Where is the trigeminal nerve located?
|
|
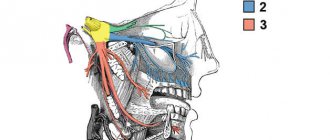
The photo below shows where the trigeminal nerve is located in humans and its exit points in great detail.
Anatomical structure
The character of TN is mixed. At the base of the brain structures, emerging from the thickness of the bridge with sensitive and motor roots, it is directed forward and slightly to the side, penetrating into the cleft of the dura mater. The sensitive root forms the trigeminal cavity, in which a fairly long ganglion (Gasserian ganglion) lies. The concave part is placed back, and the convex part is placed forward.
From the convex edge, which is located in front, there are three main branches: the ophthalmic, maxillary and non-maxillary nerves. On the inside, the node goes around the motor root, heading towards the cranial foramen ovale. There it reunites with the third branch of TN.
Branches of the trigeminal nerve
Trigeminal nerve: table
The photo above shows the areas of innervation of individual branches of the trigeminal nerve:
- first - n. ophthalmicus , supplies sensory fibers mainly to the forehead, upper eyelid and dorsum of the nose;
- second - n. maxillaris , innervates mainly the upper jaw;
- third - n. mandibularis - lower jaw.
All three branches of the trigeminal nerve, diverging, emerge from the ganglion Gasseri (Gasserian node). The latter is formed by the expansion of the nerve bundle of the sensitive portio major n. trigeminus and is located in a flat depression on the front surface of the petrous part of the pyramid, covered with dura mater. Then these branches n. trigeminus leave the base of the skull.
The first branch of the trigeminal nerve is the ophthalmic branch (ramus ophtalmicus)
The first branch of the trigeminal nerve - the ophthalmic nerve (ramus ophtalmicus) - runs along the lateral wall of the sinus cavernosus, under n. trochlearis and passes through fissura orbitalis superior.
Near the latter, it divides into three main branches:
- n. lacrymalis,
- n. frontalis,
- n. nasociliaris.
Lacrimal nerve - n. lacrimalis
N. lacrimalis is the smallest of these branches, serving mainly the skin at the lateral canthus and the conjunctiva of the lateral part of the upper eyelid and part of the lower eyelid.
Frontal nerve - n. frontalis
The largest branch is n. frontalis - passes as a continuation of the trunk under the arch of the orbit and above n. levator palpebrae super, and is divided into two branches:
- n. supratrochlearis,
- n. supraorbitalis.
The first innervates the skin in the medial corner of the eye and the conjunctiva of the medial part of the upper eyelid, forehead and crown, as well as the conjunctiva of the medial part of the upper eyelid together with n. supratrochlearis.
Nasociliary nerve - n. nasociliaris
N. nasociliaris turns just above the optic nerve medially to the orbital wall, passes through the foramen ethmoidae anterius and passes onto the ethmoid bone. Through one of the anterior openings of the ethmoid bone, it penetrates into the nasal cavity and ends with its branches on the mucous membrane and on the outer skin of the nose. N. nasociliaris innervates the tip of the nose and, like n. infratrochlearis, the skin in the medial corner of the eye, then the cornea, conjunctiva bulbi and the mucous membrane of the anterior upper part of the nasal cavity.
The second branch of the trigeminal nerve is the maxillary (ramus maxillaris)
Exit points of the trigeminal nerve (photo)
The maxillary branch (ramus maxillaris) is larger than the first and has purely sensory properties. It goes from the ganglion Gasseri through the foramen rotundum into the wing-shaped fossa, which it crosses in the direction of the canalis infraorbitalis. Through this channel it comes out as n. infraorbitalis through the hole of the same name and diverges with its endings along the face.
The most important branches of ramus maxillaris n. trigeminus:
- n. zygomaticus,
- n. infraorbitalis,
- n. sphenopalatinus.
Zygomatic nerve - n. zygomaticus
The first one is n. zygomaticus - supplies its both branches (n. zygomatico-temporalis and n. zygomatico-facialis), the skin of the anterior part of the temple and the area of the zygomatic bone with sensitive fibers; the second, in addition, is the conjunctiva of the lateral part of the lower eyelid.
Inferior orbital nerve - n. infraorbitalis
The second major branch is n. infraorbitalis - the skin of the wings of the nose, the lower eyelid, the front of the cheek and upper lip is supplied with sensitive fibers, as well as part of the conjunctiva of the lower eyelid and part of the upper eyelid. One of the terminal branches - labial (ramus labialis) - goes to the mucous membrane of the upper lip.
A significant part of n. infraorbitalis departs into canalis infraorbitalis and goes to the teeth of the upper jaw. This is nn. alveolares superiores, which branch in the teeth and gums of the upper jaw; in addition, some of them enter the mucous membrane of the maxillary cavity.
Pterygopalatine nerve - n. sphenopalatinum
The third branch of the second branch of the trigeminal nerve represents n. sphenopalatinum (pterygopalatine), which connects with the sympathetic node - pterygopalatine (ganglion sphenopalatinum). Sensitive branches of this node supply sensitive fibers to the mucous membrane of the maxillary cavity, hard and soft palate, periosteum of the teeth and gums of the upper jaw, and in addition to the tubal part of the pharynx together with n. glossopharyngeus.
In anesthesia of teeth and gums, both of these branches (n. infraorbitalis and n. sphenopalatinum) are very important.
The third branch of the trigeminal nerve is the mandibular (ramus mandibularis)
Table of innervation of the trigeminal nerve
The mandibular branch (ramus mandibularis) is the largest. It is formed from the third branch coming from the ganglion Gasseri, and from the portio minor of the trigeminal nerve. Ramus mandibularis leaves the cranial cavity through the foramen ovale and contains sensory and motor elements (see diagram above). Its main sensitive branches are as follows:
Auriculotemporal nerve - n. auriculotemporalis
N. auriculotemporalis. It supplies the skin of the anterior part of the auricle, temple and cheek with sensitive fibers, as well as the external auditory canal and part of the outer surface of the eardrum.
Buccal nerve - n. buccinatorius
The smaller branch is n. buccinatorius - goes to the skin of the corner of the mouth and to the mucous membrane of the cheek.
In addition to those described above, there are two more large terminal branches of ramus mandibularis:
- n. lingualis,
- n. mandibularis.
Lingual nerve - n. lingualis
N. lingualis passes behind musc. pterygoideus externus downwards, then protrudes between it and musc. pterygoideus externus and turns obliquely down and forward, to the floor of the oral cavity. It crosses the ductus submaxillaris (whartonianus), goes medially to the tongue and breaks up near the musc. genioglossus, onto its terminal branches. It supplies the surface of the gums of the front teeth facing the tongue with sensory fibers, the tongue up to the foramen caecum and part of the tonsils.
Mandibular nerve - n. mandibularis
The second large terminal branch is n. mandibularis, passes first together with n. lingualis and then directed through the foramen mandibulare into the canal of the lower jaw (see diagrams above). In the form n. mentalis, it comes out through the foramen mentale and supplies the skin of the lower lip and chin, as well as the mucous membrane of the lower lip, with sensitive fibers. During the passage of the trunk through the canal of the lower jaw, nn. alveolares inferiores to the lower teeth and gums. They are similar to nn. alveolares superiores.
From the article it became clear where the trigeminal nerve is located, and the innervation tables give an overview of the distribution of sensory fibers by area. The presented material will help not only students understand the anatomy and topography of the 5th pair of cranial nerves, but will also be useful to already established doctors, as it will refresh their knowledge.
Related medical articles
- Blood-brain barrier (BBB)
- Liquor system
- Spinal cord
- Cranial (cranial) nerves
Recovery and treatment
In the first case, self-recovery takes approximately 1 month; the help of doctors is not needed, since there is no anatomical damage. Symptoms of the second appear after a while - usually 6-8 weeks, so recovery can be painful and incomplete: it will take more than 2 months. In the third stage of damage to the mandibular nerve, treatment gives results only at the beginning and is performed surgically, since we are talking about degeneration with a violation of integrity. Loss of sensitivity, which is observed in a patient for more than 3 months, indicates a high probability of losing it forever. Damage to the mandibular nerve, the consequences of which is the lack of sensitivity of the nerve for a year, leads to irreversible changes. Only the professionalism and responsibility of the doctor, which is guaranteed by the specialists of our Implantmaster clinic, can protect the patient from such unpleasant injuries.
Author:
Types of diseases
All types of trigeminal nerve diseases can be divided into inflammatory and non-inflammatory.
Neuritis
An inflammatory disease of the trigeminal nerve that over time destroys the myelin sheath and nerve trunk. As a rule, inflammation of the trigeminal nerve is characterized by burning pain (sometimes accompanied by itching), impaired sensitivity and muscle atrophy.
Neuralgia
The disease trigeminal neuralgia is not inflammatory. It refers to any pain that occurs due to damage or pinching of the trigeminal nerve. Experts distinguish between primary (idiopathic) and secondary neuralgia. The causes of idiopathic neuralgia are usually difficult to determine, and secondary neuralgia is actually a manifestation of other pathologies. A characteristic feature of neuralgia is a sharp shooting pain, reminiscent of an electric shock and overtaking the patient suddenly.
Attention!!!
Gradenigo syndrome is also closely related to trigeminal neuralgia. It is characterized by abducens nerve palsy and can affect the functionality of the branches of the trigeminal nerve, pain and dysfunction of the eyeball. Some experts also distinguish damage to the nucleus of the trigeminal nerve and trismus - spasms of the masticatory muscles caused by pathologies of the trigeminal nerve.
Main functions
The trigeminal nerve is the most sensitive nerve in the face and mouth. It also contains motor tissues responsible for the innervation of the masticatory muscles. Has two sensors:
- The superficial nucleus of the trigeminal nerve, responsible for pain and tactile sensitivity.
- Deep nucleus (proprioceptive), responsible for the perception of free receptors.
Its motor part originates from the motor nucleus. Sensitive tissues are branched processes of neurons of the Gasserian ganglion. Nerve impulses depart from them to nerve cells embedded in the substance of the secreted part of the third brain, which continues the spinal cord.
The superficial nucleus is a continuation of sections of the spinal cord that look like horns. It runs through the medullary pons and bulb of the brain, and also covers the two upper cervical spinal segments.
The deep nucleus is located in the dorsal part of the pontine tegmentum. Receiving sensitive impulses from touch and pressure, it conducts them along the spinal cord through the posterior cords.
The motor nucleus is located in the middle of the deep nucleus. Its impulses exit near the sensory root, connecting with the mandibular nerve, innervating the facial and digastric muscles.
The layout and structure of the trigeminal nerve allows it to perform several important functions for the body:
- provide deep and superficial sensitivity of the eyes, mouth, nose, brain;
- responsible for the motor ability of the head muscles (temporal, chewing).
The trigeminal nerve perceives any touch, including pain, and transmits a sensory signal from the elements eaten or exhaled.
Alarms
The first signs of NAS damage are discomfort in the innervation zone (lower lip, cheek and gums in the lower jaw). There are 3 types of manifestations of the disease:
- anesthesia (absolute loss of sensation);
- dysesthesia (discomfort in the form of “pins and needles”, pain in the area of the affected NAS);
- paresthesia (decreased sensitivity: the patient does not feel pain when pricked with a needle).
Often, when removing figure eights, the lingual nerve is damaged. Sometimes this happens during implantation. Signs of the disease:
- uncontrolled tongue biting;
- violation of diction;
- decreased performance of taste buds;
- increased salivation.
Note: up to 90% of lingual nerve injuries do not require drug treatment. The pathology disappears on its own after 1.5-2 months.
Diagnosis and prevention of pathologies
When alarming symptoms appear, the doctor collects anamnesis, listens to the patient’s complaints, and conducts a visual examination. Next, he probes the exit points of the trigeminal nerve branches, assessing the degree of their sensitivity and pain. If triggers are identified, a preliminary diagnosis is made, which is confirmed using computed tomography and magnetic resonance imaging. These examinations make it possible to exclude the presence of other pathologies, as well as to detect vascular compression of the trigeminal nerve roots.
There are no specific preventive measures for trigeminal nerve diseases. Experts advise strengthening the immune system, treating infectious diseases in a timely manner, and not overcooling, especially in the summer, sitting under fans and air conditioners.