What it is
The most common condition of the lower lip, which foreshadows a cancerous tumor, is diagnosed in most cases in males of retirement age. This disease is called abrasive pre-cancerous cheilitis of Manganotti, and it is most often provoked by various types of injuries.
A characteristic feature of precancrosis Manganotti cheilitis is the formation of small oval or round erosions on the lips without infiltration, which do not heal for a very long time and often appear over a long period of time.
This disease got its name in honor of the Italian dermatologist Manganotti, who practiced in the first half of the twentieth century and described his observations regarding the manifestations of this type of precancerous inflammation of the red border of the lips.
Cheilitis Return to HOME
(cheilitis; Greek cheilos lip + -itis) - inflammation of the mucous membrane, red border and skin of the lips. A distinction is made between actual chronic illness, which occurs independently, and symptomatic illness, which develops as a result of other diseases, such as hypovitaminosis. The most common forms of X are: exfoliative, glandular, contact allergic, meteorological, candidal, eczematous, chronic fissures of the lips, abrasive precancrosis Manganotti cheilitis.
Exfoliative cheilitis
- chronic inflammation of the red border of the lips along their entire length. The lower lip is most often affected. The etiology has not been fully elucidated. It is observed, for example, in people who have the habit of frequently licking or biting their lips, in patients suffering from thyrotoxicosis. Possible causes include immune disorders, allergies, and genetic factors. Women aged 20-40 years are most often affected. There are dry and exudative forms. In the dry form, translucent scales are visible on the red border of the lips at different stages of development ( Fig. 1
).
The scales are tightly fixed in the center, their edges are slightly raised. 5-7 days after the appearance of the scales, they are easily separated, and in their place a bright red surface remains. Patients are concerned about dryness, sometimes a slight burning sensation when eating in the affected area. Biting the scales leads to erosion. The exudative form is characterized by swelling and hyperemia of the lip, the appearance of large purulent crusts on the red border, sometimes hanging from the surface of the lip ( Fig. 2
). After removing the crusts, a bright red, slightly moist surface is exposed. Patients experience burning and pain that worsens when eating. A transition from one clinical form of H. to another is often observed. The course of the disease is long.
Diagnosis is based on a characteristic clinical picture, incl. typical localization of the process. Differential diagnosis of the dry form is carried out with meteorological and contact allergic H., lichen planus and lupus erythematosus. The exudative form is differentiated from exudative erythema multiforme, drug allergies, pemphigus, and the erosive-ulcerative form of lichen planus.
Treatment is ineffective. Neuroleptics (thioridosine) or tranquilizers (chlozepid, sibazon, etc.) are prescribed, and courses of psychotherapy are conducted. Patients suffering from thyrotoxicosis receive specialized treatment from an endocrinologist. In the dry form, it is recommended to lubricate the red border of the lips with indifferent ointments, creams, a hygienic sponge, and lipstick. A certain effect is observed after radiotherapy (Bucca's rays), and in the exudative form - after preliminary removal of the crusts. Between courses of radiotherapy, an infiltration novocaine blockade is carried (administration of 5 ml
0.25% novocaine solution into the transitional fold). Positive results of acupuncture were noted. In young people, the disease progresses more favorably, and self-healing often occurs, but in older people, the disease is difficult to treat; it is usually symptomatic.
Glandular cheilitis
at a young age, it usually develops against the background of a congenital anomaly of the minor salivary glands of the mucous membrane of the lips and transition zone (primary glandular chronicity); in people of older age groups, it is a consequence of a number of diseases (for example, lupus erythematosus, lichen planus), leading to hyperplasia and hyperfunction of the minor salivary glands (secondary glandular chronicity). With primary glandular chronicity, there is an expansion of the mouths of the salivary glands, from which, when the lip is everted, droplets of saliva are released in the form of dew. Often a rim of hyperkeratosis is detected around the orifices, and sometimes extensive areas of keratinization are formed. With secondary glandular cheloma, the red border and mucous membrane of the lip are hyperemic and swollen, in the area of the transition zone, dilated mouths of the salivary glands are revealed, from which transparent drops of saliva are released, and when a secondary infection is attached, pus is released. Treatment is electrocoagulation of the salivary glands or their excision. In case of secondary glandular cancer, therapeutic measures are aimed at the underlying disease. The prognosis is usually favorable, but cases of malignancy have been described.
Contact allergic cheilitis
occurs due to exposure to a chemical agent and is manifested by a delayed allergic reaction. More often develops in women who use lipstick; The cause may also be components of toothpaste, plastic of dentures, etc. The pathological process is localized, as a rule, on the red border of the lips, but can spread to the mucous membrane and skin. Clinically it is characterized by severe or moderate swelling of part or all of the lip, hyperemia, the appearance of scales, crusts, cracks, and erosions. Patients complain of itching and burning. The diagnosis is made based on the clinical picture and anamnesis. The latter plays a major role in differentiating contact allergic asthma from other forms, primarily exfoliative and meteorological disease. During treatment, it is necessary to eliminate the effect of the etiological factor; antihistamines (suprastin, tavegil, etc.) and local glucocorticoid ointments ( fluorocort, flucinar, etc.) in the form of applications 5-6 times a day. The prognosis is favorable.
Meteorological cheilitis
caused by the action of various meteorological factors (wind, cold, low humidity, insolation, etc.). It is more often observed in people whose profession involves working outdoors (for example, shepherds, builders). Increased dryness of the skin predisposes to the development of the disease. Clinically characterized by moderate hyperemia and dryness of the red border, the formation of small scales and cracks. Under the influence of sunlight, the development of an exudative form (actinic chronicity) with pronounced swelling, the appearance of bubbles, erosions, and crusts is possible. Patients experience a feeling of tightness of the lip, itching, sometimes burning and pain when talking and eating. The course is long-term and recurrent. The diagnosis is difficult. Differential diagnosis is carried out with exfoliative and contact allergic H., lupus erythematosus and lichen planus. During treatment, it is necessary to reduce the time spent outdoors, avoid direct exposure to sunlight, it is recommended to lubricate the red border of the lips with photoprotective creams and hygienic lipstick. In cases of severe inflammation, applications of glucocorticoid ointments (0.5% prednisolone, etc.) and oral B vitamins are indicated. In case of actinic chronic inflammation, some authors note a positive effect from the use of B vitamins in combination with hingamine (0.25 g
2 times a day for 2-3 weeks) and glucocorticoids (prednisolone 10
mg
per day). The prognosis in the case of treatment and prophylactic measures is often favorable, but malignancy is possible.
Candidal cheilitis
(mycotic X.) occurs in older people with a reduced bite, and as a result, deep folds form in the corners of the mouth. The skin of the folds undergoes weeping and maceration, a grayish-white, easily removable coating appears, containing mycelium and spores of a yeast-like fungus (mystical seizure). At the same time (sometimes in isolation) the red border of the lips is affected; becomes hyperemic, edematous, the epithelial cover becomes thinner, erosions are formed, covered with a grayish-white coating. Patients complain of burning, pain when eating and opening the mouth. The diagnosis is made based on the clinical picture and plaque microscopy data. Differential diagnosis is carried out with streptococcal infection, syphilitic papules in the corners of the mouth. Treatment includes lubricating the affected areas with antifungal ointment (nystatin, levorin, 0.5% decamine), Lugol's solution with glycerin; Multivitamins are prescribed internally. Orthopedic intervention is required. aimed at normalizing the bite.
Eczematous cheilitis
can occur in isolation or be combined with manifestations of seborrheic eczema on the skin of the face. Sensitizing factors are microorganisms, food and medicinal substances, dental materials, toothpaste ingredients, etc. In the acute stage, sharp swelling and hyperemia of the red border of the lip are observed, against which small bubbles, scales, crusts, and weeping appear. The process spreads from the red border to the skin of the lip. Patients complain of itching and burning, difficulty opening the mouth. Subsequently, the red border and adjacent skin become denser due to the inflammatory infiltrate; In some places groups of nodules, bubbles, crusts, scales, and cracks appear. Dryness, peeling, and itching in the affected area are noted. The diagnosis is facilitated by the presence of signs of seborrheic eczema in other areas of the face. Differential diagnosis is carried out with contact allergic and meteorological X. Treatment includes antihistamines and sedatives. Ointments containing corticosteroids (prednisolone, sinalar, etc.) are prescribed locally; for microbial eczema, corticosteroids with antibiotics or other disinfectants (Lorinden C, Oxycort, Dermozolon, etc.) are prescribed.
Chronic cracked lips
appear, as a rule, as a result of injury, with a decrease in their elasticity, which may be due to meteorological factors, occupational hazards; with a lack of vitamins A and group B; after diseases accompanied by blistering rashes and leading to disruption of the integrity of the red border of the lips. The microbial flora that penetrates into cracks supports the inflammatory process and prevents their independent healing. More often the crack is single and, as a rule, is located in the center of the red border; the simultaneous existence of several cracks of different lengths, depths and locations is possible. On the outside, the cracks are covered with bloody or yellow dense crusts, around which an area of limited inflammation is identified. Over time, the edges of the cracks become denser and heal poorly. Patients complain of significant (in the initial period) or moderate (over a long period) pain when talking and eating. The process is recurrent. The diagnosis is made based on examination data. During treatment, drugs that have an anti-inflammatory and epithelializing effect are prescribed locally: oxycort, rosehip and sea buckthorn oil, vitamin A preparations, solcoseryl, antibiotics, etc. The lack of a positive effect is an indication for excision of the crack within healthy tissue.
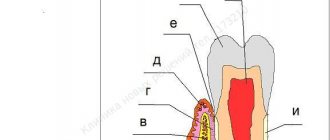
Abrasive precancrosis cheilitis Manganotti
refers to obligate precancerous diseases. It is observed mainly in men over 60 years of age. A certain role in the development of the disease is assigned to trauma, insolation, hypovitaminosis A, and diseases of the digestive system. Predisposing factors are age-related trophic changes in lip tissue and a decrease in the regenerative properties of the mucous membrane. The disease is characterized by the formation of 1-2 round or irregularly shaped erosions, usually covered with a thin crust, on an unchanged or slightly hyperemic red border. The lower lip is affected. On palpation, the affected areas are painless, no compactions are noted. The course is chronic. Erosions usually do not heal on their own. The likelihood of malignancy is high. Signs of malignancy are compaction of the bases of erosions, warty growths ( Fig. 3
). The diagnosis is based on clinical data and confirmed by the results of cytological and histological studies. Differential diagnosis is carried out with the erosive form of lichen planus and leukoplakia, herpes, and benign pemphigus. Some authors recommend starting treatment with conservative measures (elimination of irritating factors, oral administration of vitamin A, topical solcoseryl in the form of jelly or ointment, etc.) and only if there is no effect, resort to surgical intervention, others consider it necessary to carry out treatment immediately after diagnosis. excision or cryodestruction of the pathological area. The prognosis with timely radical intervention is favorable. In rare cases, the process resumes after some time.
Causes
The main reason for the development of this disease is old age. It is in old age that the immune defense weakens, pathological processes begin to form in the body, internal organs fail, and metabolism is disrupted. Because of these changes, the external defense also suffers and the epithelial layer weakens.
In old age, a person has few healthy teeth left; many have to be removed, which inevitably leads to the need to wear dentures. And since the majority of elderly people in our country are not well-off enough for treatment in paid clinics, they have to turn to state-owned clinics for the manufacture of prostheses, where the quality of the source material and the final product suffers significantly.
As a result, a complex of influencing factors, namely malnutrition of the skin of the lips, vitamin deficiencies, constant traumatic effects of low-quality prosthesis, as well as natural factors and injuries, lead to the formation of erosions on the lips.
Symptoms
The following symptoms are characteristic of abrasive precancrosis cheilitis of Manganotti:
- Formation on the red border of the lower lip of one or two or three small erosions of a round, oval or irregular shape.
- The erosion surface is most often smooth, bright red or yellow-red in color.
- Sometimes a serous or bloody crust may form on the surface of the erosion, and when removed surgically, the opened wound will bleed a little.
- Patients never complain of severe pain with abrasive cheilitis of Manganotti; on the contrary, most often the erosions are completely painless.
- The resulting erosions may not heal for several weeks or even months, and new ones soon appear in place of the healed ones or nearby.
- The disease is chronic and can last for years if the inflammation does not develop into a malignant tumor. The onset of the cancer process can be determined by the compaction of the base of the erosion and the appearance of blood at the slightest damage to the upper layer.
1.1. Etiology, pathogenesis and clinic of various forms of cheilitis
Let us dwell only on the most common forms of cheilitis in the clinic.
Eczematous cheilitis
(cheilitis eczematosis). Its main cause should be considered an allergic factor.
Various microbes can act as allergens, primarily pyococci, which cause chronic cracks in the lips. Fungi of the genus Candida
in some cases, they serve as a sensitizer, supporting, and sometimes causing eczema of the lips. Chemicals (lipsticks, dentures, some medications) can also contribute to its development. The manifestations of hypovitaminosis, primarily ariboflavinosis, sometimes resemble eczema of the lips [11, 53].
Eczematous cheilitis can be either acute or chronic. Its acute course is characterized by bright hyperemia of the lips and surrounding skin, swelling and the appearance of blisters, small cracks, bloody and yellowish crusts; areas of weeping may appear. In cases of prolonged course of eczematous cheilitis, microbiological analysis identifies streptococci, which serve as an additional allergen for eczema. In the chronic course, swelling of the lips, congestive hyperemia are noted, cracks form in the corners of the mouth, the lips are covered with scales that are easily removed by scraping [39].
Exfoliative cheilitis
(exfoliative cheilitis) was first described in 1922 by French scientists Mikulicz and Kümmel. It is a chronic inflammation of the lips, called by the authors “persistent peeling of the lips.”
The etiology and pathogenesis of exfoliative cheilitis is still unclear. Patients suffering from it (usually women) experience a more or less significant functional disorder of the nervous system. Factors that support and aggravate the disease can be various allergens of both endogenous and exogenous origin [17, 62].
Clinically, exfoliative cheilitis manifests itself in 2 forms: dry and exudative.
Exfoliative cheilitis, dry form
characterized by the following clinical manifestations: the red border (mainly of the lower lip) is dry, there is congestive hyperemia, against the background of which there are scales tightly fused in the center with the underlying tissue; the periphery of the scale is raised. When patients bite off the scales, a stagnant-hyperemic surface without erosion is exposed. The disease lasts in this form for a long time. However, exacerbations of the disease and the transition of the dry form to the exudative form may suddenly occur [74, 76].
Exfoliative cheilitis, exudative form
. The clinical picture is characterized by severe swelling of either one or both lips. The lower lip is most often affected. On examination, the lip is enlarged, the mouth is half-open, the red border of the lips is bright red, covered with a large number of wet scales and crusts, saturated with yellowish-gray exudate. With significant effusion, the crusts can form a continuous mass that hangs like an apron from the red border to the chin. The pathological process is localized only at the border of the red border (from the Klein zone to the middle of the red border), without affecting the skin of the lip and chin. The monomorphic process (absence of crusts, vesicles and erosions) distinguishes this cheilitis from the eczematous process [7].
Glandular cheilitis.
Glandular cheilitis clinically occurs in 2 forms: simple and purulent. The causes of the disease are: irritation of the oral mucosa (MOR) by sharp edges of the teeth; pathological bite (protrusion of the frontal group of teeth of the upper jaw); incorrectly placed prostheses, as well as hypertrophied excretory ducts of the minor salivary glands (MSG) [13, 54].
The clinical picture of simple glandular cheilitis is characterized by dilation of the mouths and excretory ducts of the salivary glands in the form of red dots, from which drops of saliva are released (“dew symptom”). The excretory openings of the minor salivary glands are usually located on the mucous membrane of the lips and transitional folds, but with glandular cheilitis they can also be located in the Klein zone, less often on the red border of the lips. With significant salivation, limited inflammation of the red border with the phenomenon of eczema is possible [61].
Purulent glandular cheilitis was described by Volkmann in 1870, but currently does not occur in clinical practice [68].
Actinic cheilitis
. Actinic cheilitis is one of the symptoms of dermatoses in people with increased sensitivity to sunlight. The causes of actinic cheilitis are prolonged and intense sun exposure in combination with meteorological factors (constant work outdoors, wind, frost) [12, 78]. Quite often, actinic cheilitis is observed in patients together with other allergic conditions such as solar prurigo (erythema on the facial skin) [55].
Clinically, eczematous and xerotic forms of actinic cheilitis are distinguished [46, 80]. The eczematous form of actinic cheilitis is a type of acute allergic contact dermatitis with characteristic manifestations [71]. The red border of the lower lip is most often affected. The lips become swollen, and bright red spots appear on the red border. In some cases, against this background, small bubbles appear that quickly open; in their place there remain defects in the red border of the lips. Crusts, scales, and cracks may appear [51]. Patients complain of itching, burning, and soreness in the lip area. In making a diagnosis, the determining role is played by identifying the seasonality of the manifestations of the disease and the long-term wave-like course [34, 53].
The dry form of actinic cheilitis is similar in its manifestations to the dry form of exfoliative cheilitis, resulting in diagnostic difficulties in some cases.
Abrasive precancerous cheilitis Manganotti
.
A.L. Mashkilleyson classifies Manganotti cheilitis as an obligate precancerous disease of the oral cavity. The causes of the disease are unknown. Some authors [49] assign a leading role in its occurrence and development to long-existing herpetic eruptions on the lip and exposure to insolation.
Abrasive precancerous Manganotti cheilitis occurs only on the lower lip and is characterized by the appearance of one or more oval, or less often irregular, erosions on the red border. The erosion surface is smooth and red. Since the erosion is superficial, it gives the impression of an abrasive (scraped) surface. In many patients, erosions are covered with a dark red crust. More often, erosion is located on the side surface of the lip, less often - in the center and extremely rarely - in the corners of the mouth. Inflammation of surrounding tissues may periodically disappear. Long-term existence of erosion (according to some data, up to 2 years) and spontaneous epithelialization are also possible [25].
Clinical signs of the possible transformation of abrasive precancerous cheilitis into cancer are compaction at the base and around the erosion, its bleeding with mild trauma, papillary growths and keratization of the surrounding tissue.
Diagnosis of abrasive precancerous cheilitis is based not only on the clinical picture, but also on cytological and histological examination in order to detect atypical cells and select a method of further treatment. Patients with abrasive precancerous cheilitis of Manganotti are subject to dispensary observation.
Diagnostics
The diagnosis of precancerous Manganotti cheilitis is usually made based on an external examination of the affected area and questioning the patient about the nature of the disease. In case of difficulties that may arise due to the similarity of the manifestations of this type of cheilitis with erosive and ulcerative forms of other diseases (herpes, leukoplakia, lupus erythematosus, lichen planus), analysis of scrapings from the damaged area of the lip will help. In addition, histological examination makes it possible to timely recognize the formation of cancer cells.
Treatment
In the advanced stage, Manganotti cheilitis is very difficult to treat with medications. However, if it is detected in the early stages, the prognosis for the patient is favorable. If you notice typical symptoms of this type of cheilitis, contact your dentist. Perhaps he will refer you for additional consultation with an oral and maxillofacial surgeon to eliminate factors traumatic to the lip.
Treatment of the disease begins with thorough sanitation of the oral cavity. In parallel with the treatment, the doctor prescribes the patient a gentle diet, consisting of fresh and lightly salted foods, rich in vitamins and minerals. Being in the open sun, much less smoking, is strictly contraindicated for such patients.
Treatment of Manganotti cheilitis consists of a course of taking multivitamins, theonicol and methyluracil, as well as an oil solution of vitamin A. The course of treatment usually lasts at least a month. It is recommended to constantly lubricate the lips themselves with retinol acetate or sea buckthorn oil. For more serious injuries, the doctor may prescribe corticosteroid ointments or even surgical removal of the inflammation. If cancer cells are detected in a biosample, surgery is an emergency measure to prevent further spread of the tumor.
dentist.org
Abrasive precancerous cheilitis Manganotti (cheilitis abrasiva praecancerosa Manganotti) is a disease characterized by the appearance of one, or less often several, erosions on the red border of the lower lip. Typically, erosion is located on the lateral parts of the lip, less often in the center or at the corner of the mouth. It has an oval or irregular shape with a smooth, seemingly polished surface, deep red in color (Fig. 11.62). The erosion is located superficially, sometimes covered with a dense bloody or serous crust, which is difficult to remove, and slight bleeding occurs. Erosions that are not covered with crusts do not tend to bleed. There is usually no compaction of tissue at the base and around the erosion. Erosion with Manganotti cheilitis is usually painless or mildly painful. Sometimes they occur against the background of minor inflammation, which is unstable. Erosion is characterized by a sluggish and persistent course and does not respond well to drug therapy. They can exist for a long time, sometimes spontaneously epithelialize, but after some time they appear again in the same or other places. The period of epithelization of erosions with Manganotti cheilitis can vary from 3 months to 2 years.
Rice. 11.62. Haylit Manganotti. Red erosion with a smooth surface on the unchanged red border of the lower lip.
The duration of abrasive pre-cancer Manganotti cheilitis before its transformation into cancer is individual. Rapid malignancy of the process may occur (after 4-6 months); in some patients it occurs 5-7 years after the onset of the disease. Clinical signs indicating the possible onset of transformation into cancer are the appearance of compaction at the base and around the erosion, papillary growths on its surface, bleeding after mild trauma, keratinization around the erosion. Histological examination reveals an epithelial defect (Fig. 11.63). The epithelium at the edges of the erosion is usually in a state of acanthosis; wide epithelial outgrowths are deeply embedded in the underlying stroma. The cells of the spinous layer are in a state of varying degrees of discomplexation and atypia. The stroma contains a diffuse infiltrate consisting of lymphocytes, plasma cells, and histiocytes. Cytological examination can reveal the phenomena of dyskaryosis of epithelial cells, elements of inflammation, but more often only inflammation is detected.
Rice. 11.63. Pathohistology of Manganotti cheilitis. Violation of the integrity of the epithelium, inflammatory infiltration in the underlying mucous membrane. The integrity of the basement membrane is not traced. The epithelium at the edges of erosion is in a state of acanthosis.
Differential diagnosis. Abrasive precancerous Manganotti cheilitis should be distinguished from: ? erosive form of leukoplakia; ? erosive form of lichen planus; ? erosive form of lupus erythematosus; ? pemphigus; ? actinic cheilitis; A multiform exudative erythema; ? herpetic erosions; ? lip cancer Treatment. For Manganotti cheilitis, treatment consists primarily of eliminating local traumatic factors. Sanitation of the oral cavity is carried out, including rational prosthetics. It is strictly forbidden to smoke, eat irritating foods, and avoid exposure to insolation. An examination is necessary to identify and treat concomitant general somatic diseases. If histological examination does not reveal signs of malignant Manganotti cheilitis, then general and local conservative treatment can be carried out for no more than 1-2 months. Vitamin A is prescribed orally (3.44% solution of retinol acetate in oil or 5.5% solution of retinol palmitate in oil) 10 drops 3 times a day, multivitamins. Local applications are carried out with an oil solution of vitamin A, in the presence of background inflammatory phenomena, ointments with corticosteroid drugs and antibiotics, solcoseryl, etc. If there is no effect from conservative therapy, surgical treatment is performed - removal of the lesion within healthy tissues, followed by histological examination.
Prevention
In order to avoid encountering this unpleasant disease, patients at risk are recommended to:
- be examined by a dentist at least once every six months and promptly remove sharp edges of teeth, tartar, and damaged dental crowns that injure the lip;
- dentures should be made only from high-quality materials to suit the individual characteristics of the patient’s jaw apparatus;
- give up bad habits that destroy your health;
- do not stay in the sun for a long time, use protective equipment, including oil-based lipstick;
- pay attention to and begin treatment of chronic diseases of the gastrointestinal tract, endocrine system, internal organs;
Follow a diet that excludes salty, spicy, sour and spicy foods, as well as very hot foods and drinks.
Abrasive precancerous cheilitis Manganotti
In the prevention of precancerous diseases of the oral mucosa and the red border of the lips, paramount importance belongs to the elimination of chronic factors that injure the mucous membrane (sharp edges of teeth, dentures, tartar deposits, damaged tooth crowns, galvanism phenomena), the fight against smoking, and protection from excessive insolation and drying . An important link in the prevention of precancerous diseases of the red border of the lips is the timely treatment of systemic diseases and chronic inflammatory processes of the oral mucosa - chronic lip cracks, glandular cheilitis, chronic herpetic lesions, etc.
A major role in the prevention of precancer and cancer of the oral mucosa and red border of the lips is played by mass sanitary education work among a healthy contingent of people, as well as among patients seeking help from a dentist. In conversations with patients, you should pay attention to the dangers of eating hot, scalding and overly spicy food, as well as the dangers of drinking alcohol and smoking.
It is necessary to pay attention to oral hygiene, which is one of the links in preventing the occurrence of precancerous changes in the oral mucosa. This topic should be discussed especially seriously with patients who already have precancerous diseases. Patients should be warned about the likelihood of cancer if they do not comply with the necessary doctor's instructions (stop smoking, eat irritating foods, regularly take care of the oral cavity).
Dentists, just like doctors of any other profile, must exercise oncological vigilance when examining patients. Regardless of the complaints with which the patient came, a thorough examination of the entire oral cavity and the red border of the lips is the law for the doctor. Any deviation from the norm in the oral cavity should attract the close attention of a doctor. Early manifestations of precancerous diseases or signs of their transformation into cancer are usually invisible to the patient because they are painless, so it is the doctor’s duty to diagnose them in a timely manner. The concept of “oncological alertness” primarily includes the sum of specific knowledge of oncology, which allows the doctor to conduct an early and timely diagnosis of cancer. This concept also includes knowledge of precancerous diseases and signs of malignancy, their diagnosis, and treatment. In making a diagnosis and identifying morphological signs of malignancy, the cytological method of research plays a primary role, allowing a correct diagnosis to be made in 90-95% of cases. Material for cytological examination is taken by scraping or puncture. In patients with obligate and facultative forms of precancer with a greater potential for malignancy, it is necessary to conduct a histological examination. The question of the precancerous nature of the lesion is decided on the basis of a complex of clinical and morphological signs.
Patients with precancer of the mucous membrane of the mouth and lips, especially its obligate forms, should be under the active supervision of a dentist or oncologist. The dentist must have a clear understanding of the organization of oncological care and the network of oncological treatment institutions in order to quickly refer the patient to his destination. In difficult diagnostic cases, it is necessary to remember the possibility of rapid growth of a malignant tumor and make a diagnosis as soon as possible. Treatment without diagnosis should not last more than 7 days.
Local irritants should be eliminated and agents that promote tumor growth (cauterization, physiotherapy) should not be used. In difficult cases, the doctor is obliged to involve more experienced specialists in examining the patient.
At the slightest suspicion of malignancy of a precancerous process, it is necessary to urgently excise the lesion within healthy tissues, followed by histological examination. Only after this should the question of further treatment tactics be decided. After treatment for cancer or precancerous lesions, patients should be closely monitored.