What is special about parapulpal pins?
Pins are special rod structures that are inserted not into the root canals, but into the dentin to fix the composite material (filling). Made from:
- titanium;
- of stainless steel;
- gold alloys;
- metals with polymer coating.
The use of parapulp pins in dentistry allows us to solve the problem of restoring a tooth with significant defects in hard tissue. Pins relieve the patient of the need to use orthopedic structures, since they provide reliable fixation of the filling and are able to withstand large and prolonged loads on the teeth.
What complications can there be?
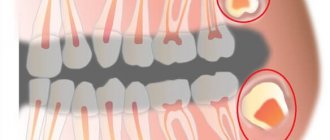
Restoration using parapulp pins is a standard procedure in dentistry, and the technique of placing pins has long been worked out by specialists down to the smallest nuances. However, in rare cases, mistakes on the part of the doctor can lead to unpleasant consequences - let’s look at them in more detail:
- Damage to periodontal tissue – periodontal perforation usually leads to an aesthetic problem in which the root area turns red and sag, exposing the neck of the tooth. The defect can be corrected by filling the canal with phosphate cement or amalgam. Another option: insert a pin into the canal at the level of the hole and seal it again,
- breakage of the rod or drill - such a nuisance can happen when bending the drill or the pin itself. To avoid such a problem, the instrument and rod must be inserted into the canal and removed as carefully as possible, without sudden rotational movements,
- difficulties when working with a drill - the tool may be dull or the specialist may choose the wrong direction of movement. Another option is that the drill rests on the enamel, which also creates difficulties with sawing fabrics,
- excessive channel width that does not correspond to the diameter of the structure - to solve this problem, you can resort to using a cementing composition.
To assess the quality of the work done, after about 6 months it is worth taking an x-ray and showing it to the doctor. The specialist will assess the condition of the restored element under operating conditions and will be able to promptly notice signs of complications, if any.
In what cases is it recommended to install pins?
Indications for the use of anchor pins are tooth destruction of varying degrees of complexity: from simple chips to almost completely lost volume of the tooth surface. Pins are installed when:
- destruction of the crown of the front tooth. The incisors and canines bear a huge load when biting; the corner or cutting edge of the tooth often breaks off;
- the destructive consequences of caries, when the enamel surface is severely damaged and holes appear in the chewing elements;
- consequences of injury, when one or more teeth have lost their integrity.
A prerequisite for the use of a titanium pin is an acceptable layer of dentin between the root and the gum. When the bone tissue is thinning, reliable fixation of the metal rod is impossible, so bone augmentation may be recommended. During extension, the membrane is also fixed with miniature titanium pins.
Titanium pins as a simple method for preserving the interdental gingival papilla
Authors: Jacopo Castelnuovo DDS, MSD Affiliate Assistant Professor, Graduate Prosthodontics, University of Washington, School of Dentistry, Seattle, Washington; Private Practice, Rome, Italy A. Burcin Sonmez DDS, MSc Resident, PhD Program, Department of Oral and Maxillofacial Sciences, University of Rome-La Sapienza, School of Dentistry, Rome, Italy; Private Practice, Rome, Italy John C. Kois DMD, MSD Director, Kois Center, Seattle, Washington Source: - Journal Compendium Continuing Education in Dentistry, September 2014, Volume 35, Issue 8. Translation: Bogoyavlenskaya Anastasia Valerievna - resident doctor of the department modern technologies of prosthetics of the Central Scientific Research Institute and Maxillofacial Surgery of the Ministry of Health of the Russian Federation. Ukhanov M.M. — junior researcher TsNIIS and maxillofacial surgery.
The aesthetic appearance of a natural or restored smile is the result of the balance that exists between the gingival and dental components [1-3]. In a healthy oral cavity, which is the most aesthetically pleasing, the relationship between these two components includes gingival projections or branches between adjacent teeth. These projections, the interdental papillae, give the scalloped appearance to the gingival component. In healthy periodontium, when the distance from the apex of the bone ridge to the contact point between adjacent teeth is 4 mm or less, and the interproximal distance between adjacent roots is 2 mm or less, the apex of the interdental papillae completely fills the interdental space [4].
On the contrary, the absence of interdental papillae in a smile may indicate a pathological condition and lead to the formation of “black triangles” or “black holes” between the teeth [5]. Interdental black triangles not only spoil the smile, but also cause discomfort to the patient, causing food retention and bacterial plaque in the interdental spaces; changes in speech associated with the passage of air through the interdental spaces and/or the passage of saliva during a conversation.
The gingival margin and interdental papilla do not have a specific shape, but repeat the shape and configuration of the underlying bone. Therefore, in order to have a scalloped gum shape (presence of interdental papillae), it is necessary to have a corresponding shape of the underlying bone, due to the presence of interdental bony apexes. In the presence of periodontal pathology or as a result of dental intervention, the bone tissue atrophies, losing the arched shape of the contour, flattens and recedes - the marginal gum also flattens and recedes, losing interdental scalloping and, consequently, papillae. As a result, the teeth appear longer, part of the root is uncovered, and the presence of “black triangles” is clearly visible.
The main deciding factor in the level of interdental papilla height is the underlying bone ridge (interdental bone peaks) [4,6-8], which plays a fundamental role [9,10]. Thus, it is extremely important to exclude iatrogenic resorption of the interdental bony apexes. Interdental bone resorption can occur as a result of procedures such as: tooth extraction (single or multiple), replacement of missing teeth with implants (single or multiple), periodontal surgery and also uncontrolled stages of restoration (for example, tooth preparation) that cause a violation of the biological width.
PARADIGM SHIFT Successful replacement of a missing tooth with a titanium implant became possible due to the high biocompatibility of titanium and its alloys with bone tissue. A few weeks after surgery, the bone-metal interface matures, leading to a process referred to as osseointegration [19,20], providing stability to the implant, which can then be restored with a crown. Installing implants in the jaws of patients with complete or partial edentia not only allows you to create artificial teeth fixed in the bone, but also avoids further resorption of bone tissue over time at the site where they were placed, even if the implant is not loaded. A retrospective, clinical, split-mouth study showed that bone-embedded, unloaded implants experienced less bone loss than adjacent functional implants over a 12-year period [21]. Well-functioning, unloaded implants can usually be observed in patients with maxillofacial prostheses retained by extraoral implants; a high service life of such structures is noted [22,23]. These important characteristics of commercial pure (CP) titanium, its alloys, and other biocompatible materials (eg, zirconium) can be used to prevent bone resorption of the interdental apexes.
EQUIPMENT AND TECHNIQUES The Titanium Reinforced Interdental Apex (TRIP) technique requires the surgical placement of rods made from any biocompatible material, such as titanium (pure or alloy), within the thickness of the interdental bone. Ideally, pin placement should be performed prior to any dental procedure that may result in resorption of interdental bone apexes (eg tooth extraction, implantation, periodontal surgery). After osseointegration of the biocompatible rod, the original height of the interdental bone apexes is maintained over time. Once the osseointegration process of the pin is complete, planned dental procedures such as tooth extraction and implant placement can be performed, with a reduced risk of interdental bone resorption and subsequent papillary atrophy. Depending on the clinical situation, it is possible to perform the integration of the safety pins immediately before the planned manipulation. The size of the biocompatible pins may vary depending on the size of the interdental bone apexes present. The prototype has the following dimensions: 0.5 mm width x 1 mm height x 5 mm length, these values can always be changed depending on the indications. Equipment for performing surgical pin integration includes: piezosurgical unit or sonic tips and calibrated tips; tester with dimensions corresponding to the pins, to check the volume of osteotomy during surgery; biocompatible pins; chisel for deep penetration and primary stabilization of the pin; surgical hammer, and collagen absorbable membranes to bridge the bone graft over the osteotomy.
INDICATIONS This technique can be used in clinical situations both before and after tooth extraction. There are four main indications: 1) Preservation of interdental bone apexes between several ovoids of a bridge (before removal). After tooth extraction (Fig. 1a), a bone crest defect occurs with a frequency of 91% [24]. The defect can be combined vertically and horizontally (55.8%), horizontally (2.9%), and vertically (32.8%). Thus, routine tooth extraction may cause flattening of the bone ridge with resorption of interdental bone (Fig. 1b). After the final fixation of the bridge with several ovoids, resorption of the interdental bone apexes occurs, forming black triangles (Fig. 1c). Biocompatible pins, using the TRIP system, are surgically inserted into the bone apexes before tooth extraction (Fig. 1e). Tooth extraction is performed either upon completion of the pin osseointegration process, or during the same visit (immediate protocol). Biocompatible rods should prevent resorption of interdental bone apexes, similar to titanium root-shaped implants (Fig. 1e). After fixation of the bridge, maintaining high interdental peaks will prevent the formation of black triangles due to the presence of papillae (Fig. 1f).
Rice. 1. TRIP system and multiple ovoid intermediate parts: a-c: tooth extraction leads to resorption of the interproximal bone and the formation of a black triangle. d-f: the introduction of biocompatible pins before removal preserves the interdental bone and papillae. 2) Preservation of interdental bone apexes between adjacent implants (before removal): When replacing extracted teeth with implants, along with the loss of bone tissue caused by extraction (deformation of the alveolar process), additional loss of bone tissue occurs as a result of implant installation (Fig. 2 a and b ). Around each implant, as a rule, about 1.5 mm of the lateral component of bone tissue atrophy is recorded [25]. Thus, if the distance between implants is less than 3 mm, it will cause flattening of the bone apexes between the implants, which will lead to the formation of black triangles, due to the loss of gingival papillae (Fig. 2 c). Using the TRIP system, as described in the first point, biocompatible pins are surgically integrated into the interdental bone apexes before tooth extraction (Fig. 2e). After completion of osseointegration, or during the same appointment (immediate protocol), tooth extraction is performed while biocompatible pins must maintain the original bone level (Fig. 2e). Implants can be placed using either an immediate or delayed protocol, while biocompatible pins must counteract the lateral component of bone loss that occurs around each implant, preserving interdental papillae and preventing the formation of interdental black triangles (Fig. 2f).
Rice. 2. TRIP system and adjacent implants: a-c: tooth extraction and insufficient distance between implants leads to bone resorption and the formation of a black triangle. d-f: the introduction of biocompatible pins before the removal of teeth replaced by implants preserves the interdental bone and papillae. 3) Preservation of interdental bone apexes between teeth and implants (before extraction): loss of bone tissue in the area of the interdental plate after installation of an implant in the vicinity of natural teeth is not as critical as in other clinical situations if socket preservation and atraumatic extraction techniques were used to prevent or reduce the likelihood of resorption of interalveolar bone tissue, which subsequently leads to morphological changes in the bone crest [26]. In such clinical situations, the height of the interdental bony apexes is usually maintained by the presence of adjacent natural teeth, while the preserved bony apex reliably maintains a stable soft tissue configuration [27]. However, after tooth extraction, some bone loss may occur, causing the appearance of black triangles, due to soft tissue recession when the defect is restored with a single implant [8,28]. Clinical observations have confirmed that soft tissue recession is even more noticeable in thin gingival phenotypes [27]. Similar to the previous two indications, with the TRIP system, biocompatible pins are surgically placed into the interdental bony apexes prior to tooth extraction. After completion of osseointegration, or during the same procedure (immediate protocol), the tooth is extracted and biocompatible pins should prevent resorption of the interdental bone apexes. The implant can be placed using either an immediate or delayed protocol, while biocompatible pins are designed to counteract the lateral component of peri-implant bone loss by preserving interdental papillae and preventing the formation of interdental black triangles. 4) Preservation of iatrogenic interdental bone peaks created by ovoids of the intermediate part during prosthetics with bridges or adjacent implants, adjustment of the site (after removal): in edentulous ridges, flattening of both bone and gingival architecture is observed (Fig. 3a). To create the illusion of interdental papillae in conjunction with the ovoids of bridges or adjacent implants, the clinician can recontour the soft tissue and underlying bone with a bur (Fig. 3b) [29] and then cement the partial temporary denture with a veneer in direct contact with the newly formed ridge until complete healing or install implants. Once the ovoid pontic or implant-supported structure is in place, the resulting bony apexes may further resorb, causing retraction of the interdental papillae and the formation of interdental black triangles (Fig. 3c). Again using the TRIP system, biocompatible rods were first surgically integrated into the edentulous ridge bone according to the desired position of the new gingival papillae (Fig. 3e). After completion of the osseointegration process or immediately after the insertion of pins at the same appointment (immediate protocol), the doctor reconstructs the ridge so that temporary crowns or implants can be relined and secured (Fig. 3f). After placement of the final restoration, biocompatible pins should prevent the resorption of the formed bone apexes over time, preventing the formation of black triangles by preserving the interdental papillae (Fig. 3f).
Rice. 3. TRIP system and edentulous ridge: a-c: in the area of the usual ovoid pontic or between implants, bone resorption and the formation of a black triangle may occur over time. d-f: the introduction of biocompatible pins before the formation of ovoids or the installation of implants will preserve the newly formed interdental bone and papillae.
CLINICAL CASE
A 68-year-old woman was treated for severe localized periodontitis in an aesthetically significant area. Her main complaint was the presence of spaces between the teeth and the unsightly appearance of the anterior teeth in the upper jaw. Periodontitis disrupts the osseous and gingival architecture, causing tooth movement, protrusion, mobility, trema, and diastema (Figure 4). A targeted radiograph revealed severe bone resorption and an unfavorable root/clinical crown ratio (Fig. 5).
Rice. 4. View before treatment. Destroyed gingival architecture and tooth migration.
Rice. 5. Radiographs before treatment. Severe localized horizontal bone atrophy may be observed.
The treatment plan included removal of the four upper incisors and replacement of the defect with a fixed partial bridge with 4 pontic ovoids. The challenge was to recreate the osseogingival architecture where it had been lost and preserve it in areas where it was still present. For this purpose, the TRIP system was used. There were no general medical or dental contraindications for the use of the system. This clinical situation before removal is presented in 1 point of indications.
DIAGNOSTIC STAGE
To correct the protrusion of the upper incisors, an esthetic template (on a vacuum former) was made from colored acrylic resin (Jet Kit, Lang Dental Manufacturing Co., Inc., www.langdental.com) to assess the correct position of the incisal edge of the teeth in relation to the patient's face. The information was then transferred to a modified diagnostic cast to complete the diagnostic wax-up. Changes made to the diagnostic model consisted of simulating tooth extraction; formation of tooth sockets that reproduce the intermediate parts of the bridge with an ideal ovoid shape; and restoration of the positive architecture of the gums, smoothed due to the development of periodontitis (Fig. 6 and 7). The diagnostic waxup was used not only to fabricate the immediate prosthesis, but also to indicate the position (mesio-distal) of the five titanium pins, as shown by the blue vertical lines on the diagnostic model (Fig. 8).
Rice. 6. The pre-extraction diagnostic model shows the planned modified gingival levels (red lines) and titanium rod locations (blue lines).
Rice. 7. Modified diagnostic model with simulation of tooth extraction.
Rice. 8. Wax diagnostic modeling. Restored inter- and intra-dental proportions.
SURGICAL STAGE
To visualize the interdental bone, a mucoperiosteal flap was removed using an intrasulcular incision from tooth No. 5 to No. 12. As shown on radiographs (Figure 5), the bone relief is smoothed due to periodontitis. A piezosurgical device with attachments (Mectron spa, www.mectron.com) was used for osteotomy. To control the size of the osteotomy, a special template with the shape and size of titanium pins was used. Titanium pins were inserted with forceps into a given area (Fig. 9) and then deepened using a chisel and a surgical hammer. As a result, all titanium pins received primary stability (Fig. 10).
Rice. 9. Surgical phase. Passively installed titanium rods.
Rice. 10. Deepening titanium pins using a hammer and chisel to achieve primary stability.
Next, the intervention site was filled with granular osteoconductive material (Bio-Oss®, Geistlich Pharma AG, www.geistlich-na.com) and covered with an absorbable membrane (Bio-Gide®, Geistlich Pharma AG). The flap is sutured with 4-0 Vicryl Plus suture (Johnson and Johnson Intl., www.jnj.com). Intraoral radiographs were taken to monitor the placement of titanium pins (Fig. 11).
Rice. 11. Control radiographs before removal demonstrate installed titanium pins.
REMOVAL AND MANUFACTURE OF TEMPORARY PROSTHETICS
Three months after the introduction of interdental titanium pins, the upper incisors were removed. A temporary fixed partial denture with 4 ovoids in the pontic was relined to the sockets of the extracted teeth formed with osteoinductive material (BIO-oss) and fixed. Two weeks after extraction, the gingival margin acquired a sharp positive architecture (Fig. 12). The goal was to maintain this result over a long period of time.
Rice. 12. Toothless comb. View 2 weeks after removal of new acute positive gingival architecture.
RECORDING DATA
A month after fixation of the prosthesis, measurements were taken to assess the change in the height of the gingival papilla. Two orthodontic transcortical titanium screws (Spider Screw®, Ortho Technology, www.orthotechnology.com) serving as a guide were inserted symmetrically apically between teeth #7-8 and #9-10, respectively. The distance was measured using a digital caliper (Mitutoyo America Corp., www.mitutoyo.com) from the center of the screw head to the tip of each papilla (Fig. 13).
Rice. 13. Measurements were made using transcortical screws as reference points.
Distances (D) were measured at six different locations at 1 month (baseline-T0), 6 months versus baseline (T1), and 12 months versus baseline (T2) (Figure 14). All measurements were taken 5 minutes after removal of the temporary fixed partial denture. Each value was the average of three measurements for each gingival papilla made by three different operators. Average distances (D) are given in Table 1.
Rice. 14. Measurements were taken of six distances from reference points to the apexes of the papillae.
A fixed effects linear regression panel estimator was created where the mean gingival papilla height (D) was regressed over time to determine whether there was a decreasing or increasing trend. This model was estimated by grouping measurements at six different locations (Table 1), excluding location 3 because it was highly correlated with location 4. Model evaluation showed a significant (P = 0.001) and positive regression coefficient (coefficient = 0.0497) for time variable, indicating an increasing growth trend over a 12-month interval (papillary growth). This growing trend is also evident from the data shown in Figure 15.
Rice. 15. Linear regression panel. Papillary height (D) value for six locations over 12 months (time).
The same model was further estimated without considering location 4 instead of 3. Similar results were obtained (P = 0.004, coefficient = 0.0453), consistent with the same conclusions.
This analysis, based on a small sample of observations on one patient, was descriptive only and showed encouraging results, but no definitive conclusions can be drawn from it.
After the first data collection of 12 months, radiographic and clinical measurements were taken at 24 months from the fixed reference points, after removal of the pins. Data recorded at 24 months (distance D) were comparable to measurements at 12 months, with no change in papilla height.
X-RAY CONTROL
X-ray evaluation of titanium rods before extraction and at 6 and 12 months after extraction does not show significant changes (Fig. 16).
Rice. 16. X-ray control 12 months after removal.
RECOVERY PHASE
The final impression was made to create the master model. The ovoids in the pontic area were isolated and formed on a plaster model to reproduce the ideal gingival contour. Particular attention was paid to the interdental spaces, replaced by titanium pins (interdental bone apexes).
The metal framework was made using the cut-back technique from the final diagnostic wax-up, then it was tried on in the oral cavity before veneering with ceramics. The ceramic ovoid profiles of the intermediate part were made convex in all directions and carefully polished. The final fitting of the fixed bridge was performed in the oral cavity to control the tightness of the pontic pontic (Fig. 17).
Rice. 17. Trying on a metal-ceramic bridge-like fixed prosthesis in the oral cavity.
Temporary blanching of the soft tissue was noted while the patient was biting on the cotton rolls. The dental floss passed under the intermediate part smoothly, without resistance, which indicated the possibility of final cementation of the prosthesis (Fig. 18). X-ray control after treatment showed the correct positioning of the interdental pins and the absence of bone resorption (Fig. 19).
Rice. 18. Cemented fixed bridge prosthesis, frontal view.
Rice. 19. X-ray control after cementation.
DISCUSSION
The TRIP system is based on the same biological principles that are the basis of modern implantology. Within a few weeks of surgical placement, the bone and titanium will establish contact, ultimately leading to osseointegration of the titanium pins [19,20]. In order to increase the bone-to-metal contact surface, the pins can be roughened in accordance with the various surface treatment techniques already available and used for root-shaped implants.
The role of the TRIP system is to prevent bone resorption of the interdental apexes. This property of titanium (as a biocompatible material) is usually seen in cases involving unloaded extraoral implants supporting maxillofacial prostheses (eg, auricular prostheses)[22,23]. In these clinical settings, the transdermal implant components create communication between the intraosseous implant (body), the bone crest, and the external environment. Intraorally, the transmucosal components of dental implants (implant neck or abutment) create a connection between the implant and the oral microflora. Therefore, on the surfaces of the implant-abutment connection, bacterial plaque can accumulate in microgaps, contributing to the occurrence of inflammation, which then leads to complications [30,31]. Conversely, in a TRIP system, pins are designed to be installed in a closed environment, without being exposed. This submerged status provides more favorable conditions for long-term preservation of osseointegration.
If the apex of the interdental pin becomes exposed over time, it will still provide useful support to the gingival papilla, acting as a supportive and tolerant underlying soft tissue, as is the case with transmucosal components of rounded implants.
In the patient situation presented here, the raised mucoperiosteal flap was of relatively large extent because many periodontally complex sites were involved in the placement of titanium pins. On the other hand, the pin integration surgical technique can be minimally invasive, especially for a periodontally healthy patient. Given the small size of the pins, its implementation can be accomplished by elevating only the buccal half of the apex of the papillae to such an extent that the interdental bony apexes are exposed, or by creating a vertical incision along the length of the papilla and opening a vertical envelope flap to expose the bone.
Surgical insertion of interdental titanium rods should ideally be made at least 1 mm into the bone peak, or at least just below the buccal cortex, with the tip of the rod aligned with the highest point of the bone peak. For this reason, the thickness of the rod should be minimal, which will allow the surgeon to insert the pin deeper without causing deformation of the bone tissue. The rods used in the reported clinical case were 0.5 mm thick.
Clinically, bony apical thickness can be assessed by using a wax micrometer and subtracting the buccal and palatal mucosal thickness, which is measured by probing the bone with a periodontal probe. Once the nail is covered with bone graft and membrane, no gray discoloration of the soft tissue should be visible. The grayish color of titanium can cause soft tissue staining if the rod is partially exposed due to buccal bone resorption. For this reason, the idea arises of using white, for example, biocompatible zirconium rods for clinical studies and clinical applications.
In this patient, measurements were taken clinically with an electronic caliper from a fixed reference point to the apices of the papillae, and three operators performed the measurements three times each. A more refined approach to evaluate measurements made with standard X-rays would probably provide more accurate data and therefore this method is recommended for all future and ongoing studies with the TRIP system.
In this particular clinical situation, a baseline (T0) clinical measurement of papillary height was taken 1 month after the iatrogenic creation of a new favorable gingival architecture with prosthetic ovoids. Initially, the preoperative contour of the gingival margin was disrupted due to periodontitis. In future studies, if performed on patients with healthy marginal gingiva, the baseline (T0) height of the gingival papilla should be recorded before tooth extraction. However, the results showed not only preservation of the papillae over a 12-month period due to exposure to the ovoids of the applied prosthesis immediately after extraction, but also some growth of the papillae, most likely due to lateral compression exerted by the pontic portion of the prosthesis [6].
In addition, for this patient, the healing phase was characterized by the presence of a thick gingiva phenotype, for which, within 1 year after surgery, coronal displacement of the gingival margin was more common [32].
After removal of the cortical screws used as a fixed reference point, clinical and visual assessment of papillary height for this patient was continued until 36 months at routine examinations every 3 months. The appearance of black triangles due to recession of the gingival papillae was not noted. In addition, nonstandardized routine x-ray examinations typically used to monitor bone levels in the area of dental implants have shown no noticeable bone loss around interdental titanium rods.
Several sophisticated techniques have been described to preserve alveolar bone: vestibular or interproximal. Some techniques recommend removing the root by sawing the tooth during implant placement, 15 others recommend installing root-shaped titanium implants either near or in direct contact with the remaining root fragments [33]. The TRIP system uses sterile, biocompatible rods placed in healthy bone, reducing the risk of infection.
CONCLUSIONS
Although controlled, prospective in-vivo studies and more data are needed to demonstrate the long-term effectiveness of the presented technique, the TRIP system, based on the biological principles of osseointegration, may be a promising solution for preserving the aesthetic architecture of the marginal gingiva.
Source: dental-revue.ru
BIBLIOGRAPHY:
1. Rufenacht CR. Structural Esthetic Rules. Fundamentals of Aesthetics. 1st ed. Chicago, IL: Quintessence Publishing Co Inc; 1990:127.
2. Frush JP, Fisher RD. The dynesthetic interpretation of the dentogenic concept. J Prosthet Dent. 1965;8(4):558-581.
3. Lombardi RE. The principles of visual perception and their clinical application to denture esthetics. J Prosthet Dent. 1973;29(4):358-382.
4. Cho HS, Jang HS, Kim DK, et al. The effects of interproximal distance between roots on the existence of interdental papillae according to the distance from the contact point to the alveolar crest. J Periodontol. 2006;77(10):1651-1657.
5. Sharma AA, Park JH. Esthetic considerations in interdental papilla: remediation and regeneration. J Esthet Restor Dent. 2010;22(1):18-28.
6. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63(12):995-996.
7. Chang L.C. Factors associated with the interdental papilla height between two maxillary central incisors: a radiographic study. J Periodontol. 2012;83(1):43-49.
8. Choquet V, Hermans M, Adriaenssens P, et al. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72(10):1364-1371.
9. van der Velden U. Regeneration of the inderdental soft tissues following denudation procedures. J Clin Periodontol. 1982;9(6):455-459.
10. Kois JC. Altering gingival levels: the restorative connection. Journal of Esthetic Dentistry. 1994;6(1):3-7.
11. Palacci P, Ericsson I, Engstrand P, Rangert B. Papilla regeneration technique. Optimal Implant Positioning & Soft Tissue Management for the Branemark System. Chicago, IL: Quintessence Publishing Co Inc; 1995:59-70.
12. De Castro Pinto RC, Colombini BL, Ishikiriama SK, et al. The subepithelial connective tissue pedicle graft combined with the coronally advanced flap for restoring missing papilla: a report of two cases. Quintessence Int. 2010;41(3):213-220.
13. Jaiswal P, Bhongade M, Tiwari I, et al. Surgical reconstruction of interdental papilla using subepithelial connective tissue graft (SCTG) with a coronally advanced flap: a clinical evaluation of five cases. J Contemporary Dent Pract. 2010;11(6):49-57.
14. Becker W, Gabitov I, Stepanov M, et al. Minimally invasive treatment for papillae deficiencies in the esthetic zone: a pilot study. Clin Implant Dent Relat Res. 2010;12(1):1-8.
15. Yalcin S, Aktas I, Emes Y, et al. A technique for atraumatic extraction of teeth before immediate implant placement using implant drills. Implant Dent. 2009;18(6):464-472.
16. Takei HH, Han TJ, Carranza FA Jr, et al. Flap technique for periodontal bone implants. Papilla preservation technique. J Periodontol. 1985;56(4):204-210.
17. Cortellini P, Prato GP, Tonetti MS. The modified papilla preservation technique: A new surgical approach for interproximal regenerative procedures. J Periodontol. 1995;66(4):261-266.
18. Cortellini P, Prato GP, Tonetti MS. The simplified papilla preservation flap. A novel surgical approach for the management of soft tissues in regenerative procedures. Int J Periodontics Restorative Dent. 1999;19(6):589-599.
19. Albrektsson T, Jacobsson M. Bone-metal interface in osseointegration. J Prosthet Dent. 1987;57(5):597-607.
20. Meffert RM, Block MS, Kent JN. What is osseointegration? Int J Periodontics Restorative Dent. 1987;7(4):9-21.
21. Marcelis K, Vercuyssen M, Nicu E, et al. Sleeping vs. loaded implants, long-term observations via a retrospective analysis. Clin Oral Implants Res. 2012;23(9):1118-1122.
22. Wright RF, Zemnick C, Wazen JJ, Asher E. Osseointegrated implants and auricular defects: a case series study. J Prosthodont. 2008;17(6):468-475.
23. Karakoca S, Aydin C, Ylmaz H, Bal BT. Survival rates and periimplant soft tissue evaluation of extraoral implants over a mean follow-up period of three years. J Prosthet Dent. 2008;100(6):458-464.
24. Abrams H, Kopczyk RA, Kaplan AL. Incidence of anterior ridge deformities in partially edentulous patients. J Prosthet Dent. 1987;57(2):191-194.
25. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
26. Agarwal G, Thomas R, Mehta D. Postextraction maintenance of the alveolar ridge: rationale and review. Compend Continue Educ Dent. 2012;33(5):320-326.
27. Nisapakultorn K, Suphanantachat S, Silkosessak O, Rattanamongkolgul S. Factors affecting soft tissue level around anterior maxillary single-tooth implants. Clin Oral Implants Res. 2010;21(6):662-670.
28. Gastaldo JF, Cury PR, Sendyk WR. Effect of the vertical and horizontal distances between adjacent implants and between a tooth and an implant on the incidence of the interproximal papilla. J Periodontol. 2004;75(9):1242-1246.
29. Garber DA, Rosenberg ES. The edentulous ridge in fixed prosthodontics. Compend Continue Educ Dent. 1981;2(4):212-223.
30. Jansen VK, Conrads G, Richter EJ. Microbial leakage and marginal fit of the implant-abutment interface. Int J Oral Maxillofac Implants. 1997;12(4):527-540.
31. Subramani K, Jung RE, Molenberg A, Hammerle CH. Biofilm on dental implants: a review of the literature. Int J Oral Maxillofac Implants. 2009;24(4):616-626.
32. Pontoriero R, Carnevale G. Surgical crown lengthening: a 12-month wound healing study. J Periodontol. 2001;72(7):841-848.
33. Hurzeler MB, Zuhr O, Schupbach P, et al. The socket-shield technique: a proof-of-principle report. J Clin Periodontol. 2010;37(9):855-862.
How are parapulp pins installed?
It should be noted that implanting pins is a delicate job and requires the precision of a dentist. Before installing a titanium pin, it is necessary to clean and seal the dental canal to prevent possible inflammation. The process then looks like this:
- The tip of the pin is inserted into the hard tissue of the tooth.
- The pin is fixed with dental cement.
- Further restoration (building up) of the tooth is carried out using a composite material. The shade is selected in accordance with the natural color of healthy chewing elements.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
Sale of pins for fixing membranes throughout Russia
In our online store you can buy different models of pins, paper or titanium pins and devices for storing and installing them (pin holders, multi-section boxes) in St. Petersburg, Moscow and other cities.
We cooperate with foreign and domestic companies that produce high-quality consumables and instruments for orthodontics. Medical pins comply with international quality standards, certificates and other documents are provided.
Order dental instruments by filling out a special form: indicate the address, the name of the clinic or your name, the number of pins and other materials. For your convenience, we offer the “One-Click Purchase” option: select a product, provide a phone number or email address. Our employees will call or write to you to discuss the time, collection address, payment method.
We offer to buy pins at prices from manufacturers, with pleasant promotions and discounts. If necessary, we give installments of up to 6 months to pay for the goods. Find out more about the terms of cooperation from our managers.
Advantages and disadvantages of restoring the integrity of the dentition using pins
The main advantage of using parapulp pins is the ability to restore a tooth even in case of severe destruction. There is no need to remove the chewing element and install an implant, since the base will not be affected. This method also has the following advantages:
- the root system is not affected;
- the mucous membranes of the mouth are not irritated (unlike wearing crowns);
- do not cause allergic reactions;
- long period of operation (up to 10 years);
- the ability to choose a pin for a specific situation thanks to a wide range of models;
- affordable price.
Quality, durability and reasonable cost are, of course, huge advantages. But despite all the advantages, modern patients prefer other methods of jaw restoration. The fact is that the metal spoke “shines through” the composite and somewhat spoils the aesthetics. Therefore, it is not recommended to use parapulp pins on incisors and canines without the use of crowns. A good dental specialist will definitely offer a solution to the problem of dentition restoration if the installation of a pin is not suitable for the patient for any reason.
Sources:
- Personal experience as an orthopedic dentist;
- Abolmasov N.G., Abolmasov N.N., Bychkov V.A., Shashmurina V.R. Replacement of defects in teeth and dentition with fixed dentures. - Smolensk, 1995;
- Arutyunov S.D. Principles of designing stump pin inlays for pathological abrasion of teeth. - Dentistry, 3, 1997;
- Bragin E.A., Dolgalev A.A., Skryl A.V. Method of manufacturing stump inlays in a laboratory using fire-resistant models (certificate of rational approval No. 953, issued by SGMA on September 30, 1998);
- Bragin E.A., Cheprakov V.V., Skryl A.V., Stroganov G.N. A method for restoring teeth destroyed below the level of the gingival margin using laser coagulation of the gums (certificate for rationalization No. 963, issued by the SGMA on December 30, 1998);
- Borovsky E.V. Clinical endodontics. — 2nd ed., add. And correct. / E.V. Borovsky. - M.: JSC "Dentistry", 2003;
- Cohen Stephen. Endodontics. — “Peace and Family”, St. Petersburg, 2000;
- N. Baba - Contemporary Restoration of Endodontically Treated Teeth (2016);
- Peter Murray - A Concise Guide to Endodontic Procedures (2015).
Procedure for caring for pinned teeth
In the postoperative period, patients are recommended:
- adhere to a gentle diet, give up alcohol, cigarettes and food that can injure the epithelial tissues of the oral cavity;
- provide thorough hygienic care of teeth and oral cavity;
- floss regularly;
- do not attempt to open bottles with your teeth, do not crack the shells of nuts or seeds;
- visit the dentist at least once every six months.
It is important to understand that the appearance of pain, swelling, hyperemia or inflammation of the gums in the area of the restored tooth may indicate the development of serious complications of the procedure. For this reason, identifying the symptoms described above is the basis for contacting doctors and receiving professional medical care.