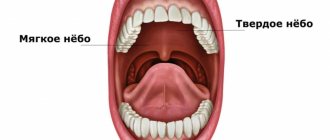
If you go to the mirror and open your mouth wide, you can see two formations that are located on the side surfaces, in the depths of the pharynx, which are shaped like an almond. This is why the tonsils are called tonsils. And since the tonsils are located in the soft palate, they are called palatine tonsils.
Also, in common parlance, the palatine tonsils are also called tonsils. They are one of the important organs of the pharyngeal immune system and form an important part of the Pirogov-Waldeer lymph-epithelial pharyngeal ring.
Palatine tonsil, tonsila palatina. It is located in the tonsillar fossa between the palatoglossus and velopharyngeal arches.
Make an appointment right now!
Call us by phone or use the feedback form
Sign up
What other tonsils are there in the pharynx?
Other tonsils that form the lymphoid pharyngeal ring are: adenoid vegetations, or, more simply, adenoids, which are not a paired organ. They are located in the dome of the nasopharynx. It is impossible to see them with the naked eye. In order to recognize the condition of the adenoids, it is necessary to perform an endoscopic examination of the nasopharynx. Inflammation of the adenoids is called adenoiditis and is more common in children.
Also in the pharynx there is a lingual tonsil, located at the root of the tongue, which, like the adenoids, is an unpaired organ.
There are also tubal ridges, which are also called tubal tonsils. They are located at the entrance to the pharyngeal mouth of the auditory tube. The tube ridges are located deep in the nasopharynx, on the lateral (medial) surfaces of the nasopharynx on the right and left. Tubal tonsils perform an important function - they protect against infection entering the auditory tube. Since each of the tonsils of the lymphoepithelial pharyngeal ring deserves separate close attention, in this article we will only talk about the palatine tonsils and chronic tonsillitis. Other tonsils and the pathology they cause will be described in detail separately, in other relevant ENT articles.
What are the indications for adenoid removal (adenotomy)?
Adenotomy
- Cost: 50,000 - 80,000 rubles.
More details
- Poor nasal breathing during the period when the child is healthy. This is dangerous because the child’s body experiences hypoxia (oxygen starvation). Insufficient oxygen supply to the body can lead to a delay in the psychomotor development of the child; the child may be adynamic, or, conversely, hyperactive. Due to the fact that the child constantly breathes through his mouth, the facial skeleton (adenoid face) is formed incorrectly. The quality of life of such children certainly suffers.
- Hearing loss or frequent inflammation in the ears are also direct indications for adenotomy. The mechanism of occurrence of this pathology occurs as follows. Where the adenoids are located, there is the mouth of the auditory tube (Eustachian tube) - an organ that connects the middle ear (what is located behind the membrane) and the nasopharynx itself. If, with your mouth closed, you pinch the tip of your nose and exhale into your nose, then air will enter your ears due to this very organ. Due to the close anatomical location of the adenoids and the auditory tubes, the inflammatory process from the adenoids can move to the mouth of the auditory tubes, causing in turn inflammation and, as a consequence, dysfunction of the auditory tube. In addition to the chronic inflammatory process in the auditory tubes, when adenoids grow, they can cover the mouths of the auditory tubes, leading to the development of adhesive otitis media or the formation of exudative otitis media (fluid in the middle ear). Frequent purulent-inflammatory phenomena in the cavity of the middle ear (sound transmitting apparatus) lead to the formation of adhesions and scars between the auditory ossicles, which subsequently leads to hearing loss in adulthood. In these cases, between the organ of hearing and the natural filter in the form of adenoids, we choose the organ of hearing.
- It is also necessary to part with adenoids if the child often suffers from adenoiditis, which, with local treatment, does not produce significant positive dynamics, but only leads to recovery for a short period of time. This is a consequence of the fact that the adenoids do not carry out their immune function, they have worn out themselves as a natural filter, are a source of chronic infection and need to be sanitized (removed). Adenoiditis can also often be associated with herpes viral infection (Epstein-Barr virus, cytomegalovirus, type 6 virus), which live in the lymphoid tissue, leading to a decrease in immunity, including local immunity. If your child suffers from ARVI more than 6 times a year, there is cervical lymphadenitis (enlarged lymph nodes), conservative treatment of adenoiditis helps for a short time, in this case you need to contact a pediatrician for further examination for a herpes viral infection. When this group of viruses is detected, adequate treatment is prescribed, and if positive dynamics are observed in the adenoids during therapy, the child should be observed and there is no need to rush into surgery.
But if, together with treatment from a pediatrician, no effect is observed, then, according to the law of surgery, the tissue that prevents a person from living is removed.
Read more about tonsils
It must be said that the palatine tonsils are the largest lymphoid formations of the entire pharyngeal ring, and they play, perhaps, the leading role in the disposal of bacterial and viral infections that enter the pharynx by airborne droplets.
Due to their size, the palatine tonsils are the first to stand in the way of microbes that enter the oral cavity from the external environment, and protect the body from infection by viruses, bacteria, spirochetes, protozoa and other microorganisms.
The palatine tonsils have depressions - lacunae, which in turn are exit holes for deep and sharply convoluted canals - crypts, which are located in the thickness of the palatine tonsil, leading to its root. The number of lacunae and crypts can vary from 1 to 14, but on average, in each amygdala there are from 4 to 7 lacunae. The diameter of the lacunae can also vary, depending on gender, age, individual characteristics of the patient, as well as the duration and severity of the disease and the presence of scar changes in the tonsils themselves.
It is believed that the wider the exit hole - the lacuna - the higher the likelihood of the palatine tonsil to self-cleanse. This statement is true. Accordingly, the smaller the diameter of the lacuna, the more pronounced and severe the tonsillitis. Moreover, if the tonsil produces a large amount of caseous-necrotic detritus (plugs), the severity of the course also noticeably increases.
Normally, on the mucous membrane of the palatine tonsils, as well as in the thickness of the palatine tonsils, in the lacunae and crypts, there is a growth of non-pathogenic and conditionally pathogenic microflora, in normal (permissible) concentrations. If there are more microorganisms (for example, due to intensive growth, or the addition of other pathogenic microflora from the outside), the palatine tonsil immediately destroys and utilizes the dangerous infection and normalizes a dangerous condition for the body. At the same time, the macroorganism, that is, the person, does not notice this in any way.
The tissues of the palatine tonsils produce the following main protective substances: lymphocytes, interferon and gamma globulin.
The palatine tonsils act as a serious infectious and inflammatory barrier and are an important component in creating not only local, but also general immunity in the human body. Therefore, when it comes to removing the palatine tonsils, you first need to think ten times, weigh the pros and cons, and only after that make a decision about removing the tonsils.
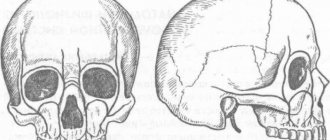
Anatomy
Palatal
The tonsil is a paired formation located in the fossa of the tonsils (fossae tonsillares) of the lateral walls of the pharynx between the palatoglossus arch (areus palatoglossus) and the velopharyngeal arch (areus palatopharyngeus). It has an oval shape, its long axis runs from top to bottom and somewhat from front to back. In a newborn, the size of the palatine m. in the vertical direction is 10 mm, in the transverse direction 9 mm, thickness 2.1 mm; in an adult, respectively, 15-30 mm, 15-20 mm, 12-20 mm. In the palatal M., two surfaces are distinguished: internal (free) and external, facing the wall of the pharynx. The inner surface is uneven, covered with a mucous membrane, has 8-20 irregularly shaped tonsillar dimples (fossulae tonsillares), which are the mouths of tonsillar crypts (cryptae tonsillares), which, branching, penetrate the thickness of the palatine membrane. The crypts increase the free surface area of each palatine membrane up to 300 cm2. When swallowing, the palatine membranes are slightly displaced, and their crypts are freed from their contents. The outer surface of the palatine membranes is covered with a capsule (capsula tonsillae) up to 1 mm thick; on it lies a layer of loose paratonsillar tissue, the edges go down to the root of the tongue, in front it communicates with the tissue of the palatoglossal arch, at the top - with the submucosa of the soft palate. In an adult, the distance to the internal carotid artery from the upper pole of the palatine M. is 28 mm, from the lower pole 11-17 mm, to the external carotid artery 41 mm and 23-39 mm, respectively. The upper corner of the M.'s fossa remains free and is called the supratonsillaris fossa. Sometimes there is an additional palatine M.—the palatine lobe of the palatine M., the edges of which can extend deep into the soft palate and not have a direct connection with the main palatine M. (Fig. 2). In these cases, it represents an additional intrapalatine M. (tonsilla intrapalatina accessoria), the edges usually contain a deep branched crypt - the sinus of Tourtuali, which plays a certain role in the pathology of the M.
Pharyngeal
M. (syn.: nasopharyngeal M., Lushka's tonsil, third M.) is located on the border of the upper and posterior walls of the pharynx (see), has the appearance of a round-shaped plate with 4-8 folds of the mucous membrane diverging on its surface, protruding into the cavity nasopharynx. The pharyngeal M. is well developed only in childhood; with the onset of puberty, its reverse development occurs.
lingual
M. (syn. fourth M.) is located in the region of the root of the tongue (see), occupying almost the entire surface of the root of the tongue. Its shape is often ovoid, the surface is uneven, and lingual follicles (folliculi linguales) are located on the mucous membrane, divided by grooves into a number of folds. M.'s crypts are shallow, at the bottom of many crypts the excretory ducts of the salivary glands open, the secretion of which helps to wash and cleanse the crypts. In a newborn, the lingual M. is well developed, its longitudinal size is 6 mm, transverse 9 mm. After 40 years, a gradual reduction of lingual M occurs.
Pipe
M. is a paired formation, which is an accumulation of lymphoid tissue in the thickness of the mucous membrane of the nasopharynx at the pharyngeal opening of the Eustachian tube (see Auditory tube).
In a newborn, the tubal M. is well defined, approx. 7.5 mm, diameter approx. 3.5 mm. Tubal M. reaches its greatest development at 5-7 years of age; later it gradually atrophies and becomes almost invisible. Rice.
3. Schematic representation of the blood supply to the palatine tonsil: 1 - external carotid artery; 2 - maxillary artery; 3 - descending palatine artery; 4 - ascending pharyngeal artery; 5 - ascending palatine artery; 6 - facial artery; 7 - lingual artery; 8 - superior thyroid artery; 9 - common carotid artery; 10 - internal carotid artery; 11 - palatine tonsil. The blood supply to the tonsils of the lymphoepithelial pharyngeal ring, including the palatine M. (Fig. 3), is carried out by arterial branches (aa. tonsillares), extending directly from the external carotid artery or its branches: the ascending pharyngeal (a. pharyngea ascendens), lingual (a. lingualis), facial (a. facialis), descending palatine (a. palatina descendens). M.'s veins are formed in the parenchyma, accompany the arteries and flow into the pharyngeal venous plexus (plexus venosus pharyngeus), lingual vein (v. lingualis), and pterygoid venous plexus (plexus venosus pterygoideus). M. does not have afferent lymphatic vessels. The draining lymphatic vessels flow into the lymph nodes: parotid, retropharyngeal, lingual, submandibular. M.'s innervation is carried out by the branches of the V, IX, X pairs of cranial nerves and the cervical part of the sympathetic trunk. In the subepithelial layer of connective tissue septa, M.'s parenchyma, there are individual nerve cells, their clusters, pulpy and non-pulpate nerve fibers, various types of nerve endings, and extensive receptor fields. The blood supply and innervation of the muscle change with age.
Chronic tonsillitis
Chronic tonsillitis is an autoimmune disease that occurs as a result of frequent sore throats and a decrease in the body’s overall resistance since childhood. With the development of the disease and its exacerbation, a person does not have enough general immunity to keep the palatine tonsils “in working order” and adequately fight the infection.
If harmful microbes get onto the surface of the mucous membrane and into the lacunae of the palatine tonsil, a real battle occurs between the microbes and the human immune system.
The palatine tonsil fights all pathogenic and conditionally pathogenic infections, but not being able to fully resist attacking microbes, it provokes either a new outbreak of sore throat or an exacerbation of chronic tonsillitis (treatment cannot be delayed in any case), thereby triggering an infectious-inflammatory process in palatine tonsils.
As a result of a lost fight, pus accumulates and stagnates in the lacunae of the tonsils, that is, dead leukocytes that come to the aid of the tonsil in the fight against a dangerous infection. The purulent masses irritate and inflame the tonsil tissue from the inside and have a toxic effect on it, thereby causing a sore throat - a severe infectious outbreak of inflammation of the tonsils.
In the absence of quick and adequate treatment, the contents of the lacunae and crypts of the palatine tonsils serve as a breeding ground for pathogenic microbes and a constant source of infection, even after an attack of tonsillitis.
What does a sore throat look like?
Signs of a sore throat are varied and depend on the disease. The diagnosis is made on the basis of a visual examination, examination of the patient’s complaints, and laboratory tests. There are distinctive signs of throat diseases that parents of children, especially, need to be aware of. This information is necessary to make a decision about urgent hospitalization or visiting a doctor at the clinic.
Angina
The first signs of a sore throat are redness of the tonsils, then the appearance of plaque. Purulent formations and necrotic changes may be present. During the inflammatory process, the lymph nodes enlarge. The accompanying symptoms of sore throat are severe intoxication and elevated body temperature. Follicular tonsillitis is accompanied by a loose plaque of a purulent nature on the tonsils. With necrotizing tonsillitis, gray dead areas are present, the palatine arches and the base of the tongue are affected. In the case of fungal tonsillitis, inflammation affects the tonsils, there is redness, looseness, and a yellow-green coating.
Pharyngitis
The disease causes damage to the mucous membrane of the larynx. Often appears in children as a result of exposure to viruses, fungi, allergens, and bacteria. In the catarrhal form, swelling of the larynx and redness are observed. With hypertrophic pharyngitis, enlargement of the pharyngeal tonsils is added to the listed symptoms. In the atrophic form, the vessels of the posterior wall of the larynx become more pronounced. In the case of granulosa pharyngitis, granules and clots of mucus are formed.
Candidiasis
Characterized by a pronounced fungal coating. The temperature remains normal, there are no complaints of sore throat. The main symptom is a cheesy layer on the palate and larynx, and less often on the tonsils. The condition may be accompanied by swelling and inflammation.
Adenoids
Children are most susceptible to the disease. Signs of adenoids are difficulty breathing through the nose, snoring at night, and hearing loss. It is quite difficult to independently assess their condition due to their location in the vault of the nasopharynx. A doctor can see the changes using a special mirror.
Diphtheria
A disease of infectious origin that affects the oropharynx. The throat becomes swollen, the tonsils are enlarged. A specific symptom is a filmy gray coating covering the larynx and tonsils. Diphtheria occurs with an increase in temperature to 39 degrees, inflammation of the lymph nodes, and swelling of the neck.
Laryngitis
The disease is accompanied by an inflammatory process in the laryngeal mucosa. The throat is bright red and there is swelling. Redness extends to the surface of the epiglottis. With laryngitis, there is an increase in blood vessels and the appearance of red dots (as a result of blood penetration). The patient has a hoarse voice, a barking cough that worsens at night.
Whooping cough
Whooping cough is a bacterial disease that is accompanied by an intense cough. The damage to the larynx is mechanical in nature; as a result of constant coughing, the mucous membrane is injured.
Scarlet fever
A specific symptom of the disease is the rich crimson color of the tongue. In the first days of the disease, a white coating and blisters are present, then the color changes. There is inflammation of the tonsils, and a rash appears on the surface. In severe cases of the disease, ulcers may appear on the surface of the tongue and throat.
Laryngeal papillomatosis
Caused by benign neoplasms. Papillomas are easy to see in areas of the larynx, sometimes they appear on the tonsils and lips.
In addition to visual symptoms, throat diseases also have other manifestations. It is important to seek medical help in a timely manner, especially when it comes to children. Some throat diseases can be fatal to a child. Using visual examination and laboratory tests, the doctor will establish a diagnosis and draw up a treatment plan.
Forms of the disease
- recurrent form, that is, with frequently recurring sore throats;
- protracted form, when the inflammatory process in the palatine tonsils is characterized by a sluggish and prolonged course;
- compensated form, when episodes of sore throat and exacerbation of tonsillitis are not observed for a long time.
Chronic tonsillitis is the most common disease among all diseases of the pharynx and one of the most common diseases of all ENT organs, along with such a diagnosis as acute sinusitis.
Chronic tonsillitis can affect both adults and children, from the moment the palatine tonsils begin to develop (from 2-3 years). Moreover, the incidence of this disease in childhood is much higher.
Some respiratory diseases can also be classified as social diseases. For example, sinusitis and tonsillitis are among them. Poor environment, stress, lack of sleep, overwork, monotonous and poor nutrition, as well as poor heredity are predisposing factors to the development of the disease.
Causes
The development of the disease is closely related to frequent sore throats (acute tonsillitis). Very often, incompletely cured tonsillitis leads to chronic tonsillitis. Very often, tonsillitis is an exacerbation due to the accumulation of plugs in the tonsils - caseous-necrotic masses, which are often confused with food debris.
Main reasons for development
- Unfavorable working conditions. The greatest influence is exerted by gas and dust levels in the air at work.
- Poor environmental conditions, pollution from vehicle exhaust gases, harmful emissions into the atmosphere.
- Low quality of consumed water.
- Weak (low) immunity.
- Severe hypothermia of the body.
- Stressful situations.
- The presence of chronic diseases in the nasal cavity, paranasal sinuses and oral cavity - dental caries, purulent sinusitis, etc., which often leads to infection of the tonsils.
- Irrational or poor nutrition, in which excess amounts of proteins and carbohydrates are consumed.
- Heredity (mother or father suffers from chronic tonsillitis). It is very important for a woman to undergo one or two courses of treatment for tonsillitis during pregnancy (depending on the severity of the process) in order to minimize the likelihood of the disease developing in the unborn child.
- Frequent overwork, fatigue syndrome, inability to fully rest.
- Smoking and alcohol abuse.
Removal of tonsils: pros and cons
The debate about the need to remove or preserve tonsils has been going on for a long time and with varying success. Those who advocate that nature does not deal with the structure of unnecessary organs give the following arguments about the benefits of the tonsils:
- Producing a huge amount of immunoglobulins, the tonsils of a healthy person contribute to the proper development and protection of the body from viral infections.
- The porous surface of the tonsils serves as a barrier to pathogenic microorganisms seeking to enter the throat and the internal environment of the body. Once in the center of the immune cells, the harmful bacteria die.
Proponents of surgery believe that even normal tonsils can eventually cause major health problems:
- During some diseases, for example, chronic tonsillitis or acute tonsillitis, disruptions and irreversible changes occur in the proper functioning of the lymphatic formations. The tonsils are constantly inflamed, do not allow you to breathe freely, and harmful bacteria are not eliminated.
- Frequent purulent sore throats can cause a throat abscess, a general infection of the body.
- Constantly enlarged tonsils lead to hearing impairment or deterioration of respiratory functions.
Most doctors agree with the removal of the tonsils in the most severe cases: when the body is unable to respond to medication treatment.
Symptoms
How to independently recognize chronic tonsillitis? Symptoms and treatment in adults and children can only be correctly determined by an ENT doctor. Below are characteristic signs - if you find them in yourself, consult a doctor.
The disease is characterized by symptoms such as:
- Headache.
- Feeling of something foreign in the throat, as if something was stuck in the throat. In fact, this is nothing more than large accumulations of caseous masses, that is, plugs in the thickness of the palatine tonsils.
- Increased fatigue, weakness, decreased performance. All this is due to the so-called tonsillogenic intoxication, or in other words, intoxication syndrome.
- Aching pain in the joints and muscles (with severe illness).
- Aching pain in the heart, with interruptions in heart function - extrasystole (with severe illness).
- Pain in the lower back, in the kidney area (with severe disease).
- Bad mood, and in some cases increased body temperature, and for a long time.
- Persistent skin rashes, provided that there was no previous skin pathology.
All these symptoms appear due to the entry of waste products of microorganisms into the blood from the palatine tonsils, i.e. staphylococcal and streptococcal infections, poisoning the entire body.
Bad breath appears due to the accumulation of organic substances and the decomposition of bacterial infection in the lacunae (recesses of the tonsils) and crypts (their canals). Tonsils become a source of bacterial infection, which can spread throughout almost the entire body and cause inflammation of the joints, myocardium, kidneys, paranasal sinuses, prostatitis, cystitis, acne and other diseases.
If the tonsils do not cope with their function as an immune organ, then even slight overwork, stress, or mild hypothermia can significantly reduce the immune defense and open the way for microbes and exacerbation of the disease.
Causes of enlarged tonsils
Tonsils enlarge if the body is infected with strepto-staphylococci or viral infections. This happens as a result:
- The transition from normal inflammation to chronic inflammation.
- Decreased immunity during hypothermia, a stressful situation or due to other reasons.
- Irritation or poisoning from chemicals, allergens, unusually spicy foods.
You can compare what normal and inflamed tonsils (tonsils) in the throat look like in the photo:
Complications
Chronic tonsillitis is very dangerous due to rapidly occurring complications. The most severe of them are heart disease - myocarditis, inflammation of the joints - rheumatism and serious kidney damage - glomerulonephritis.
Some toxins that are produced by microbes in the tonsils and then enter the bloodstream can damage cartilage and ligament tissue. The result is inflammation and pain in the muscles and joints. Other toxins often cause persistent fever, changes in blood tests, fatigue, depression, and severe headaches.
Chronic tonsillitis can affect the functioning of such a vital organ as the heart. The tonsils are often parasitized by group A beta-hemolytic streptococcus, the protein of which is very similar to the protein found in the connective tissue of the heart. Because of this, the immune system can show retaliatory aggression not only to the emerging streptococcus, but also to its own heart. As a result, heart rhythm disturbances, heart valve prolapses, and even the development of severe myocarditis and bacterial endocarditis occur.
For the same reason, articular surfaces and kidney tissue are at great risk. Unfortunately, the development of diseases such as rheumatoid arthritis and glomerulonephritis is extremely high.
Due to the fact that the source of infection remains in the tonsils for a long time, a distortion of the body’s reactivity occurs, resulting in allergic changes. In some cases, just one course prescribed by a doctor can get rid of itching and allergic rashes, and in some cases stop the development of bronchial asthma attacks.
Chronic tonsillitis during pregnancy
It is very important to pay attention to the disease during pregnancy. When planning a pregnancy, even in the case of a compensated condition, that is, a condition outside of an exacerbation of tonsillitis, it is highly advisable to carry out a planned course as prescribed by a doctor. This will reduce the bacterial load on the entire body in general and on the palatine tonsils in particular.
It is very encouraging that doctors are now referring pregnant women and women who are just preparing for pregnancy for treatment of tonsillitis. Unfortunately, in some cases one of the reasons for not carrying a pregnancy to term is this disease, although at first glance it is hard to believe, tonsillitis is a traffic jam, the treatment of which and other manifestations may seem in no way related to pregnancy.
Before conceiving a child, it would be correct to examine the future father of the child for the disease and, if necessary, treat it as well. This will significantly reduce the risk of developing chronic tonsillitis in the unborn child. And, on the contrary, the worse the condition of the future father and especially the mother, the risk of developing the disease in the child increases many times over.
Before pregnancy, it is very important to carry out comprehensive treatment of the symptoms of chronic tonsillitis. But even during pregnancy, it is recommended to repeat the course, preferably in the second trimester, when the woman’s condition is perhaps the most comfortable. It is important to note that physiotherapeutic procedures cannot be carried out during pregnancy, but it is highly desirable to wash the palatine tonsils using a vacuum method, followed by treatment with antiseptic solutions.
The right approach
Sore throat, tonsillitis - treatment in children and adults is important to carry out immediately for all diseases of the oral cavity and nasopharynx that bother you. If breathing through the nose is impaired, and mucus or mucopurulent discharge flows down the back wall of the pharynx, then these symptoms should be given special attention.
Chronic tonsillitis - treatment (effective) can be conservative and surgical. Due to the fact that the removal of tonsils can cause serious harm to the defenses and immunity of the human body, otolaryngologists should try their best to preserve the tonsils and restore their functions without resorting to surgery to remove the tonsils. Modern methods of treating tonsillitis provide a greater chance of recovery without intervention.
Friends! Timely and correct treatment will ensure you a speedy recovery!
Chronic purulent tonsillitis - treatment of a conservative type must always be carried out in an ENT clinic, performing a complex, pathogenetically based course of treatment, as well as using a medicinal approach - medications prescribed by an ENT doctor.
What healthy tonsils look like and where they are located
The tonsils of a healthy person are of average size; they usually do not extend beyond the arches of the pharynx. But exceptions are possible - in some people large tonsils occur due to anatomical features, not disease .
Photo: this is what healthy tonsils (tonsils) look like
The naturally uneven surface structure of the tonsils should not be pronounced and lumpy. Healthy tonsils are indicated by their color; usually it is uniform, pinkish in color, without red furrows or inclusions.
The back wall of the oral cavity, palate, and uvula with healthy tonsils are evenly colored and have no signs of inflammation. The pharyngeal mucosa should be free of swelling and have a pronounced pattern of blood vessels. There should be no purulent deposits or unhealthy plaque on the surface of the tonsils themselves.
A complex approach
First stage
Viral tonsillitis - treatment with a good and pronounced effect is obtained by washing the lacunae of the palatine tonsils. There are two ways to wash the tonsils.
A very old method is to rinse the tonsils with a syringe. Previously, this method was widely used, but today it is used for lack of a better one or when the patient’s gag reflex is very pronounced.
The disadvantages of this method are that during the process of washing the palatine tonsils, the pressure created by the syringe is not sufficient to effectively wash out caseous masses from the lacunae of the tonsils. Also, this technique is contact and traumatic, since when using a straightened attic needle, its thin and sharp end can prick the inner surface of the palatine tonsil, namely the crypts - the channels into which the needle enters. Also, the tip from the set with a syringe is used for rinsing the tonsils and injecting into the larynx. On the contrary, it is very wide in diameter and injures the tonsil tissue when inserting the tip into the lacuna, or in general, due to the large outer diameter, it cannot always get there.
Practice has shown that today, the best results are achieved by the approach when the ENT uses the Tonsilor attachment.
First, it is necessary to rinse the lacunae of the palatine tonsils with a modified attachment of the Tonsilor apparatus with a transparent antiseptic solution, for example, saline solution (also known as isotonic sodium chloride solution). This is necessary so that the doctor can clearly see what he is washing out of the palatine tonsils.
Second phase.
Since the tonsils are washed from pathological secretions, it is necessary to immediately influence the tissues of the palatine tonsils with low-frequency ultrasound. At the same time, a medicinal solution passes through the ultrasonic tip of the “Tonsilor” apparatus, which, due to the ultrasonic effect of cavitation, turns into a finely dispersed medicinal suspension, which, due to hydraulic shock, hits the tissues of the palatine tonsil and the posterior wall of the pharynx with force and impregnates the medicinal solution into the submucosal layer of the tonsil.
The procedure for exposure to ultrasound is correctly called: Ultrasonic medicinal irrigation. In our clinic we use a 0.01% solution of Miramistin. This drug is good because it does not lose its properties under the influence of ultrasound. Miramistin is a very strong antiseptic drug, and ultrasound exposure further enhances the durability of the physiotherapeutic effect.
Third stage.
It is necessary to treat (lubricate) the palatine tonsils with Lugol's solution, which is also a strong antiseptic based on iodine and glycerin.
Fourth stage.
The otorhinolaryngologist at our clinic conducts a laser therapy session on the tissue of the palatine tonsils and the mucous membrane of the posterior pharyngeal wall. Laser treatment of tonsillitis in adults is very effective. Its action is aimed at reducing swelling and inflammation of the tissues of the palatine tonsils.
The laser radiation source can be installed in the oral cavity and acted in close proximity to the palatine tonsils and the mucous membrane of the posterior pharyngeal wall, thereby achieving the best results.
You can also install the laser emitter on the skin of the anterolateral surface of the neck in the projection of the location of the palatine tonsils and the posterior wall of the pharynx.
Fifth stage.
It is recommended to conduct sessions of vibroacoustic influence. They are carried out with the aim of normalizing microcirculation in the tissues of the palatine tonsils and improving the trophism (nutritional function) of the palatine tonsils themselves.
Sixth stage.
Effectively sanitize the microflora located on the surface of the palatine tonsils using ultraviolet irradiation (UVR).
This method has long been known, has proven itself very well and is still in service in many city (especially children's) clinics.
In this case, it is necessary to approach courses. The number of procedures in each specific case is determined individually at the first consultation with an ENT specialist. But for a lasting effect to occur, at least five sessions must be performed. If, during the fifth procedure, caseous and mucous masses are still washed out of the lacunae of the palatine tonsils, rinsing and other procedures must be continued “until clean rinsing waters”. As a rule, the number of ENT procedures does not exceed 10 treatment sessions.
After a full course, the lacunae of the palatine tonsils restore their ability to cleanse themselves, and the patient feels much better and more energetic.
In order to have a lasting result, it is necessary to carry out conservative treatment 2 to 4 times a year, as well as independently once every 3 months, take homeopathic and antiseptic medications.
In this case, you will most likely be able to avoid exacerbations of this disease and the need to remove the tonsils.
If, 2-4 weeks after the end of the course, caseous detritus again begins to accumulate in the thickness of the palatine tonsils, and the patient’s ENT complaints begin to bother them, as before the start of the course, conservative treatment of chronic tonsillitis in children and adults is considered ineffective. In this case, the patient is asked to consider the option of surgical removal of the tonsils. But fortunately, such an outcome (result) is quite rare.
Functions and structure of the tonsils
Tonsils are organs of the human body’s immune system. Their main function is antibacterial protection against pathogenic microbes that penetrate the oral cavity by airborne droplets and provoke inflammatory diseases. The second, no less important task of lymphoid cells, colloquially called tonsils, is hematopoietic. They supply lymphocytes into the bloodstream and control their content in the required quantity.
There are six tonsils in total:
- A pair of palatals. As you can see in the photo below, the tonsils are the largest ones available. They are located on the sides of the pharynx in the tonsillar niches. To see where the tonsils are, you should open your mouth wide and look in the mirror. The free surface of the lymphoid formations, covered with several layers of epithelium, is turned towards the pharynx. Each formation has crypts - cracks. The other side of the palatine tonsil fuses with the lateral surface of the pharynx using a capsule.
- A pair of tubes located in the nasal cavity at the mouth of the auditory tube. Normally small organs in case of hypertrophy block the connection between the nose and middle ear, causing otitis media and hearing impairment.
- Pharyngeal. It is almost impossible to independently see the location of the tonsil, called the nasopharyngeal or pharyngeal tonsil. The organ located in the back of the nasopharynx can be detected only when it is significantly enlarged and in a position hanging over the uvula.
Enlarged adenoids—the so-called inflamed pharyngeal tonsil—are especially dangerous for children. Children cannot breathe fully, hearing loss occurs, and otitis media develops. If drug treatment does not work, the adenoids are removed.
- Lingual. Where the tonsil is located is clear from its name - it is located at the root of the tongue. A rough formation with tubercles is covered with lymphoid tissue. When inflamed, the tonsil interferes with eating and hurts when talking.
Drug treatment of chronic tonsillitis
Dear patients! In this article I will describe only general principles and approaches.
More precise treatment will be offered to you at the initial ENT consultation, where an accurate diagnosis, form and degree of the disease will be made, as well as an optimal recovery plan will be proposed and a prognosis for the duration of remission will be given.
So:
- Antibacterial approach. Antibiotic therapy is important and necessary. But the decision to prescribe antibacterial drugs is made individually and only after a visual examination.
Antibiotics can be either light, prescribed for a short course and have no effect on the mucous membrane of the gastrointestinal tract, or heavy, which must be prescribed under the guise of probiotic medications. The choice of antibiotic depends on the severity of chronic tonsillitis and the microflora that supports this condition. - Probiotic treatment is prescribed in case of taking aggressive antibiotics, as well as in the presence of concomitant gastritis, duodenitis, reflux esophagitis.
- Antiseptic approach. Antiseptic sprays, aerosols, and rinses also give a very good effect and are therefore mandatory in the fight against chronic tonsillitis. I prefer a 0.01% solution of Miramistin, a 1% solution of Dioxidine (1 ampoule diluted - 10 ml + 100 ml of boiled warm water) and Octenisept, which must be diluted with boiled warm water or saline in a dilution of 1:5 , or 1:6.
- Decongestant (desensitizing) therapy is mandatory. It is needed to relieve swelling of the palatine tonsils and the surrounding tissue, as well as the mucous membrane of the posterior pharyngeal wall. This is also necessary for better absorption of all medications used. Such modern medications as Cetrin, Claritin, Telfast can cope with these tasks. But if a certain desensitizing drug helps you for a long time, you should not change it to another.
- Immunostimulating therapy. Here I want to draw your attention to the fact that the doctor prescribes drugs that stimulate the immune system. These drugs should not be confused with immunomodulators, which are strictly prescribed by an immunologist based on the results of a blood test. There are not so many drugs that stimulate local immunity at the level of the palatine tonsils and the mucous membrane of the posterior pharyngeal wall. Of the well-known drugs, Imudon comes first. The course must be at least 10 days. You need to take (dissolve) Imudon 1 tablet 4 times a day.
- Homeopathic treatment. In addition to conventional drug therapy of a chemical nature, it is necessary to take homeopathic medications that improve the trophism and, as a result, the nutritional function of the palatine tonsils. The drugs of choice may be tonsillotren and tonsilgon, as well as rinses, steam and ultrasonic inhalations with infusions and herbs: propolis, string, sage, chamomile and some other herbs.
- Emollient therapy is used symptomatically, when, against the background of exacerbation of tonsillitis, as well as taking medications, there may be dryness, rawness and soreness in the throat. In such cases, you can use peach oil, which must be instilled a few drops into the nose, throwing back the head. You can rinse your mouth with 3% hydrogen peroxide (VERY IMPORTANT! 6% and 9% hydrogen peroxide CANNOT be used!!!). To do this, you need to pour half a bottle of peroxide (10 ml) into a cup, put it in your mouth and rinse the entire solution once, for as long as possible. Then the solution is spat out and rinsed from foam and bitterness with warm boiled water. After gargling with hydrogen peroxide, you will feel a significant softening and comfort in your throat. You can gargle twice a day, but no more.
- Analgesic therapy is used if necessary, as symptomatic therapy, depending on the severity of the pain syndrome. Of the tablet forms, it is better to give preference to Nurofen or Ketanal and its derivatives: Ketarol, Ketalar, Ketanof, Ketanal.
- Diet therapy. Nutrition also plays a significant role in recovery. It is necessary to limit the intake of spicy, fried, sour, salty and peppery foods. During treatment, you should exclude hard foods from your diet. It is also recommended to protect yourself from very hot and very cold foods. Drinking alcohol, especially strong alcohol, is also contraindicated.
Pathology
Developmental anomalies
. Developmental anomalies include the palatine lobule and the accessory palatine M. Sometimes, instead of one palatine M, two M develop on each side. Additional lobules hanging on the stem have been described. As a rule, these anomalies do not require treatment.
Damage
— burns, wounds of M. — are rare in isolation; more often they are combined with internal and external injuries of the pharynx (see).
Foreign bodies
- most often fish bones, which can penetrate into the muscle tissue, causing pain when swallowing. Remove them with tweezers or special forceps. After removal, a disinfectant rinse and a gentle diet are recommended for one to two days (see Foreign bodies, pharynx).
Diseases
Rice.
6. Schematic representation of the first stage of the tonsillotomy operation: the hyperplastic area of the left palatine tonsil is captured by the tonsillotomy ring. Acute disease of palatine M.— acute
tonsillitis
, or tonsillitis
(see). Hron, inflammation of the palatine M.—tonsillitis (see). Hyperplasia of the palatine membranes occurs in children; there are no signs of inflammation. M. are only increased in size. If hyperplasia causes difficulty breathing or swallowing, children undergo surgery - tonsillotomy (Fig. 6), i.e. partial cutting off of the protruding part of the M. Before the operation, a full wedge examination is necessary.
The operation is low-painful, most often performed without anesthesia, on an outpatient basis, with a special instrument - a guillotine-shaped knife - tonsillotome, the size of which is selected according to the size of the removed muscle. Hyperplasia of the palatine muscles is in most cases accompanied by the proliferation of adenoid tissue of the nasopharynx, therefore tonsillotomy is often combined with adenotomy (see . Adenoids). Bleeding after tonsillotomy is usually minor and stops quickly. The child should remain under medical supervision for 2-3 hours. It is recommended to observe bed rest for 1-2 days, then semi-bed rest for 3-4 days. Food should be liquid and mushy, at room temperature.
Acute inflammation of the pharyngeal M., or acute adenoiditis
(see), observed mainly in children. In this case, the tubal M. may also be involved in the inflammatory process. Inflammation is catarrhal, follicular or fibrinous in nature. Due to the anatomical proximity of the mouth of the auditory tube, symptoms of tubo-otitis may occur (see).
Isolated disease of the lingual M. is much less common. It occurs in middle-aged and elderly people and may be accompanied by an abscess of the lingual M.; occurs with high fever, difficulty swallowing and speaking, and severe pain when protruding the tongue.
With angina of the lateral ridges of the pharynx, inflammation occurs in the lymphoid follicles scattered along the back wall and in the lateral lymphoid ridges (columns). Often a whitish dotted coating appears on individual follicles of the posterior pharyngeal wall.
A disease of the lymphoid tissue of the larynx is called laryngeal angina
; it is manifested by high fever, general malaise, sharp pain when swallowing food and palpating the larynx area. Plaques are often visible, and there may be swelling of the outer ring of the larynx (see Laryngitis).
In addition to the primary lesion of the tonsils, changes in the lymphoid tissue of the pharyngeal ring occur with blood diseases. With leukemia (see), infectious mononucleosis (see Infectious mononucleosis), lymphogranulomatosis (see), an increase in palatal M. can cause difficulty breathing and swallowing. Ulcerative changes in the palatine muscles, such as necrotizing tonsillitis, are also possible.
With syphilis, the palatine M. are affected in all stages of the disease. There are descriptions of hard chancroid M.: against a limited hyperemic background in the upper part of M. a hard infiltrate appears with painless erosion in the center, the edges soon turn into an ulcer with compacted edges and bottom; the lesion is unilateral, characterized by regional lymphadenitis (see). In stage II of syphilis, syphilitic tonsillitis occurs: round or oval plaques, separate and confluent, appear on the muscle, rising above the surface of the muscle, surrounded by a reddish rim, easily ulcerating; characterized by bilateral lesions; the entire M. is enlarged, dense, covered with plaque; Papules are found on the mucous membrane in the corners of the mouth, on the palatine arches, and along the edge of the tongue. In stage III, gumma can lead to the disintegration of M., which threatens bleeding from large vessels. Treatment - see Syphilis.
Primary M. tuberculosis is rare; its main symptom is difficulty swallowing and nasal breathing as a result of concomitant M. hyperplasia. Secondary M. damage can be observed in patients with pulmonary tuberculosis. Both forms can occur hidden, simulating a banal chronic condition, tonsillitis. Treatment - see Tuberculosis.
Surgical removal of tonsils
If we talk about the removal of the tonsils, then the operation to completely remove the tonsil tissue is called a bilateral tonsillectomy.
Partial removal of the tonsils is called a bilateral tonsillotomy.
It is extremely rare that the palatine tonsil is removed routinely on one side. There is also a practice of a number of hospitals (they like to do this in the Pirogov City Clinical Hospital No. 1) of removing the palatine tonsil or tonsils in case of a paratosillar abscess. This operation is called abscessonsillectomy. But it must be remembered that against the background of severe pain caused by an abscess, removal of the tonsil is extremely painful. Due to the purulent process, it is impossible to provide adequate anesthesia. Therefore, it is necessary to anesthetize the peri-almond tissue only with strong anesthetics: Ultracaine and Ultracaine DS-forte.
Routinely, palatine tonsils can be removed under local anesthesia or general anesthesia. Previously, this operation was performed only under local anesthesia.
Fortunately, there is now modern equipment that allows removal of palatine tonsils under general anesthesia or under anesthesia using cold plasma coagulation - Coblator.
Prevention of chronic tonsillitis
- Drug therapy
. If an ENT patient undergoes treatment courses in the clinic once every 6 months, then in addition to six-month procedures, he is recommended to take the drug Tonsilotren, with a frequency of once every 3 months, i.e. 4 times a year. The course of taking (resorption) of the drug is for 2 weeks (more precisely 15 days). It is also possible to instill 0.01% Miramistin solution, 4 pumps 4 times a day for 2 weeks, in courses 4 times a year. - Climatotherapy and spa therapy
. An important point in the prevention of chronic tonsillitis is visiting seaside resorts. Sunbathing, humidified sea air, swimming and, as a result, the inevitable entry of sea water into the mouth have a beneficial effect on the prevention of chronic tonsillitis. - Work and rest schedule
. In order for the periods of remission to be long, it is necessary to fully rest and not expose yourself to stress. It is not without reason that chronic tonsillitis, like sinusitis, is classified as a social disease, in which the more stress and workload there is at work, the higher the likelihood of exacerbation of chronic tonsillitis. - Diet
. It is very important to eat right. Under no circumstances should you get carried away with fried, salty, peppery, sour, bitter, i.e. that food that irritates the mucous membrane of the back of the throat and palatine tonsils. Citrus fruits are contraindicated. The consumption of alcoholic beverages, especially strong ones, is also contraindicated. It is not advisable to eat very hot and very cold and solid foods.
Embryology
Rice.
1. Schematic representation (sagittal section) of the nasal, oral cavities and pharynx: 1 - lingual tonsil; 2 - palatine tonsil; 3 - pharyngeal (nasopharyngeal) tonsil; 4 - tubal tonsil; 5 - scattered lymphatic follicles in the mucous membrane of the posterior pharyngeal wall. Rice. 2. Schematic representation of the anatomical variants of the palatine tonsils (according to K. A. Orleans with some modifications): 1 - free tonsil protruding into the pharynx; 2 — the mouth of the accessory intrapalatal tonsil; 3 - additional intrapalatal tonsil; 4 - sine of Turtual; 5 - muscular wall of the tonsil fossa; 6 - tonsil capsule; 7 - triangular fold; 8 - tonsil, pinched in the palatine arches; 9 - upper corner of the tonsil fossa; 10 - large palatine lobule. The formation of the tonsils occurs during the prenatal period of development in the area of the head intestine. There is a certain sequence in their formation and development. First of all, the palatine, then the pharyngeal, lingual and tubal M. appears. The palatine M. are laid at the bottom of the second gill pouch at the end of the 2nd - beginning of the 3rd month in the form of a protrusion of the endoderm. The latter gives rise to the epithelial cover and crypt system of M. Lymphoid tissue of M develops from the surrounding mesenchyme. At the 8th month of intrauterine development of the fetus, lymphatic follicles of M. (folliculi lymphatici tonsillares) appear, and by the end of the 1st month of the child’s life, centers appear in them reproduction (centrum multiplicationis). Pharyngeal M. is formed in the 3rd-4th month in the form of 4-6 folds of the mucous membrane in the area of the pharyngeal vault. At the 6th month, lymph follicles appear for the first time, and at the 2nd - 3rd month after birth, reproductive centers appear. Lingual M. is formed as a paired formation in the 5th month in the form of longitudinal folds of the mucous membrane of the root of the tongue. At the 6th month, the folds fragment, at the 7th month, follicles appear, and at the 3rd - 4th month after birth, reproductive centers appear. Tubal M. are formed in the 8th month in the form of separate accumulations of lymphocytes around the pharyngeal opening of the auditory tube. By the birth of a child, follicles are formed, and in the first year of life, reproductive centers are formed.
Treatment or removal of tonsils?
Dear patients! If you have visited several specialists in this field, if a course of treatment for chronic tonsillitis has been carried out and none of the methods has brought the expected result, then only in this case should you think about removing the tonsils.
If a conservative approach gives lasting results for 4-6 months or more, then the palatine tonsils are able to fight on their own. Your task is to help the tonsils by regularly sanitizing them and stimulating their work physiotherapeutically.