Periodontium is the connective tissue adjacent to the root system of the tooth. Accordingly, periodontitis is considered an inflammation or change in the structure of tissues in this area. The periodontium consists of blood vessels, nerve connections and lymphatic formations. It performs the function of feeding the organ and distributing the load from the tooth to the bone.
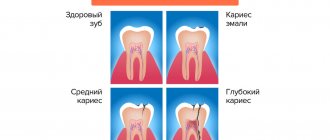
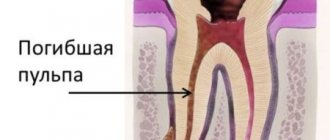
Periodontal inflammation is a fairly common disease, since this diagnosis occurs as a complication of advanced dental caries. The destruction of dental tissue opens access to the internal cavity of the organ. The next stage usually becomes pulpitis - inflammation of the nerve bundle of the tooth, and if this process is not stopped, then the infection through the root canal goes deeper into the root and, as a result, leads to periodontal infection.
Of the many types of periodontitis described below, the leading position is occupied by periodontal inflammation of infectious origin. Hemolytic streptococci, entering the pulp tissue, slowly corrode it, destroying the entire tooth structure.
Symptoms and manifestations
If pulpitis is diagnosed by acute pain upon contact with cold or hot food, then the characteristic symptoms of periodontitis are painful tapping or pressing on the tooth.
This diagnosis may be indicated by:
- swelling of the cheek or gum near the tooth;
- a feeling of fullness in the tissues of the organ;
- the occurrence of a fistula with the outflow of pus into the oral cavity;
- increased pain when eating or pressing on the causative tooth;
- the feeling of an “overgrown” tooth (due to compaction of the tissues under the root, the organ begins to bulge);
- pulsation in the root area;
- increased temperature in the area of the causative tooth.
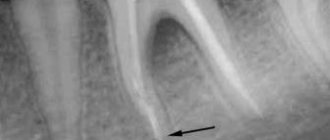
The chronic type of this disease can be asymptomatic and detected only with the help of an X-ray examination. Therefore, the insistent recommendations of the dentists of the LeaderStom clinic to undergo a dental examination by a doctor once every six months are so important for the early detection of such diseases.
Is it possible to get rid of gaps between teeth?
If you have diastema, you should definitely visit an orthodontist, since getting rid of gaps in your teeth is not only possible, but also necessary. Modern treatment methods make it possible to cope with such a problem quite quickly, and dentists offer a large selection of methods for hiding the gap.
The only situation where treatment is not required is diastema on baby teeth in children. This is considered normal and does not require medical intervention. Over time, when the bite changes, the teeth take on the correct position on their own.
A small diastema on baby teeth is normal.
Types and differential diagnosis
Like most diseases, periodontitis can occur in acute or chronic form. Sluggish periodontal inflammation is divided into three types:
Granulating
Depending on the type of infection that affects the tooth tissue, and on the specific immune response of the body, various kinds of altered tissues are formed in the periodontal cavity. With chronic periodontitis of this type, granulating tissue appears. It looks like a loose red formation near the top of the tooth root, which quickly grows and thereby destroys the bone tissue of the jaw. Of all three types of chronic inflammation, granulating periodontitis is considered the most active and pronounced. Its characteristic manifestation is the formation of fistulas, which can keep the tooth in a latent form of the disease for a long time. Connective tissue can not only affect the plate of the alveolar process (jaw), but also spread even to the skin. Therefore, advanced cases of periodontitis are much more difficult to treat and can affect large areas of tissue, including adjacent teeth. An X-ray image allows differentiation of granulating periodontitis from other types of periodontal disease. It clearly shows darkening in the area of the apex of the tooth root with circular outlines of tissue or in the form of flames. At the same time, the image does not show sharp boundaries, as in some other classifications of periodontitis. These dark spots indicate that the bone tissue has dissolved as a result of inflammation and has been replaced by connective tissue.
Fibrous
This form of the disease is quite rare and is accompanied by an asymptomatic chronic course. As a result of sluggish periodontitis, connective fibrous tissue forms around the tooth root. It is denser and is visible on an x-ray as a periodontal tooth gap, more widened than usual. The result of the appearance of fibrous tissue can be:
- suffering from acute periodontitis, which was successfully treated;
- poor-quality filling of tooth root canals;
- lack of treatment for granulating periodontal inflammation.
If the disease has entered the stage of remission (quiescence), and the patient does not complain about the causative tooth, then fibrous periodontitis cannot be treated. However, in cases of exacerbation, therapy in the form of refilling the root canals of the tooth is possible.
Granulomatous
If granulating periodontitis does not have clear outlines on an x-ray, then granulomatous periodontitis is characterized by the presence of a capsule with purulent contents. It occurs at the apex of the tooth root and gradually grows, affecting the bone tissue.
There are three degrees of development of periodontal abscess:
- Granuloma. The size of the capsule with this diagnosis reaches 0.5 cm in diameter.
- Cystogranuloma. It is diagnosed when the dense membrane reaches 1 cm.
- Cyst. More than one centimeter in diameter suggests the cystic development of periodontitis.
An increase in granuloma indicates that the inflammatory process does not find a way out and continues to dissolve the bone tissue near the tooth. In this case, a whole chain of pathological processes occurs in the human body. Sometimes particularly advanced cases showed a cyst of up to 4-5 cm in the tissue, which significantly impaired the integrity of the lower jaw, increasing the risk of its fracture.
On the other hand, the accumulation of serous fluid in the tooth area regularly causes additional intoxication to the entire body, which can be accompanied by periods of weakness, fatigue, low-grade fever and other symptoms of periodontitis.
Among all forms of chronic
Granulomatous periodontitis is considered to be the most sluggish. The fibrous tissue of the capsule serves as a protective barrier that prevents pathogenic bacteria from entering the blood. Therefore, the liquid in the capsule can remain in the tooth tissue for years without showing itself. Depending on their location, granulomas can be located either immediately under the root apex or in the tissues of the lateral cavity.
Conclusions. Expert advice
A gap or gap between the front teeth is called a diastema. This is a malocclusion that occurs for various reasons: genetics, early change of teeth, anomaly in the shape or size of the incisors, etc. There are false and true diastemas: the first appears in children and is “outgrown”, the second is permanent and requires treatment.
It is possible to get rid of the gap between teeth, but all methods require a visit to the orthodontist, and attempts to correct the problem using traditional methods are simply dangerous. To correct the dentition, braces, plates, mouth guards, and surgical methods are used. You can also make cosmetic corrections: install veneers and lumineers, close the gap with a filling, or extend incisors.
It is not necessary to correct the diastema if it is small and the doctor considers it safe. A small cleft is a cosmetic defect. If the gap is large, it causes caries, eating problems, curvature of the jaw bone, etc. The development of diastema can only be prevented through regular visits to the doctor.
Causes of development of chronic periodontitis
As already mentioned, one of the main causes of periodontal inflammation is untreated caries. However, the disease can develop for other reasons.
- Low quality filling materials. Some types of root fillings (especially those based on clove oil) can dissolve over time, forming empty cavities in the tooth tissue, which become a favorable breeding ground for anaerobic microbes. Other filling materials may shrink or crack, which can lead to the same result with bacteria and periodontitis. Partial filling of the root canal. Very often, when removing the pulp and cleaning the canals of the tooth, a small area remains at the apex of the root. If the canal is not completely sealed, then an infection develops in these tissues, which ultimately leads to periodontitis.
- Perforation of channels. When installing pins or cleaning channels, they sometimes break through. If a small hole in the root of a tooth is not disinfected and sealed hermetically, then inflammation will develop on the part of the periodontal tissue. This disease is characterized by the occurrence of periodontitis on the puncture side.
- Inflammation of the gums or periodontitis can also cause periodontal disease. There is a high probability of infection spreading if the patient has chronically inflamed gums with deep pockets of soft and then bone tissue. Particularly advanced cases can even lead to periodontitis of the apex of the roots.
- Tooth injuries. There is a category of people who do not consider it dangerous to crack a nut or open a beer bottle with their teeth. This bravado lasts until the tooth becomes inflamed or breaks off. Even such a “harmless” action as the habit of chewing a pen can turn into chronic periodontitis.
In addition to the obvious provocateurs of this disease, there are also secondary factors that indirectly cause or contribute to the development of incipient periodontitis in the dental tissues.
- Failure of metabolic processes in the body.
- Pathogenic microflora in the oral cavity.
- Malocclusion, which leads to injury to dental crowns.
- Chronic diseases of internal organs.
- Reduced immunity.
- Frequent infectious and viral diseases.
- Diabetes.
- Disturbances in the endocrine system.
A separate category of such factors should include poor nutrition, which leads to multiple imbalances in the body, and poor oral hygiene.
What is the correct name for the gap between the front teeth?
The correct name for the gap between the front teeth is diastema, which goes back to the Greek word diástema (Greek διαστημα). The term means "distance", "span" or "interval". Although in Greece the word was used without reference to dental disease, today diastema refers specifically to a dental problem.
A more simplified, but also correct name for the gap between the teeth is a gap or chip. This word is used primarily in literary language and works of art. But no matter what you call the problem, it still needs to be treated: although diastema is not the most unpleasant dental pathology, it remains a defect that can cause a number of dental problems.
Acute periodontitis
The acute form of this disease is characterized by similar symptoms as in the chronic course of the disease, only in a more pronounced form. Sharp pain in a tooth can begin spontaneously, often at night. In this case, the slightest touch to the causative tooth leads to a “lumbago” effect. The periodontal tissues swell significantly, which causes the tooth to rise, as if to grow. This fact further injures the diseased tissue, since the enlarged tooth, when chewing, receives more pressure from the closing tooth from the other jaw.
The active phase of the disease is divided into two types:
- serous periodontitis;
- purulent periodontitis.
The first two to three days pass through a serous period, when fluid with a large number of leukocytes accumulates at the site of infection. After this time, the serous tissue becomes purulent and all the symptoms of periodontitis intensify. A so-called throbbing pain in the tooth appears, which practically does not subside. If a person has not yet consulted a dentist, then before the visit, acute pain can be eased by taking painkillers. It is simply impossible to delay going to the doctor at this stage, since the symptoms will not allow the person to eat, sleep, or live normally. The accumulation of purulent contents at the root of the tooth corrodes hard tissues, which leads to the organ’s staggering. The areas of the gums, cheeks and lips are also painful and have swelling of varying degrees. Acute purulent periodontitis is a rather dangerous disease, since in the absence of effective antibacterial treatment it can acquire various stages of complications.
- Periodontal stage. Pus accumulates in the area of the periodontal gap, causing the feeling of an overgrown tooth. This is the initial stage of dental tissue abscess, which must be stopped immediately.
- Endosseous stage. The infection, along with pus, enters the bone tissue. The process of damage to the alveolar plate begins.
- Subperiosteal stage. The amount of pus under the root of the tooth increases, and it accumulates under the periosteum. This formation is called flux. In parallel with the increase in flux, the swelling of the cheek intensifies. Acute and aching periods of pain worsen.
- Submucosal stage. It is characterized by a breakthrough of the periosteum and the release of exudate into the soft tissue. Opening the fistula relieves acute symptoms of pain in the tooth, transforming periodontitis into a chronic form. However, as soon as the outflow is disrupted, periodontitis immediately reactivates.
Consequences
All people decide for themselves whether or not to remove the diastema. A small chip will not do any harm, but large gaps have very negative consequences, namely:
- the formation of an incorrect bite, which affects the bone skeleton, reduces the quality of nutrition, and leads to an increased risk of caries;
- the appearance of disturbances in diction due to the inability to pronounce some sounds correctly (the air flow is not fully retained by the teeth);
- violation of aesthetics, which can lead to prejudice on the part of employers and colleagues.
Periodontitis by location
There are two main divisions in the classification of periodontitis based on the location of the disease: apical and marginal. The first option (apical) is also apical, based near the apex of the tooth root. This type is the most common, since periodontal infection in most cases occurs through a descending channel: from caries to inflammation of the pulp, and then through the root canal the infection descends into the periodontal tissue. This process most often becomes chronic, since the protective mechanisms of the periodontium are much more powerful than those of the pulp. Therefore, the infection can enter the deep tissues of the tooth for years without causing signs of disease.
Marginal chronic periodontitis is located on the lateral walls of the tooth root and has the etiology of microtraumas.
Periodontitis, the treatment stages of which are a complex, complex process, requires immediate attention to a dental clinic. It is safe to say that such a diagnosis requires highly qualified specialists with extensive experience in solving such problems. Dentists of the LeaderStom network of clinics are rightfully considered the best in this area of dental therapy. The latest technologies, progressive techniques and extensive practice allow them to cope with the most complex, advanced cases.