantation. At the diagnostic stage, the doctor finds out the exact location of the nerve. This helps to avoid injury to the “twig”.
An experienced dentist will definitely analyze CT and X-ray data, compare the results and draw up an implantation plan based on the individual structural features of the patient’s lower jaw.
The implant is screwed in carefully; its final position should be no closer than 2 mm to the nerve process.
Types of trigeminal neuralgia
There is an additional classification that can also be used in making a diagnosis.
Acute
Acute trigeminal neuralgia, accompanied by frequent and severe attacks.
Chronic
Chronic trigeminal neuralgia is a consequence of an untreated disease. The patient has been observed for a long time: remissions alternate with exacerbations.
Atypical
Atypical trigeminal neuralgia occurs against a background of stress and nervous exhaustion (psychosomatics).
Postherpetic
Postherpetic trigeminal neuralgia occurs after a history of herpes and its symptoms differ from the classic type. The pain is usually burning and may not go away for two to three hours.
Diagnosis of the disease
Modern medicine has in its arsenal many diagnostic techniques that make it possible to determine the type of neuralgia and the cause of its occurrence:
- visual examination and questioning of the patient;
- X-ray of the jaw;
- MRI of the brain and blood vessels;
- laboratory analysis of urine and blood;
- electromyography.
Diagnosis is carried out by a neurologist, but additional examinations by other specialists are often required: dentist, ophthalmologist, otolaryngologist. Particular attention is paid to differential diagnosis, since neuralgia may resemble other diseases in its symptoms, in particular glaucoma, otitis media, ethmoiditis, Slader syndrome, etc.
Causes and prevention of mandibular nerve injuries
The only cause of such damage is considered to be medical errors. Since in preparation for implantation, X-rays of the jaw are taken, which the doctor must carefully study so that when choosing an implant and a place for it, he does not injure the nerve, the injuries are caused by his unprofessionalism or negligence.
Damage to the mandibular nerve most often occurs when:
- improper administration of anesthesia - needle injury;
- choosing an implant that is too long;
- damage by an instrument - when preparing the site for the implant.
The only way to avoid such an injury is for a doctor to responsibly approach the stage of preparation for surgery, carefully studying the condition and structure of his patient’s jaw. The only way of prevention for the patient is to choose a trusted clinic and a highly qualified doctor. Specialists at the Implantmaster clinic have been able to reduce the number of injuries of this kind to 2%, since they carefully study three-dimensional photographs of a person’s jaw before implantation, and can correctly assess the condition of the bone tissue, the location of nerves and blood vessels, and select the optimal size of the implant.
Treatment of trigeminal neuralgia
Treatment and drugs
For successful treatment, complex drug therapy is used. First of all, these are anticonvulsants (carbamazepine, finlepsin or clonazepam), which are included in the mandatory rehabilitation program and relieve the main manifestations of neuralgia. The dosage and duration of treatment are determined strictly by the attending physician.
For additional effect, antihistamines and local pain relievers may be prescribed. To compensate for the lack of gamma-aminobutyric acid (a kind of mediator between the brain and the nervous system), baclofen, phenibut or gabapentin are prescribed. In the stage of exacerbation of neuralgia, specialists often prescribe antidepressants to eliminate psychological discomfort (the most common remedy is finlepsin). If the cause of the disease is a virus or infection, antiviral and antibacterial agents, as well as NSAIDs, are prescribed. During the recovery period, it is recommended to take B vitamins.
Physiotherapy
To eliminate pain, novocaine blockades and sodium hydroxybutyrate injections are actively used. The most popular and effective physiotherapeutic techniques: acupuncture, ultraphonophoresis, magnetic therapy, and low-frequency laser therapy. Massage for trigeminal neuralgia is also a good addition to general treatment and allows for better blood circulation.