Glossalgia is a secondary manifestation of a number of diseases and manifests itself in the form of painful sensations in the tongue area. The patient may experience burning, pinching, tingling and other unpleasant symptoms. Symptoms are not related to external stimuli or food intake. Upon examination, the mucous membrane of the tongue is not changed, has a physiological color, and is free of damage. The pain can be quite intense and usually occurs for no apparent reason. Taking painkillers provides only a short-term effect. To radically solve the problem, it is necessary to identify and eliminate the main cause causing these clinical manifestations.
According to ICD-10, glossalgia is one of the manifestations of glossodynia, which is a pathology of a neurological nature.
Causes of glossalgia of the tongue
It has been noticed that glossalgia appears after traumatization of the tongue by foreign sharp objects, incorrectly installed fillings, implants or prostheses. Also, its symptoms are often associated with disorders of the autonomic nervous system. Due to further irritation of the mucous membrane, the disease becomes chronic. Scientists have not established the organic causes of glossalgia.
Among the provoking factors, doctors name:
- liver diseases;
- diseases of the gastrointestinal tract;
- vascular lesions combined with diseases of the central and peripheral nervous system, functional disorders;
- malfunctions of the nervous system.
According to reviews, glossalgia can occur as a result of neurosyphilis, encephalitis, hemorrhagic and ischemic stroke. It can also be a symptom of viscero-reflex bulbar syndrome, which is characterized by damage to the vagus and glossopharyngeal nerves.
Etiology and pathogenesis
The etiology and pathogenesis have not been fully elucidated. The observations of A. G. Zhukova (1972) and the clinical and experimental studies of E. S. Yavorskaya (1974) made it possible to identify some specific links in pathogenesis, which gave them the basis to differentiate glossalgia from glossodynia. However, most authors continue to consider the terms “glossalgia” and “glossodynia” to be synonymous. A.G. Zhukova and E.S. Yavorskaya believe that in the genesis of glossodynia the leading place belongs to organic and functional disorders of various parts of the c. n. pp.—sensitive and motor nuclei of the pontobulbar part of the brain stem, bulbospinal nuclei of the trigeminal nerve, reticular formation of the medulla oblongata; The genesis of glossalgia is more characterized by dysfunction of the sympathetic and parasympathetic parts of the nervous system. Changes in the nervous system are often accompanied by visceral pathology; at the same time, the frequency of detection of diseases of the digestive organs in patients with glossalgia and glossodynia is explained by the anatomical and functional connection of the nucleus of the vagus nerve innervating the gastrointestinal tract. tract, with the nucleus of the trigeminal nerve.
What are the symptoms of glossalgia?
With glossalgia, patients complain of:
- burning and tingling sensation in the tongue area;
- dry mouth;
- pain in the mouth.
The discomfort caused by the disease is permanent or periodic. It may intensify after eating spicy food or prolonged conversations. In some patients, while chewing non-spicy food, the pain, on the contrary, goes away.
If glossalgia is left untreated, symptoms may disappear and reappear. However, it is usually not possible to establish the causes of their occurrence. Changes in the mucous membrane of the tongue and oral cavity are not detected in the described pathology. Only 5% of patients experience:
- swelling of the mouth;
- coating of the tongue with a white or yellowish coating;
- hypertrophic changes in the papillae of the tongue.
During palpation, patients experience acute pain. Constant discomfort and the inability to talk, eat, drink normally have a negative impact on the emotional sphere. Some patients with symptoms of glossalgia become depressed, become too suspicious and apathetic, and suffer from insomnia.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
Clinical manifestations of glossalgia
The leading symptom is pain, burning of the tongue. Usually these sensations occur in its lateral parts and at the tip. Clinical manifestations may occur periodically or haunt the patient almost constantly. They are not associated with any damage and occur spontaneously.
Many patients note that the clinical picture of the disease manifests itself under stress, at the time of nervous overstrain, and with severe anxiety. When eating, discomfort usually decreases or disappears altogether.
The disease is recurrent. The pain may disappear for a long time and then suddenly appear again.
Many patients complain of dryness of the oral mucosa. During the conversation, they feel quickly tired; with severe symptoms, speech may be difficult.
A characteristic symptom is a decrease in pain sensitivity in the affected areas of the tongue. A functional disorder leads to the fact that in the absence of a stimulus, the central nervous system receives a false signal about the influence of a damaging factor, but in the real presence of one, the impulses are blocked. This can lead to secondary trauma to the tongue.
The psychological portrait of a patient with glossalgia is quite typical. These are people who are excitable, react inadequately to the surrounding reality, show excessive concern about their condition, and show groundless aggression. When talking about their problem, they may describe their condition biasedly and talk about symptoms that are actually absent. During the conversation, it is possible to find out that such patients suffer from sleep disorders, nightmares, depression or other mental disorders.
Many patients with glossalgia sincerely believe that they suffer from a serious, incurable disease, such as cancer. When diagnosed with glossalgia, they question the doctor’s competence, refuse treatment and go to see another specialist, leaving a negative review about the previous one.
Diagnosis of glossalgia of the tongue
Diagnosis of glossalgia is aimed at differentiating the disease from conditions that have similar symptoms, such as:
- pathological bite syndrome;
- initial stage of osteochondrosis of the cervical spine;
- tongue injury;
- neuralgia;
- neuritis.
The main difference between glossalgia and organic lesions is the discrepancy between the painful sensations and the intensity of the impact. In addition, the doctor draws attention to the fact that changes in the mucous membrane of the oral cavity and tongue are almost completely absent.
With neuralgia, the pain is short-term and localized specifically in the area of a specific nerve. With glossalgia, they are diffuse in nature, since we are talking about inorganic damage to the vagus nerve.
Glossalgia differs from neuritis in that the pain is distributed throughout the entire oral cavity. It's not one-sided. At the same time, tactile sensitivity does not disappear completely and does not increase during chewing of food.
Clinical signs
Patients' complaints and the intensity of subjective sensations vary widely. Paresthesia of the mucous membrane of the cheeks, palate, lips, skin of the infraorbital and chin areas is often associated. Taste sensitivity may be reduced, and taste may be distorted. Paresthesia has a depressing effect on the psyche of patients, and some of them develop cancerophobia. G., as a rule, affects people over 40 years of age and more often women.
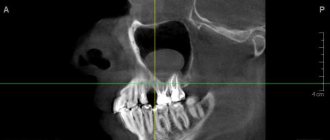
Predisposing and provoking factors can be caries, incorrectly placed fillings and dentures, tartar, galvanic currents with dentures made of dissimilar metals, tongue injury, irritating foods, and some medications.
G. develops gradually. Initially, the phenomena of paresthesia are short-lived; Over time, the attacks are repeated, their intensity and duration increase, especially in the evening, after a long conversation, in stressful situations. The intensity of paresthesia is disproportionate to changes in the mucous membrane of the tongue. The mucous membrane of the tongue, if G. does not accompany glossitis (see), is initially not changed, but sometimes there is a slight atrophy of the papillae of the tongue and hyperplasia of lymphatic follicles. Gradually, one can detect hypertrophy of the leaf-shaped and grooved papillae, swelling, dilation of the veins on the lower surface of the tongue, and decreased salivation.
G.'s phenomena can last in some cases for months, in others for years; sometimes remissions occur without treatment, but after a certain time an exacerbation occurs again.
How to cure glossalgia
Treatment for glossalgia depends on the cause of the disease. It may consist of:
- sanitation of the oral cavity;
- replacement of poorly installed dentures, allowing the formation of a correct bite.
The patient is also recommended to consult with a gastroenterologist, neurologist and endocrinologist, and talk with a psychologist.
Pathogenetic therapeutic measures for glossalgia consist of influencing the central and peripheral parts of the pain symptom and normalizing homeostasis. For this, the patient is prescribed:
- valerian;
- bromine preparations;
- mild tranquilizers (“Phenazepam”);
- B vitamins;
- trimecaine blockade of the lingual nerve (allows you to completely restore the functions of the affected nerve);
- iron preparations (“Gemostimulin”, “Ferroplex”, “Ferrocal”);
- local anesthetics;
- mouth baths;
- treatment of painful areas with vitamin A and rosehip oil.
Also, for a speedy recovery from glossalgia, the following can be used:
- hypnosis (hypnotic sleep);
- reflexology;
- physiotherapy.
Surgeries are not performed for glossalgia. Usually, patients manage to get rid of an unpleasant illness with the help of medications, folk recipes and physiotherapeutic procedures.
Possible complications
This disease does not threaten health, but significantly reduces the quality of life.
If you ignore an unpleasant symptom, glossalgia can become chronic. Its symptoms will occur from time to time, exacerbating the unstable psycho-emotional state.
Against the background of pain, anxiety, eating disorders, sleep disorders, nervousness, and phobias can develop.
As the condition worsens, treatment should be carried out not only by the dentist, but also by other specialists - a neurologist, psychiatrist or psychotherapist.
A long-lasting symptom can cause forced dietary restrictions, which can affect the overall health and cause vitamin deficiencies, weight loss, and lack of minerals.
Possible complications include inflammatory diseases of the oral cavity.
For example, a lack of saliva can lead to canker sores.
, and when exposed to unfavorable factors or injuries, the likelihood of
glossitis, gingivitis
and other
ailments
increases.
Prevention of glossalgia
Prevention of glossalgia involves regular examination of the oral cavity and an annual visit to the dentist. Important:
- timely restoration of damaged teeth and treatment of caries;
- install only high-quality prostheses;
- brush your teeth twice a day;
- Periodically rinse your mouth with herbal decoctions and special antiseptic solutions.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Causes
External causes of glossalgia symptoms include tongue injury. You can get such an injury when eating nuts, chips, crackers. It is quite easy to scratch the surface of the tongue with such products. It can also be burned by hot drinks or strong alcohol. Many patients suffering from chronic glossalgia notice that signs appear when they experience stress for a long time or face problems at work or in their personal lives. From this, experts conclude that the disease is psychological in nature. Glossalgia is often observed in people diagnosed with vegetative-vascular dystonia. There are a number of diseases of the human body systems that are accompanied by chronic glossalgia. These include:
- gastrointestinal infections, for example gastritis;
- diabetes;
- hypothyroidism, leading to dysfunction of the thyroid gland;
- advanced stages of syphilis. The disease first affects the skin and mucous membranes, then the internal organs. A special form of the disease is neurosyphilis, in which Treponema pallidum affects the components of the human nervous system;
- encephalitis of any origin. There are allergic, infectious and other encephalitis. The disease is often associated with tick bites;
- cardiac ischemia.
It is known that signs of glossalgia are often observed in people with weakened protective functions of the body. Permanent trauma to the tongue due to improperly sized dentures, braces, fillings, or a chipped tooth leads to increased symptoms of the disease.
Diagnostic measures
It is important to correctly diagnose in order to distinguish between glossalgia and other language pathologies that develop due to trauma, increased pain and sensitivity of the nerves. The specialist will perform a visual and instrumental examination of the oral cavity to assess the bite relationship. The main thing is to determine the difference in sensitivity and strength of impact.
In case of trauma, pain sensations are clearly located. With nerve pain, the pain quickly disappears at the point where the nerve passes. In inflammatory processes - on the one hand, and with a change in reactivity.
Glossalgia is a pathological condition characterized by paresthesia and pain in the tongue without any visible changes. When paresthesia spreads to other areas of the mucous membrane of the mouth, pharynx, and pharynx, the disease is called stomalgia. Typically, middle-aged and elderly people with pronounced neuropsychic changes suffer from glossalgia (stomalgia). Women get sick 5-6 times more often than men. The disease most often begins after trauma to the tongue with a sharp edge of a tooth, a denture, after tooth extraction, or stress. Patients complain of burning, tingling, rawness, a feeling of pepper on the tongue, a feeling of heaviness in the tongue, intensifying towards the end of the day, and dry mouth.
A characteristic diagnostic sign for glossalgia is the absence of unpleasant sensations while eating. This is explained by the anatomical proximity of two nuclei in the central nervous system. The nucleus, which models chewing movements, is located in the pons. Very close to it is the nucleus of the trigeminal nerve. More powerful excitation comes from the nucleus of the masticatory muscles, which suppresses the impulse of the sensory nucleus of the trigeminal nerve.
In the pathogenesis of the disease, the main role belongs to the pathology of the autonomic nervous system, which is supported by irritation of the neuro-reflex circuit at its various levels. These disorders are usually functional in nature. The disease lasts for years. The longer the course of the disease, the more severe the clinical picture and the more difficult the treatment. Against this background, patients often experience neurotic conditions, cancerophobia, and syphilophobia.
The purpose of the study is to find ways to improve the effectiveness of treatment for elderly patients suffering from glossalgia, stomalgia and hyposalivation.
Material and methods.
We examined 11 patients aged from 65 to 86 years (2 men, 9 women) diagnosed with glossalgia (9), stomalgia (2). Hyposalivation was observed in all patients examined. All patients complained of burning, tingling of the tongue, and a feeling of dry mouth. Patients of the examined age category, as a rule, constantly take several medications per day (antihypertensive, sedatives, blood thinners). All these medications also cause, to some extent, inhibition of the salivary glands and hence dryness.
Most patients reported suspiciousness, anxiety, and poor sleep. On examination: anxious facial expression. The height of the lower part of the face is often reduced. When examining the tongue, dryness and moderate atrophy of the filiform papillae were revealed. The hygienic condition of the oral cavity is unsatisfactory, dental plaque, sharp edges of the teeth, pathological abrasion of the teeth.
Diagnoses were made: glossalgia (stomalgia), hyposalivation, anxiety-depressive syndrome. The diagnosis was based on clinical characteristics, namely: complaints, medical history, external examination and examination of the oral cavity.
After obtaining informed consent and consulting a psychoneurologist, all patients underwent a course of general and local treatment.
General treatment: psychotropic drugs, stimulation of salivation, massage of the collar area, a course of intramuscular injections of the drug Milgamma, treatment of concomitant diseases by specialists.
Local treatment: correction of oral hygiene, professional hygiene, grinding of sharp edges of teeth and orthopedic structures, bilateral blockades of the lingual nerves. For blockades, a 6% solution of thiamine bromide with a 2% solution of lidocaine was used. The course is at least 5 blockades.
To eliminate dryness in the oral cavity, an aqueous 2% solution of pilocarpine hydrochloride was used. Prescribed 5-6 drops of pilocarpine with water 30 minutes before meals 3 times a day for a long period. After 7-10 days, dry mouth disappeared.
The use of aloe mouth rinse, spray and gel also helped relieve dryness, providing a moisturizing effect. After meals three times a day, the tongue was treated with Cholisal gel, which contributed to the disappearance of paresthesia.
Results.
After 2 months of treatment, all 11 patients’ complaints disappeared, sleep normalized, anxiety and psycho-emotional stress went away.
Conclusion.
Our study showed that recovery of patients with glossalgia, stomalgia and hyposalivation against the background of anxiety-depressive syndrome is possible with complex and qualified treatment. Treatment of elderly patients with these diagnoses requires appropriate correction.
Treatment
If glossalgia is not treated, it can progress over months and even years with periodic periods of remission, which after some time will be replaced by exacerbations. Occasionally, glossalgia occurs on its own without additional medical intervention. Initially, after the patient visits the doctor, it is necessary to organize a complete sanitation of the oral cavity, including prosthetics and treatment of malocclusion. Pain is relieved with local anesthetic medications. First of all, you need to find out what caused the disease. If it is caused by injuries in the oral cavity, then it will be necessary to eliminate the original causes of the injury, that is, replace dentures or dental fillings, polish sharp edges, etc. If the cause of the development of glossalgia is another pathology, then it is important to visit an appropriate specialist to relieve it. In the treatment of glossalgia, various keratoplasty medications are often used, for example, rosehip oil, as well as medications that help increase saliva production when severe dry mouth occurs. In accordance with the clinical picture of the pathology, sometimes during the entire treatment sessions of hypnosis, psychotherapy and physiotherapeutic procedures such as electrophoresis, electrosleep, iontophoresis and others can be implemented.