It's all the virus's fault!
The term "stomatitis" is derived from the merger of two Greek words: stoma (mouth) and itis (inflammation). There are a great variety of different types of disease - serous, aphthous, allergic, etc. The most dangerous is herpetic, or cold sore, stomatitis caused by a virus. Its main manifestations are painful ulcers covering the oral mucosa. The trigger mechanism of the disease is the activation of herpes simplex virus types 1 and 2. First of all, the disease threatens those who have a weakened immune system and, as a result, the body simply does not have the strength to give a worthy rebuff to viruses.
Sores in the mouth as a sign of aphthous stomatitis
Wounds in the mouth can arise as a result of the development in a person of a separate independent disease of the oral mucosa, caused by the growth and development of pathogenic microorganisms. But, in addition, the cause of such wounds may also be hidden in the general somatic condition of an adult or child.
In most cases, mouth ulcers are symptoms of a disease such as canker sores. Stomatitis is a lesion of the human oral mucosa that occurs as a result of an atypical reaction of the immune system to foreign irritants. Depending on the nature and causes of the disease, stomatitis can be of various types: ulcerative, herpetic, allergic, vesicular, etc. But people most often have to deal with the aphthous form of this disease.
Let's name the main symptoms of aphthous stomatitis:
- The appearance of round ulcers (ulcers) in a person’s mouth, which are grayish in color and surrounded by a red, inflamed rim. Ulcers are located either separately or in groups and have different sizes.
- Painful sensations in the affected areas of the upper and lower palate of a person that occur during eating, drinking, or talking.
- Deterioration of a person’s general well-being, weakness.
- Temperature increase. But this is not a mandatory symptom; it occurs in most cases in children, since they are more difficult to tolerate aphthous stomatitis in the oral cavity.
- Enlarged submandibular lymph nodes. This symptom of aphthous stomatitis also occurs more often in children than in adults.
Forms of the disease
Lightweight
It is considered the most beneficial for the body. In this form, people with high immunity suffer from herpes stomatitis. It flows without temperature. It is distinguished by single rashes that do not cause discomfort and disappear on their own without consequences.
Average
General disorders are added: weakness, drowsiness, fatigue, loss of appetite. Rashes appear in several places at the same time. The temperature rises to 37-37.6°C.
Heavy
This form of stomatitis indicates extremely low immunity. The rashes are multiple and painful. Severe headache, chills, and vomiting appear. The temperature exceeds 38oC.
If the disease is mild, the patient may not notice any external signs!
How to distinguish herpes from stomatitis?
Many patients try to find an answer on the Internet to the question: “Do I have stomatitis or herpes? How to recognize? Herpes stomatitis can be easily distinguished from ordinary stomatitis by 3 key signs.
- With herpes infection, the rash is localized in the gum area. Whereas with stomatitis - on the soft tissues of the oral cavity (tongue, cheeks).
- A herpes rash first appears as blisters, which then ulcerate, while stomatitis begins with the appearance of ulcers.
- Herpetic stomatitis is characterized by a stable appearance of the rash in the same places, and with ordinary stomatitis its location often changes.
First aid
If the temperature rises, you can take an antipyretic drug. In the future, before visiting a doctor, nothing should be done. Do not take antibiotics yourself or try to get into the ulcer with any object.
How to relieve symptoms of ulcers
- do not eat sour and salty foods
- food should be warm, no hot dishes or drinks
- Care should be taken to ensure that the child does not put dirty hands in his mouth
- teeth should be brushed, but make sure that the bristles do not touch the gums with ulcers
- It is recommended to rinse your mouth with herbal solutions (oak bark, chamomile) 3-4 times a day
You should be careful when using antibacterial solutions. They must be prescribed by a doctor. If such solutions are used incorrectly, they can provoke the development of thrush. The antibacterial agent will “kill” the beneficial microflora, which can result in a fungal infection.
Prevention of ulcers
- professional oral hygiene at least 2 times a year
- Regularly replacing your toothbrush
- Proper brushing of teeth at least 2 times a day
- using additional hygiene techniques such as irrigators, dental floss, and tongue scrapers
- Children should be monitored for bad habits such as putting dirty fingers and other objects into their mouths
- It is important to treat your teeth in a timely manner. Microbes that are found in carious teeth and rotten roots can serve as a source of infection for ulcers
If you have problems in the oral cavity, contact the specialists of the Center for Family Dentistry!
Herpetic or aphthous?
It will be somewhat more difficult to distinguish between herpetic and aphthous stomatitis. The latter got its name from the Greek term “aftha”, which means “ulcer”.
If with herpetic stomatitis there are many ulcers, but they are small, then with aphthous stomatitis there are few of them, and the size can reach 7–8 mm.
The second important distinguishing feature is the absence of swelling of the gums with aphthous stomatitis.
If you are looking for differences between herpetic and aphthous stomatitis, then the third thing you should pay attention to is the localization of the rash. Aphthous is characterized by the appearance of ulcers in the oral cavity, while herpes infection can spread to the border of the lips.
Allergic stomatitis in children
In children, the disease occurs more often than in adults, and at the same time, a weak and fragile child’s body reacts more sharply to irritants. The baby begins to be capricious, complain of pain in the mouth and, of course, is afraid to go to the dentist.
In no case should parents let a child’s illness take its course, relying on traditional methods of treatment. If the baby suffers from allergic stomatitis, no ointments or rinses will cure him 100% as long as contact with the allergen continues. Sensitive thin mucous membranes easily crack, bleed, and pathogenic microorganisms quickly penetrate into the ulcers.
It is important to take the child to a specialist as soon as possible, explain to him that the doctor will help him get rid of the pain, and begin the examination.
How to distinguish herpes sore throat from stomatitis?
Despite the fact that these medical terms have the same grammatical root, herpetic sore throat and herpetic stomatitis are two different diseases. Unlike stomatitis, herpes sore throat occurs not due to the penetration of the herpes virus, but as a result of an adenovirus infection (in particular, the Coxsackie A virus). Children are more likely to suffer from this disease than adults. The rashes are localized, for the most part, on the soft palate and tonsils. Typical symptoms of stomatitis include pain in the abdomen and abnormal bowel movements.
Attention!
The disease begins acutely, with a jump in temperature to 40 degrees, and is severe, so differential diagnosis should only be carried out by a doctor.
Why does aphthous stomatitis occur?
As noted above, the causes of aphthous wounds in a person’s mouth can be both local and general somatic in nature. Let's look at the main ones.
Local causes of aphthous stomatitis:
- Mechanical damage to the human oral mucosa. Such injuries occur as a result of a person eating hard and tough foods. Often, even a small scratch on the roof of the mouth can cause aphthous stomatitis.
- Thermal lesions of the human oral mucosa. The occurrence of wounds and the development of aphthous stomatitis in this case provoke burns of the mucous membrane, which a person could receive by consuming hot drinks or food.
General somatic causes of wounds in the human oral cavity:
- Heredity factors. The predisposition to the occurrence of aphthous stomatitis in the mouth may be determined by genetic reasons. Therefore, there is a risk of developing this disease and the manifestation of a chronic form of stomatitis (when ulcers on the mucous membrane appear regularly) in people whose parents also suffered from this disease.
- Somatic diseases. Aphthous stomatitis often develops in people who suffer from any secondary somatic diseases. For example, these could be diseases of the digestive system and gastrointestinal tract.
- Weak immunity. For this reason, children are susceptible to oral ulcers because their immunity is not yet fully developed. In a child, aphthous stomatitis is more severe than in an adult and is accompanied by an increase in temperature and a deterioration in general well-being. Against the background of colds, immunity is also often reduced, and aphthous stomatitis occurs in the person’s mouth.
- Avitaminosis. With an incorrect diet, a person does not receive enough substances necessary for the successful functioning of the body. Due to a lack of vitamins C and B or microelements such as selenium, folic acid, zinc or iron, in some cases aphthous stomatitis occurs in a person’s mouth.
- Allergy. An allergic reaction associated with eating foods such as citrus fruits, nuts (especially peanuts), chocolate, red berries (strawberries, wild strawberries) or foods containing gluten (cereals, pasta) in some cases leads to the appearance of canker sores. wound in a person's mouth.
- Stress. When a person finds himself in a stressful situation, he spends significant resources to cope with the current problem. This leads to a loss of strength, decreased immunity and a general weakening of the body, as a result of which wounds form in the person’s mouth and he develops aphthous stomatitis.
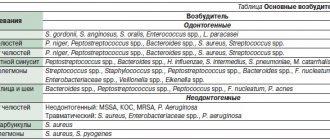
Bacterial or viral?
In addition to viral origin, the disease can be caused by bacteria: streptococci and staphylococci are normally present in the microflora of the oral cavity and begin to multiply uncontrollably during the inflammatory process. The latter may be caused by caries or periodontitis (read more about the disease in the article).
How to distinguish viral stomatitis from bacterial one? It is extremely difficult to do this at home, so it is better to consult a doctor. The main differential feature is the localization of the rash. With viral herpetic stomatitis, vesicles with transparent contents first appear on the tongue (its tip, along the side surfaces and under it), and then can even spread to the pharynx and tonsils.
For bacterial stomatitis, the location of the rash on the gums and those areas where the skin borders the mucous membrane (for example, on the red border of the lips) is more common. Also, with a disease caused by streptococci, “jams” are often observed - pustules on the corners of the mouth, which quickly begin to bleed, become covered with a crust, crack and cause constant discomfort while eating and talking.
Types of diagnostics
An experienced doctor can identify herpetic stomatitis in adults during an initial examination, relying on only two methods.
- Clinical picture.
Based on the totality of the patient’s specific complaints and distinctive external signs, the dentist will not only assess the severity of the disease, but also differentiate it from ordinary stomatitis, candidiasis, etc. - Immunofluorescence.
Express microscopy method, the most accurate for diagnosing acute herpetic stomatitis.
Symptoms of inflammatory diseases
Inflammation in the oral cavity is manifested by both general and local symptoms [1]. Even before the onset of local manifestations, general malaise, pain, irritation, rashes in the mouth, increased body temperature, and decreased appetite are noted [1]. In addition, inflammation in the mouth itself can act as a symptom of another disease or general pathology [1].
Symptoms of certain inflammatory diseases
Stomatitis is a wide group of diseases that can be caused by individual pathogens, for example, fungi (candidal stomatitis) or the herpes simplex virus (herpes stomatitis), and systemic diseases, for example, chronic diseases of the gastrointestinal tract (aphthous stomatitis) [2] .
Most often, stomatitis appears as rashes (ulcers, blisters or other forms) on the oral mucosa. The nature of the rash is a striking distinctive feature that plays an important role in diagnosis. For example, with aphthous stomatitis, the ulcers never appear on the outer surface of the lips, as is the case with lesions caused by the herpes simplex virus [2].
Herpetic stomatitis, as a rule, accompanies a general infection of the body and is characterized by rashes on the inner surface of the cheeks, tongue, palate, and lips [2].
With insufficient oral care, bacterial microflora may develop and cause deeper lesions of the mucous membrane.
If the necessary treatment of acute herpetic stomatitis is not carried out, a recurrent form occurs, which is accompanied by regular rashes on the oral mucosa of vesicles and aphthae "Microbiology, virology and immunology of the oral cavity", ed. Doctor of Medicine V. N. Tsareva.
Catarrhal stomatitis occurs quite often and develops due to the lack or poor hygiene and the presence of chronic foci of infection in the oral cavity. Symptoms of this type of stomatitis are swelling of the mucous membrane, the appearance of plaque on it, first white, then brown, and bad breath [1].
Candidiasis (candidal stomatitis, thrush) is caused by fungi of the genus Candida, which are normally always present in the mouth in small quantities [2]. Factors contributing to the sharp growth of fungi are long-term use of antibiotics and some other drugs, hypovitaminosis, endocrine and other disorders.
A striking symptom of candidiasis is the appearance of a white or yellowish-white coating on the tongue and the mucous membrane of the cheeks due to the development of inflammation in the mouth. The plaque is easily removed, revealing reddened, inflamed and eroded areas of the oral mucosa underneath.
Leukoplakia refers to chronic inflammatory diseases. It develops in response to constant irritation of the oral mucosa, for example, from a part of a denture, a sharp edge or chipped tooth, hot drinks or food, alcoholic beverages, or smoking [1]. Leukoplakia manifests itself in the form of whitish thickenings, usually in the cheek area along the line of closure of the teeth, in the corners of the mouth, on the back and on the lateral surfaces of the tongue.
Causes of herpes stomatitis
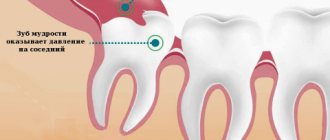
There are two types of herpetic stomatitis: acute and chronic. Acute herpetic stomatitis, according to Dr. Komarovsky, occurs only in children under 3 years of age, when for the first time the child’s body, already deprived of antibodies to the herpes virus received from the mother, is first exposed to a viral attack from the outside. Moreover, the source of infection, as a rule, is the parents themselves - carriers of the virus, who kiss the baby or lick his pacifier or feeding spoon.
Recurrent or chronic stomatitis is already the lot of adults. The disease is recurrent in nature as soon as the body’s immune forces are weakened. In this case, primary infection can occur either through airborne droplets (sneezing), or through household contact (for example, through the use of the same dishes with a virus carrier) or hematogenous (through blood during injections, etc.). The incubation period of the disease can last up to two weeks depending on the state of the immune system.
Attention!
The pathogenesis of the disease in dentistry is still unknown. But if the body is weakened, any injury to the palate or gums can provoke activation of the herpes virus types 1 and 2!
Causes
The causes of stomatitis in the mouth in adults are of the following types:
- Due to non-compliance with the rules of oral hygiene or improper care of it - rotting of food waste residues in damaged teeth or in gaps with an abnormal structure of the dentition, mechanical impact on the epithelium with a hard brush or rapid movements and strong pressure while brushing the teeth.
- Due to sudden and systematic changes in temperature in the oral cavity.
- Chemical exposure - brushing teeth with toothpastes that contain sodium lauryl sulfate or contain a lot of fluoride; sharp contrast between alkaline and acidic foods. For example, eat boiled meat with a sour apple or fresh wild berries after flour.
- Increased acidity in the mouth;
- Infectious agents: bacteria – cocci; viruses – herpes, ARVI, influenza; pathogenic microflora in the gastrointestinal tract - dysbacteriosis (not so much the microorganisms themselves, but putrefactive and or inflammatory processes due to their vital activity).
- Non-infectious pathogens - pneumococci, fungi except candida. Candida is classified as both infectious and non-infectious, depending on the quantity and location.
- Pathology with concomitant diseases: with diabetes, as a complication of periodontitis, other diseases whose symptoms are inflammatory processes in the body.
Immune nature:
- Autoimmune diseases - when antibodies attack healthy cells;
- Arthritis;
- HIV - in late stages or during exacerbations, or during manifestations of other diseases due to reduced immunity by the immunodeficiency virus.
- Taking medications or folk remedies that interfere with salivation or failure to replenish the body with fluid in a timely manner after taking them.
Often, stomatitis in adults occurs from a high temperature: 39.5 or higher, which lasts 5 days or more. After the temperature normalizes or drops to subfebrile levels, the disease goes away in 3-5 days, and in case of reduced immunity - 7-10 days.
Treatment of herpetic stomatitis
How to treat herpes stomatitis? Unfortunately, the herpes virus, once entered into a person’s blood, remains in a “dormant” state for the rest of his life. But treatment of viral stomatitis is possible provided that you do not delay visiting the dentist when the first signs of the disease are detected. During the period of therapy, in order to avoid infecting loved ones, you should eat and drink from separate containers and avoid kissing. The patient is recommended a diet that excludes spicy, smoked, sour and salty foods, which can irritate the damaged oral mucosa, and an increased drinking regimen (up to 2.5 liters per day), aimed at combating the manifestations of general intoxication of the body.
Ulcerative stomatitis - symptoms and treatment
The main goal of therapy is to reduce pain and speed up healing. First of all, it is necessary to eliminate irritants that cause discomfort to the patient. The next step is to reduce symptoms as much as possible.
To treat stomatitis, rinsing with solutions of furatsilin, miramistin, chlorhexidine, and hydrogen peroxide is prescribed. Rinsing will reduce pain and itching, and cleanse the oral cavity of food debris that injures the damaged areas.
In case of severe pain, applications with painkillers are prescribed - “Kamistad”, “Lidocaine Asept”. Treatment for different forms of stomatitis will differ.
Infectious stomatitis. When treating, it is first necessary to understand what problem with the immune system caused this condition and to strengthen the body’s defenses. To do this, Prodigiosan is administered intramuscularly, the oral cavity is treated with antiseptics, proteolytic enzymes, and UV therapy is prescribed [11].
Vesicular stomatitis. To reduce symptoms, proper rest, drinking plenty of fluids, and taking antipyretic medications will be helpful. Also, the oral mucosa is treated with antiseptics (Suprastin, Hexetidine, Pipolfen) and antiviral ointments are used - rhiodoxol and tebrofen. Antiherpetic drugs are often prescribed - Famciclovir, Acyclovir, Valacyclovir. If you follow the doctor’s recommendations, the symptoms of the disease quickly go away and the patient recovers.
Vincent's ulcerative necrotic stomatitis. During treatment, dental plaque is carefully removed, the oral mucosa is treated with antiseptics, and multivitamins are prescribed (for example, Complivita).
Allergic stomatitis. Treatment consists of eliminating the cause of the allergy and taking oral antihistamines. In severe cases of allergic stomatitis, sodium thiosulfate solution is administered intravenously. During treatment in a hospital, drip infusions of hemodez, isotonic sodium chloride solution, polyglucin, and corticosteroids are prescribed.
Chronic recurrent aphthous stomatitis. With local treatment, traumatic factors are eliminated, the mouth is rinsed with tetracycline (250 mg per 5 ml of water 4 times a day for 5-7 days), applications are made with corticosteroids and antibiotics, and painkillers are prescribed. For deep ulcers, proteolytic enzymes are used.
General treatment includes taking medications:
- tetracycline, rifampicin (two capsules twice a day);
- “Tarivid” (one tablet twice a day for 20 days);
- sodium thiosulfate (10 ml of 30% solution intravenously once a day or 1.5-3 g orally);
- “Prodigiosan” (start with 15 mcg once every five days and increase the dose to 100 mcg);
- "Levamisole" (50 mg three times a day two days in a row a week or 150 mg once);
- "Delagil" (one tablet once a day);
- "Colchicine" (one tablet twice a day for two months);
- "Aevit" (1 ml once a day intramuscularly for 20 days);
- “Histaglobulin” (2 ml subcutaneously once every three days) [11].
Stomatitis due to intoxication with salts of heavy metals and chemical solutions. If a chemical gets on the mucous membrane, you must immediately wash it off with a neutralizing solution. Further treatment of patients with chemical burns is carried out with painkillers and antiseptics and drugs that accelerate the restoration of the epithelium. A high-calorie diet is also important. For extensive scars, surgical intervention is indicated [15].
Drug therapy
Rinse
To stop the spread of infection throughout the oral cavity, as well as to prevent the occurrence of sore throat, anti-inflammatory drugs such as Stomatidine and Miramistin are prescribed. The greatest effect is achieved by repeating the rinsing procedure every 3 hours, strictly adhering to the instructions for medicinal solutions.
Antiviral drugs
To suppress the reproduction of the herpes virus, the patient is advised to take “Immudon” and “Acyclovir” orally according to the scheme, and for external use - “Viferon” ointment or “Silicea” gel.
Vitamin therapy
Tablet vitamin complexes such as “Complivit” help improve immunity.
Attention!
Before use, consultation with a specialist is recommended!
Treatment at home with folk remedies
On the Internet you can often come across the question: “How to treat herpetic stomatitis with folk remedies?” Let’s make a reservation right away: when treating this disease, you cannot rely solely on traditional medicine methods. Therapy must be comprehensive, and only a doctor can choose it correctly.
An effective folk remedy for rinsing the mouth is propolis tincture diluted with boiled water 1:3. In case of pronounced “jams” in the corners of the mouth and painful ulcers inside, applications with natural sea buckthorn oil have an analgesic and wound-healing effect.
Prevention measures
- Strengthening the immune system.
Avoid excessive exercise and stress. Take a multivitamin in the fall and spring. Regular exercise and hardening increase the vitality of the body. - Healthy lifestyle.
Get rid of bad habits: scientists have proven that excessive smoking and alcoholic beverages can become a catalyst for the activation of the herpes virus in the body. - Timely treatment of chronic diseases.
Do not forget that simple stomatitis, if you do not seek medical help in a timely manner, can develop into herpetic stomatitis. Chronic caries and acute respiratory viral diseases suffered “on the legs” also seriously undermine the body’s immune defense. - Maintain personal hygiene.
According to statistics, it is poor oral hygiene that most often opens the way for herpes infection. - Avoid oral trauma.
Even a minor microcrack from a prick with a fish bone or careless use of a toothpick can become an “entry gate” for the herpes virus.
Attention!
With reduced immunity, herpes stomatitis becomes chronic and relapsing: the disease can recur 2-6 months after recovery.
Table - diseases that manifest as a sore on the tongue
Below is a table with a detailed description of tongue diseases.
| Disease | Symptoms | Treatment | Forecast |
| Stomatitis | Main signs of the disease:
| Depending on the type of disease, the doctor may prescribe:
| The prognosis for people suffering from stomatitis is favorable, especially if the person receives appropriate treatment. Complications, as a rule, are not observed, except for the chronic form of the pathology. Therefore, it is important to treat stomatitis in a timely manner, as well as follow the doctor’s preventive recommendations. |
| Injury | Main features:
| Treatment involves treating the wound with iodine tincture or brilliant green. In some cases, antiseptic medications are used. The doctor may prescribe rinsing the mouth with disinfectants. In addition, it is necessary to maintain oral hygiene and take vitamins B and C. In case of severe injuries that result in bleeding, sutures are allowed. | With timely treatment of this phenomenon, the prognosis is considered favorable. |
| Syphilis | At the initial stage of development of the disease, general malaise, loss of strength, depression, and depression appear. Next, painless round chancres (red bumps) form on the tongue. In advanced cases, enlarged lymph nodes, destruction of bone and cartilage tissue, tooth loss, and collapse of the nose are possible. | Therapy for this disease involves the use of penicillin medications. If an allergic reaction occurs, these drugs are replaced with Erythromycin, Tetracycline or Cephalosporin. In some cases, aminoglycosides are prescribed to inhibit the growth of syphilis pathogens. | The primary and secondary stages of this disease can be completely cured. However, after completing the course of therapy, it is necessary every 3 months. take control tests within two years. The tertiary stage of syphilis is now also being treated, but the deformations of the tongue that have begun cannot be restored. Also, the deep star-shaped scars left after gummas do not disappear. |
| Cyst | Cystic neoplasms (ranulas) affect the mucous membrane, as a result of which salivation worsens and the oral cavity dries out. As the disease progresses, the patient develops speech impairments and problems chewing food. | In case of infection of the affected area, anti-inflammatory, antipyretic and antibacterial medications are prescribed. The optimal method of treating ranulas is to remove them in several ways:
| In most cases of cystic neoplasms, the prognosis is considered favorable. The disease does not pose a serious threat to the health and life of the patient. |
| Cancer | The disease manifests itself by:
| The following methods are used to treat this disease:
| With timely detection and radical combination therapy for tongue cancer, the prognosis is considered favorable in 65–80%, in some cases up to 95%. When starting treatment for advanced stage cancer with metastases to the lymph nodes, patient survival is no more than 35%. |