Etiology and pathogenesis
The development of periostitis most often occurs with inflammatory diseases of the oral cavity and teeth, pulpitis and periodontitis. Also, the development of purulent inflammation of the periosteum can occur after jaw fractures, injuries and wounds of the soft tissues of the cheek, after treatment with anesthesia. Through damage to the dental tissue, gums or cheeks, the pathogen enters the jawbone, causing inflammation.
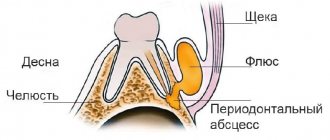
Acute periostitis can develop as a result of acute or chronic periodontitis, with suppuration of odontogenic cysts, and difficulty in teething. The process begins with the inner layer of the periosteum, gradually spreading to all other layers. Periostitis occurs when the focus of primary infection of the tooth canal or gum is blocked and its contents penetrate into the periosteum. The exudate penetrates through small holes in the alveolar plate through the channels.
Less commonly, flux develops in diseases of the pharynx (sore throat, pharyngitis, laryngotracheitis) or in the presence of a focus of infection in the body, from where it can be transferred to the periosteum with the blood or lymph flow.
When examining purulent contents during purulent periostitis, staphylococci (Staphylococcus aureus is one of the main causes of flux development), streptococci, various types of bacilli and putrefactive bacteria are often found.
Reference! 25% of all pathogenic microflora during flux are aerobic bacteria, the rest is anaerobic forms.
General factors influencing the development of the disease:
- weak immunity;
- hypothermia;
- stressful situations;
- poor oral hygiene;
- carious processes in teeth;
- old fillings;
- frequent medical interventions;
- bad habits.
Forms of periostitis
Depending on the cause of the flux and its course, we talk about its forms:
- Acute: simple – occurs as a result of a bruise of the face, with fractures and injuries of the jaw bones;
- purulent – penetration of periodontal infection to the periosteum;
- tuberculosis - when Koch's bacillus is carried into the periosteum and bone tuberculosis;
- syphilitic - as a complication of congenital or acquired syphilis.
- ossifying – chronic form with the development of compactions in the form of bone tissue;
Reason to see a doctor
If you were able to independently determine the cause of the gum swelling (an erupting tooth is visible, an injury is obvious, a tooth was recently removed, etc.) and it does not require the intervention of a doctor, you do not need to go to the clinic. But if the inflamed gum hurts for more than 3 days and there is no improvement in the condition, you should still consult a doctor.
If you have gum inflammation, you need to urgently go to the hospital in several cases:
- there was an unpleasant odor from the mouth and pus was found;
- not only the gums are swollen, but also the cheek;
- when you tilt your head to the painful side, you feel heaviness;
- there is a high temperature;
- swollen tissues are very different in color from healthy ones (white and yellow tumors indicate suppuration, and bluish and burgundy shades indicate blood stagnation);
- the pain seems to pulsate and is not relieved by analgesics.
Even in the absence of these symptoms, but if the cause of gum swelling is unknown, it is worth visiting a specialist. This will help avoid dangerous complications, as well as quickly alleviate the condition, relieve or reduce pain.
Clinical picture
The main symptom for all types of flux is severe toothache at the site of infection, sometimes diffuse (with extensive bone damage). Swelling gradually begins to increase: first it is localized above the site of inflammation, and then along the surrounding tissues, sometimes affecting the neck, temple and eye.
Important! Sometimes flux occurs painlessly or with a mild pain effect, which, as a rule, indicates the development of a chronic form with sluggish inflammation and periodic relapses.
Inflammation is accompanied by the following symptoms:
- pulsation at the site of the lesion;
- increase in body temperature to subfebrile and febrile levels;
- headache;
- enlarged lymph nodes on the affected side;
- weakness, lethargy, lack of appetite;
- pain when swallowing, talking, opening the mouth;
- pain when pressing on the gum;
- redness of the oral mucosa at the site of the lesion.
How to relieve pain and discomfort
- Do not touch the blood clot in the socket with your tongue, toothbrush, hands or foreign objects;
- make oral baths from herbal decoctions and antiseptic solutions;
- if the pain radiates to the ear or another part of the head, take a painkiller;
- exclude hot food and drinks.
If your gums hurt for several days after wisdom tooth removal or you have a headache, you don’t need to worry too much. Analgesics prescribed by your dentist will help you cope with these symptoms. If the discomfort does not go away after a week, painkillers do not help much - you need to go to the doctor. If the temperature is above 37.5℃, which does not decrease to normal, the development of an allergic reaction (to an analgesic, hemostatic sponge), or a sharp deterioration in health, you should consult a doctor immediately.
Therapy and rehabilitation
Treatment of the disease is carried out by two methods - conservative and surgical. The choice of method depends on the form of the disease, its severity, and the course of the disease. In the early stages of development of the pathological process, conservative treatment is possible by prescribing a complex of drugs:
- broad spectrum antibiotics
- anti-inflammatory;
- painkillers;
- antipyretic.
IMPORTANT! Conservative treatment requires careful compliance with all doctor’s instructions until the process is completely eliminated. Otherwise, there is a risk of the disease becoming chronic.
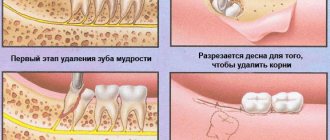
Purulent periostitis is treated by wide opening of the purulent sac with dissection of the periosteum to the bone. At the same time, the issue of treating the tooth that caused the inflammatory process is being resolved. Most often, such a tooth is removed. After removing the pus, medications are prescribed, including antibiotics, anti-inflammatory and painkillers. Additionally, physical therapy may be prescribed: UHF, microwaves. The patient is recommended to frequently rinse the mouth with a solution of baking soda or sage tincture.
Simple periostitis requires complete rest of the injured area and treatment with physiotherapeutic procedures. All other types are reduced to treating the underlying disease or eliminating the focus of fibrous tissue growth.
IMPORTANT! Under no circumstances should you treat flux yourself. It is especially not recommended to pierce a purulent sac: there is a high risk of infection in neighboring tissues.
To speed up the treatment and recovery processes, you can resort to traditional medicine methods.
During pregnancy
During pregnancy, women often experience problems with gums. This is due to the radical restructuring that occurs in the body.
Do you want to know what causes teeth grinding during sleep in adults and how to start treatment with folk remedies? Then you need to read the following article. And you can see the photos before and after biorevitalization from the article provided at the link. Here you will find a lot of useful information about this procedure.
Also, pathological conditions develop against the background of decreased immunity, lack of vitamins, and unbalanced nutrition.
Prevention
Flux is easier to prevent than to treat. Prevention methods are simple and known to almost everyone. They consist of timely treatment of carious teeth, timely removal of the gum hood from wisdom teeth, the correct choice of toothbrush and toothpaste, and timely replacement of oral hygiene products. It is recommended that you visit your dentist at least twice a year and have your teeth professionally deep cleaned to remove plaque at least once a year.
IMPORTANT! Don’t forget about strengthening your immune system and giving up bad habits.
Dental flux is an unpleasant disease that requires treatment by specialists at an early stage of development. Self-medication in case of periostitis is unacceptable. With a favorable course and initial stage of development, conservative treatment is possible, but most often they resort to the surgical method.
Pain after wisdom tooth removal
Patients are always interested in the question, how many days does the jaw hurt after wisdom tooth removal? Pain after surgery is a standard tissue response to injury. Normally, the pain subsides within a few hours or within 3 days after extraction (in case of complicated removal). The pain a patient experiences after wisdom tooth removal indicates the success of the procedure.
- The first discomfort and pain appear 2-3 hours
after the intervention (when the anesthetic wears off). - The first 3-4 days
there is aching pain, redness and swelling of the soft tissues. If the extraction is successful and the hole is properly cared for, the pain will gradually disappear. - Over the next 2 weeks
, if there are no complications, the wound will heal completely, and minor pain may occasionally occur in the late afternoon. - After 3 weeks,
all discomfort should disappear.
If a wisdom tooth has been pulled out and it hurts for more than 5 days, the intensity of the pain increases, it becomes throbbing, debilitating, accompanied by fever, swelling - this indicates a complication and requires immediate medical intervention.
What to rinse with?
To eliminate painful sensations, people are advised to rinse their mouths with special antiseptic solutions, for example:
- Chlorhexidine. The medicine is diluted in water in accordance with the recommendations specified in the instructions. Manipulations are carried out after brushing your teeth, no more than three times a day.
- Miramistin. The drug is able to eliminate pain and also destroy pathogenic microorganisms.
- Hydrogen peroxide.
Traditional methods
To eliminate painful sensations, people can use folk recipes, provided there are no contraindications and individual intolerance to the components included in them:
- Soda-salt solution. To prepare it, you need to pour a glass of water into a deep container, into which soda and salt (a teaspoon each) are poured. After thorough mixing, it should be used for rinsing. You can add a few drops of iodine to the soda-salt solution. Manipulations should be carried out every two hours.
- For mouth rinsing, it is recommended to use herbal infusions made from eucalyptus, calendula or sage.
- A good effect is achieved by using chamomile infusion. To prepare it, dry and crushed grass (1 tbsp) is poured into a deep container, which is poured with boiling water (1 l). The contents of the dish should be infused for 15 minutes, after which it is filtered. The collected liquid is used to rinse the mouth.
Why does the gum around the wisdom tooth hurt?
The inflammatory process in the area of the third molar is always accompanied by swelling and pain. This allows you to notice it immediately and begin treatment in a timely manner. Before giving prescriptions to the patient, the dentist finds out the cause of the disorder. This is necessary to eliminate the infectious focus and prevent relapse.
Radiography is used to make the correct diagnosis. In the image, the doctor sees what is happening to the tissues and how far the inflammation has gone.
The main reasons look like this:
- wisdom tooth coming out;
- pericoronitis developed;
- a carious process occurs in the cervix.
Pain due to wisdom tooth cutting
Eights can appear both at 20 and at 50. And each case is a variant of the norm. You can never predict when these units will decide to show up. You can understand that a wisdom tooth is growing by the following signs:
- increase in gum volume;
- compaction and redness of tissues;
- pain when touching the inflamed area.
It happens that a unit does not cut through for a very long time. This is possible when the volume of bone structures is too large, there is insufficient space to accommodate a volumetric crown, or the unit is in a dystopic position (then it grows to the side or at an angle).
Pericoronitis as a cause of pain
The tissue surrounding the third molar may become inflamed. Plaque actively accumulates in the hole through which the figure eight erupts. A so-called gingival hood is formed. It does not allow the unit to “pass” completely and is a suitable place for the growth of bacteria and the accumulation of food debris.
Dental neck caries
The third molar has the same structure as the rest of the oral cavity, so caries on its surface is not uncommon. Then he hurts himself or the gums near him ache.
Due to the peculiarities of the position of the unit, a person usually does not have the opportunity to examine the carious cavity. Therefore, you should visit the dentist's office. Neglected caries leads to pulpitis. Then the treatment will be much more difficult.
Other reasons
Less common causes of discomfort in the figure eight area include:
- burn of mucous membranes;
- mechanical damage to tissues;
- hormonal imbalances, long-term use of hormonal medications, thyroid diseases;
- wearing incorrectly selected or low-quality removable dentures;
- stomatitis;
- gingivitis.