Reasons for appearance
This disease belongs to the genus of polyetiological ones. This means that a variety of reasons can lead to its appearance:
- injuries to the oral mucosa;
- problems with the gastrointestinal tract;
- disturbances in the functioning of the hypothalamus;
- nervous system disorders;
- side effects from taking medications.
Mouth injuries
Injured mucous membranes of the oral cavity are called the main cause of glossalgia. Microtraumas caused by foreign objects and sharp edges of teeth lead to impaired blood circulation in the capillaries, which results in stagnation of blood in the mucous membrane.
Endocrinology
Disturbances in the functioning of the gastrointestinal tract and their chronic diseases are the second common cause of unhealthy sensations in the tongue. Most often, people with reduced gastric secretion, chronic colitis, cholecystitis, and hepatitis suffer from this.
Hypothalamus
Pathologies of the hypothalamus lead to disruption of all basic functions of the body, including such important ones as: the cardiovascular system and the digestive system. These deviations are also reflected in the state of the tongue.
Nervous system
Nervous disorders, depression, constant stress, overwork, or psychological trauma are another reason.
Side effects
A famous expression says: “everything is medicine and poison.” Some medications, when used in incorrect proportions or when the body is sensitive to taking them, give side effects, expressed in glossalgia.
Other reasons
Other causes include: stomatitis, infectious inflammation of the tongue, salts of heavy metals and other chemical poisoning.
General information
Glossalgia refers to diseases of the tongue, as the sympathocomplex has a number of causes: neurogenic, symptomatic, ischemic, caused by local factors. Usually the process is polyethylogical and does not cause morphological changes; it is expressed in the form of paresthesia and hyperesthesia , which are felt as a burning sensation and perversion of taste.
The course is long-term, from several months to several years, and is associated with systemic diseases, psychological disorders or depression .
Very often, the burned oral mucosa is considered exclusively as one of the symptoms of systemic diseases, especially those affecting the nervous system, and through local irritants, glossodynia manifests itself and increases discomfort, leading to relapse.
Our team of doctors
Maxillofacial surgeon, Implantologist
Bocharov Maxim Viktorovich
Experience: 11 years
Dental surgeon, Implantologist
Chernov Dmitry Anatolievich
Experience: 29 years
Orthopedist, Neuromuscular dentist
Stepanov Andrey Vasilievich
Experience: 22 years
Endodontist, Therapist
Skalet Yana Alexandrovna
Experience: 22 years
Orthopedic dentist
Tsoi Sergey Konstantinovich
Experience: 19 years
Dentist-orthodontist
Enikeeva Anna Stanislavovna
Experience: 3 years
Classification
With neurogenic development factors, burning pain syndrome is called glossodynia . It is an organic pathology of the nervous system and is usually caused by neuralgia , neuropathies of the lingual or glossopharyngeal nerve , ganglionitis of the submandibular or sublingual autonomic node , irritation of pain from the cervical part of the autonomic trunk or functional pathology with sympathalgia , a paresthetic sensory phenomenon against the background of bulbar disorders.
Glossodynia is more common in women over 30. Depending on the form and location of paresthesia, they are distinguished:
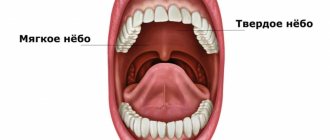
- mucosal glossopharyngeal form of glossodynia - concentrated on the root of the tongue, pharynx and cervical region of the esophagus;
- dermatomucosal form - when not only the oral mucosa is burned, but also the skin of the face.
Glossalgia is a particular manifestation of stomalgia , a disease manifested by constant pain and paresthesia of the mucous membranes and organs of the oral cavity. The burning sensation spreads not only to the tongue, but also to the palate, gums, mucous membranes of the cheeks, and throat.
Glossalgia of the tongue: symptoms, diagnosis and photos of manifestations
This disease may have the following symptoms:
- burning or painful tingling sensations;
- feeling of discomfort while eating or talking;
- pain of various types;
- numbness of the tip or entire tongue;
- decreased salivation.
The last symptom is observed in more than 30% of patients.
Unpleasant sensations are usually localized on the sides, at the tip, or at the root of the tongue. They manifest themselves especially strongly in the evening after a busy day at work or under severe stress. When eating occurs, symptoms may either intensify or not manifest themselves at all.
Pathogenesis
Pain localized in the tongue area is not a manifestation of a visible inflammatory process or the result of morphological changes.
The symptom complex of glossalgia is usually caused by damage to the autonomic nervous system, which are formed against the background of chronic somatic diseases of the digestive system, as a result of vascular and endocrine disorders. The development mechanism may be based on:
- allergic reactions;
- action of galvanic currents;
- disruption of salivation (salivation);
- decrease in the threshold for the perception of irritation.
Glossalgia: treatment
If you do not treat it in a timely manner, this disease will never be cured (such cases are rare). It will manifest itself throughout life, either subsiding during positive changes in the body, or intensifying as the diseases that led to glossalgia develop.
First of all, it is important to correctly classify this disease and not confuse it with other ailments of the oral cavity or neuralgia. And not every doctor is capable of this, only a well-trained and experienced dentist or neurologist. The insidiousness of this disease lies in the fact that it rarely manifests itself externally, which is why the experience and professional instinct of a specialist are so important when diagnosing.
After detecting glossalgia, the first step is to carry out preventive work in the oral cavity. Quite often, to eliminate it, it is enough to correct the bite, grind the sharp edges of the teeth, correct or replace implants. In general, work to eliminate objects that cause cuts and microtrauma to the mucous membrane.
To prevent the patient from experiencing pain while the dentist is working, he is injected with painkillers, or a course of rinsing with various tinctures is prescribed.
If work in the oral cavity has given only partial results, the dentist may recommend contacting the following specialists:
- general practitioner;
- endocrinologist;
- neurologist;
- psychiatrist.
These specialists will be able to determine the root cause of the disease and begin to eliminate it.
As mentioned above, most often glossalgia is a symptom of endocrinological disorders or problems with the nervous system. The patient should not be surprised if the therapist, after examining the tongue, refers the patient to a psychologist, who, in turn, will prescribe a course of psychotherapy or hypnosis.
It also happens that a comprehensive analysis of the body helps to eliminate the cause of the disease, which shows that the maximum permissible concentration of certain medications is exceeded.
No matter which doctor the patient consults, the course of treatment will not last more than two months.
Author:
Diagnostics
The disease must be differentiated from traumatic and inflammatory lesions of the mucous membrane, neuralgia, and clinical manifestations of osteochondrosis.
Glossalgia is supported by the absence of changes in the language, the diffuseness of the pain syndrome, as well as a reaction that does not correspond to the intensity of the stimulus. It should be noted that neuralgia has a specific localization, corresponding to the area of innervation of a particular nerve. With glossalgia, sensations can be diffuse or migrate.
In case of injury, the pain is constant and localized. The consequences of damage are visible on the mucous membrane; the patient’s sensations and the picture visible upon examination coincide. With glossalgia there is no such pattern. Damages in this pathology are present, but they are secondary in nature and do not correspond to the localization of pain.
Causes of Burning Mouth Syndrome
This condition may be associated with any general somatic or dental disease, or it may occur on its own. As a rule, burning mouth syndrome is a condition in which its source is unknown. It occurs spontaneously, and the patient cannot indicate the cause or trigger for the complaint.
There are several theories about the development of this pathology, but none of them have yet been proven. Researchers of this problem have made several assumptions as a theory of the origin of the syndrome. One of the most common is the theory of sex hormone deficiency, since complaints of chronic burning of the tongue are often made by pre- or postmenopausal women. True, when checking studies in this area, reliable statistical significance was not established, but, nevertheless, as a theory, this reason is supported by many practitioners [3].
“Among patients with burning mouth syndrome, women were more common. According to some studies, there were 10.3 times more women with complaints typical of this condition than men.”
Saperkin N.V., Ph.D., Associate Professor of the Department of Epidemiology, Microbiology and Evidence-Based Medicine PIMU [1]
There is an assumption that certain autoimmune processes, especially those that occur in old age, may also be background for the occurrence of burning mouth syndrome [2].
It is possible that this disease occurs in people with neurological or mental disorders, depression. But this is also not the leading theory, since there are studies indicating that it was not depression that led to the onset of the syndrome, but on the contrary, burning mouth syndrome became one of the reasons for the development of a depressive episode. The same spectrum of causes of burning in the mouth includes cancerophobia, especially in people who have quit smoking and are afraid of developing cancer of the lip or tongue, as well as in people with a fear of household transmission of STDs [2].
Injuries can lead to the syndrome, including those not noticed by a person, associated with his habits, congenital or due to pathologies with malocclusion, dental anomalies. Some researchers note that individual changes in the sensitivity and density of the oral mucosa can lead to the development of glossopyrosis. A correlation has been noted between mental lability and increased sensitivity of taste buds: in such people, the incidence of burning mouth syndrome was higher. In general, the approximate list of conditions and diseases in which the syndrome may appear is quite wide [3].
- In women, there is a deficiency of estrogen or progesterone.
- Autoimmune pathology.
- Neurological disorders, PTSD.
- Psychiatric disorders.
- Chronic irritation of the mouth, such as from improper dentures.
- Sensory defects.
Diseases that may cause a burning sensation in the mouth:
- Anemia.
- Parkinson's disease.
- Deficiency of B vitamins, zinc.
- Neuropathy.
- Hypothyroidism.
- Taking medications.
- Diabetes mellitus type 2.
- Sjögren's syndrome with xerostomia.
- Candidiasis of the oral mucosa, esophagus.
- Herpes.
- Cracked tongue.
- Allergies, including contact ones.
- Hiatal hernia.
- HIV.
- Myeloma.
- Oncological diseases [3].
Prevention
Preventive measures for diseases of the oral cavity and, in particular, the tongue are:
- giving up tobacco, hookah, electronic cigarettes and alcohol;
- daily high-quality hygiene and the use of mouth rinses that do not contain alcohol and toothpastes - without sodium lauryl sulfate;
- visit the dentist at least once a year;
- avoiding microtrauma of the tongue, for example, when using low-quality artificial onlays on teeth (veneers), when shelling seeds, eating food with sharp edges - candies, crackers, chips, nuts, apples with a hard crust;
- following a gentle healthy hypoallergenic diet.