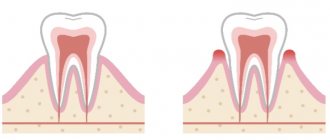
Gingivitis is an inflammation of the gum tissue. This is the initial and most common form of gum disease in general. If left untreated, gingivitis can progress to periodontitis, which is a destructive form of periodontal disease.
Gingivitis is associated with the long-term effects of plaque deposits on the teeth. Dental plaque is a sticky substance made up of bacteria, desquamated epithelium and food debris, which always accumulates in areas of the teeth that are difficult to clean naturally. This is also the main cause of caries.
Periodontitis is an inflammation and is based on infection of the pockets between the tooth and the gum, which destroys the tissues that support the teeth - the gums, ligaments and teeth (in the alveolar bone).
If plaque is not removed in a timely manner, it turns into a hard deposit that forms at the base of the tooth. Plaque and tartar irritate and cause inflammation of the gums. Actively reproducing bacteria and toxins, which are the “waste” of their vital activity, are the cause of the rapid progression of gum disease.
The following are factors that increase the risk of developing the disease:
- Poor oral hygiene
- Pregnancy – hormonal changes affect gum sensitivity
- Diabetes
- Rough and uneven teeth
- Use of certain medications (phenytoin, bismuth)
- Use of contraceptives
Many people may experience some symptoms of gingivitis at different times in their lives - they often develop during puberty or adulthood due to hormonal changes (pregnancy, menopause). Different forms of gingivitis can persist or recur frequently, depending on the health of your teeth and gums.
Forms of gingivitis
- Catarrhal
- Ulcerative-necrotic
- Hypertrophic
Symptoms
- Externally - red and swollen gums
- Bleeding. Bleeding from the gums, even while brushing your teeth, is a sign of inflammation and a leading marker of periodontal disease.
- Bad breath. Food debris and bacteria can cause a bad taste in the mouth and persistent bad breath.
- Recession of gum tissue and tooth loss. As the disease progresses, the gum tissue decreases in volume and the supporting structure of the bone weakens.
- Abscesses. In the recesses of periodontal pockets between the gum and bone, dental deposits or food particles can become blocked, which causes acute purulent inflammation, the product of which is pus.
Acute catarrhal gingivitis
Acute catarrhal gingivitis is characterized by hyperemia and swelling of the gums, bleeding, pain, burning, chronic cyanosis, swelling, and loosening of the gums. Microbial plaque and hard dental deposits are responsible for the development of the disease. False pathological pockets and gingival stone are formed.
Characterized by the following
The gingival margin appears dirty gray, easily separated from the necrotic film. Acute pain, inability to eat. Bad breath, drooling. Regional lymph nodes are enlarged and painful. Body temperature up to 38-39. Lethargy, headache. Ulcers can spread to the oral mucosa.
Often, the presence of nausea in the first trimester does not allow proper oral care. When exposed to mild irritants, slight bleeding occurs on contact. Infection and the formation of purulent discharge are possible.
Treatment includes:
- Tartar removal
- Removing dental plaque from the tooth surface
- Polishing interdental spaces
- Correction of the proper condition of fillings
Causes of gingivitis
The most common cause of gingivitis is poor personal oral hygiene. Violation of the rules may consist of inappropriate technique, irregular brushing of teeth, refusal to use dental floss and rinses after meals. As a result, food particles accumulate between the teeth, and a large amount of soft plaque forms on the surface of the teeth. This is a favorable environment for the proliferation of bacteria, which leads to the inflammatory process.
Soft plaque, which is not removed for a long time, mineralizes and hardens over time. When tartar appears, pathogenic microorganisms also actively multiply on it. In addition, the sharp edges of hard deposits injure the gum margin, which reduces local protective factors.
There are other common local causes of gingivitis:
- unsound orthopedic, orthodontic structures: braces with sharp edges,
- chips of enamel, destruction of teeth and fillings: injury to mucous membranes with sharp edges;
- teething disorders, dental caries, pulpitis, periodontitis, abscesses and other diseases;
Systemic pathologies and certain conditions can lead to the development of gum inflammation. The most common ones are:
- endocrine diseases - diabetes mellitus, Graves' disease, etc.;
- diseases of the digestive system - gastroesophageal reflux, Crohn's disease, chronic cholecystitis, etc.;
- hypovitaminosis, lack of minerals due to a strict diet or impaired absorption of nutrients;
- taking certain medications - antidepressants, local vasoconstrictors, antibiotics, combined contraceptives, beta-blockers, etc.;
- past infections and surgical interventions;
- puberty, pregnancy, menopause - changes in hormonal status not associated with illness;
- allergic reactions to food, medicines, hygiene products;
- bad habits.
Often there is a combination of factors - a combination of local and general causes of weakening of immune forces. You can find out the exact reasons only with the help of a doctor.
Ask a Question
Diagnosis of catarrhal gingivitis
Diagnosis of catarrhal gingivitis is not difficult. By collecting a history of the onset of the disease, complaints, and also by examining the patient, you can accurately understand the cause of the disease. It is necessary to examine the gums with instruments and check the teeth for mobility.
Teeth staining is often used to identify plaque, this method clearly shows the patient whether their hygiene is good or if there is room for improvement.
Plaque is painted in different shades of purple; the darkest color is painted on denser and long-accumulated plaque; it is in these areas (between the teeth and near the gums) that we most often do not clean the plaque.
They also take a photo of all the teeth (panoramic photo) to make sure that gingivitis has not progressed to periodontitis, a more severe inflammatory disease of the gums that damages the bone.
Symptoms and consequences
Symptoms of gingivitis are determined by stage. The disease can begin with the following manifestations:
- swelling, redness, looseness of the gums;
- increased sensitivity of tissues, bleeding during brushing teeth and eating due to fragility of blood vessels;
- pain when chewing and touching;
- bad breath.
As the disease progresses, the necks of the teeth may become exposed, which leads to increased sensitivity of the teeth - it becomes difficult to accept hot and cold drinks and foods. The pain also increases over time, and severe difficulty chewing food may occur. In addition to general symptoms, there are also specific ones characteristic of a particular type of gingivitis.
The consequences of gum inflammation can be very serious: the pathological process often spreads to the ligamentous apparatus of the tooth, and periodontitis occurs. This condition is dangerous due to the mobility of teeth and the high probability of their loss. A chronic focus of inflammation in the mouth is a risk factor for the development of diseases of the ENT organs.
Forms of the disease
In dentistry, there are two main forms of the disease:
- acute catarrhal gingivitis. This is a pronounced one-time inflammation of the gums, which has a temporary limitation and can develop into a more serious form;
- chronic inflammation. It develops when the acute stage is ignored and self-medication; it is a low-grade inflammation. It recurs periodically and requires repeated treatment.
In terms of prevalence, gingivitis can be localized, when 1-3 gums become inflamed, and generalized, in which the entire tissue of the dentition or both jaws is affected.
Types of gingivitis
Gingivitis can be acute or chronic. In the first case, noticeable symptoms occur. Chronic forms are characterized by mild symptoms, pain is absent or minimal. Periodic slight bleeding of the gums during brushing and halitosis may occur. It is important to understand that sluggish gingivitis is characterized by periodic exacerbations.
Inflammation of the gums is classified not only by its form, but also by the nature of its course.
Catarrhal gingivitis
Catarrhal gingivitis is characterized by redness of the gum area. Itching and bleeding due to mechanical action and mild pain may occur. This is the most common and easiest to treat type of inflammation. Quite often it acts as the initial stage of development of other forms.
Ulcerative gingivitis
Necrotizing ulcerative gingivitis is characterized by the formation of open ulcers, death of areas of gum tissue, and strong bad breath. One of the typical symptoms is the appearance of a grayish coating. The disease is more difficult to treat; in the absence of timely assistance, purulent foci and severe necrosis may appear.
Hypertrophic and atrophic gingivitis
Ulcerative-necrotic gingivitis is followed by hypertrophic gingivitis - excessive growth of tissues occurs that cover the crowns of the teeth. There is keratinization of areas of the gums.
The atrophic form of the disease, on the contrary, is characterized by a decrease in the level of the gums and exposure of the necks of the teeth. This condition is dangerous due to the loss of healthy teeth.
Desquamative gingivitis
This type of inflammation is characterized by abundant desquamation of the gum epithelium. Distinctive features are pronounced redness and noticeable peeling areas of the surface of the mucous membranes.
Hypertrophic gingivitis –
Hypertrophic gingivitis is a variant of chronic gum inflammation.
With it, there is an increase in the volume of the gums, which can occur either due to persistent chronic swelling of the gums (which practically does not respond to anti-inflammatory therapy), or due to its fibrous growth. The hypertrophic form of gingivitis most often occurs only on the front surface of the teeth. Causes of occurrence - most often occurs with endocrine disorders, toxicosis of pregnant women (gingivitis of pregnant women), with hormonal changes in adolescents (juvenile gingivitis), as well as with malocclusion and in the presence of local traumatic factors - overhanging edges of fillings and crowns. In some cases, gum hypertrophy is a consequence of long-term chronic catarrhal gingivitis.
Hypertrophic form of gingivitis: photo
Hypertrophic gingivitis - symptoms and treatment will depend on the form of this disease, i.e. depending on what exactly causes the gum enlargement (edema or fibrous growth). In accordance with this, edematous and fibrous forms of hypertrophic gingivitis are distinguished.
- Edema form (Fig. 16-17) - the gingival papillae in this form are enlarged not due to tissue proliferation, but due to their swelling.
Accordingly, they will not be dense, but loose. It is this form of gingivitis that most often develops in pregnant women and adolescents against the background of hormonal changes. At the beginning of treatment, it is necessary to remove dental plaque and anti-inflammatory therapy. If the effect of these measures is insignificant, then sclerosing therapy is used, when, against the background of pain relief, a sclerosing solution is injected into the swollen gingival papillae. Typically, solutions of 40% glucose, 25% magnesium sulfate, 10% calcium chloride are used. 0.1-0.2 ml of solution is injected into each papilla. Course – 3 or 4 injections into each gingival papilla. The intervals between series of injections are usually 1-2 days. If the effect of such therapy is absent or insufficient, prednisolone is injected into the gingival papillae.
- Fibrous form (Fig. 18, 19) - the gingival papillae in this form are dense, and not loose as in the edematous form. This is due to the fact that the increase in gum volume did not occur due to swelling, but due to the proliferation of fibrous connective tissue. Treatment begins with the elimination of traumatic factors (overhanging edges of fillings, crowns, and also in the case of a traumatic bite - selective grinding of teeth). At the same time, dental plaque is removed.
The main method of treating the fibrous form is surgical excision of gum tissue (Fig. 19-21). After excision, a course of anti-inflammatory therapy is prescribed, for example, therapeutic dressings with heparin ointment, hydrocortisone and other drugs. It should be noted that in the absence of treatment, the long-lasting edematous form of hypertrophic gingivitis can easily turn into fibrous.Surgical excision of the gum –
Diagnostic features
Gingivitis can be recognized visually—sometimes one examination by a doctor is enough. But you should make sure that there are no more serious pathologies, so diagnosis may include not only a visual assessment of the condition of the oral cavity, but also other measures:
- collecting anamnesis, assessing the condition of structures in the oral cavity;
- probing of periodontal pockets if present;
- determination of tooth mobility;
- electroodontodiagnosis to determine the condition of the dental pulp;
- panoramic x-ray or targeted x-ray - to exclude periodontitis, periostitis and other pathologies of deep structures, jaw bone tissue, etc.
It is important to take into account the presence of chronic diseases and medications. Only with complete information can a doctor make an accurate diagnosis and develop an effective treatment regimen.
Gingivitis - classification
Based on the form of the disease and the nature of its course, acute and chronic gingivitis is distinguished.
- The acute form begins with noticeable redness and bleeding of the gums. They swell and the interdental papillae enlarge.
- The chronic form is not so obvious, but the pathological process leads to the growth of gingival tissue and its “creeping” onto the tooth.
Depending on the type of inflammatory process, gingivitis occurs:
- Catarrhal
— exudative processes predominate, fluid is released from hyperemic gum tissue. There is a burning sensation in the oral cavity, there is heavy plaque on the teeth, and the papillae are swollen.
- Hypertrophic
— proliferative processes (tissue proliferation) predominate. In turn, hypertrophic gingivitis comes in two forms - edematous and fibrous. In the first form, the gums bleed and are painful, and in the second form, the gums are dense and no bleeding is observed.
- Ulcerative-necrotic
- the process goes deeper into the periodontal tissue, causing, in addition to pain and bleeding, ulceration of the gums. The general condition suffers, the lymph nodes enlarge. If left untreated, this type of gingivitis can develop into Vincent gingivitis, which affects the entire mouth.
Dentists also distinguish mixed varieties of the disease.
Principles of treatment
Treatment of gingivitis begins with hygiene: professional teeth cleaning. It is important to remove soft and hard dental plaque. For this, hand tools, an ultrasonic scaler, and the powder blasting method can be used. Subgingival dental plaque can be removed using the Vector device.
It is important to eliminate foci of infection - to fill teeth affected by caries, to undergo endodontic treatment in the presence of pulpitis, to remove the roots of teeth that cannot be restored and are not involved in the prosthetic process.
It is necessary not only to pay attention to the causes of the disease, but also to reduce the influence of harmful factors:
- stop smoking;
- consume food and drinks only at a comfortable temperature;
- remove spicy and smoked foods, marinades, especially those with vinegar, from the diet;
- During the treatment period, try to eat less solid food so as not to injure the loose gum tissue.
If the source of injury to the mucous membrane is the sharp edges of teeth or dentures, the doctor will immediately take measures to prevent further damage or recommend contacting a dentist of another profile - an orthopedist, an orthodontist.
Treatment of catarrhal gingivitis
The most important thing in treatment is to understand why the disease began and how to avoid its reoccurrence.
To remove plaque and tartar, professional hygienic cleaning is carried out.
The doctor also teaches you how to brush your teeth correctly and selects suitable hygiene products for home use.
After professional teeth cleaning, rinsing with antiseptic solutions is prescribed for 7-10 days to neutralize the action of microorganisms.
Usually, removing dental plaque gives an effective result in the fight against catarrhal gingivitis. If inflammatory processes continue to develop after cleaning your teeth, then you should pay attention to other possible causes of catarrhal gingivitis and their elimination.
If catarrhal gingivitis develops against the background of general diseases, then appropriate measures are taken to treat them (for example, therapy for diabetes mellitus). In the treatment of chronic catarrhal gingivitis, gum massage, ascorbic acid electrophoresis and other measures can be performed.
Treatment is often accompanied by the prescription of a special diet that excludes irritating foods and includes foods rich in vitamins B, A, E, C. It is also necessary to reduce the amount of simple carbohydrates, especially sweets.
Drugs for the treatment of gingivitis
Treatment for gingivitis may involve the use of medications in different forms. Mouth rinses based on antiseptics allow you to solve two problems at once: mechanically remove food debris and bacterial plaque, and also deliver active ingredients to inflamed tissues. Dentists recommend using ready-made pharmaceutical products; in each specific case, a specialist will prescribe a medicinal solution to quickly alleviate the condition. Ready-made formulations are more convenient to use, and the concentration of active components in them is known, this distinguishes them from traditional methods.
The most popular are rinses based on the following antiseptics:
- chlorhexidine;
- furacillin;
- chlorophyllipt;
- Metronidazole.
Calendula, chamomile, yarrow, oak bark, and St. John's wort have antiseptic properties. Doctors do not recommend preparing alcohol infusions; it is better to choose decoctions. The recipes call for using one teaspoon of dry raw materials per glass of boiling water. It is important to cool the broth to a comfortable temperature. Take into account possible allergic reactions, give preference to those herbs to which there was no previous intolerance. It is necessary to discuss with your doctor the possibility of using traditional methods.
Effective drugs for the treatment of gingivitis are ointments and gels. Multicomponent local products for applications not only help relieve inflammation, but also have an analgesic, decongestant, and antipruritic effect. The active components of such drugs can be lidocaine, antibacterial, antifungal substances, and antiseptics. The doctor will select a gel or ointment taking into account the shape and type of gingivitis. Thus, for ulcerative inflammation, it may be advisable to use regenerating agents, and acute catarrhal gingivitis will require the use of a powerful anesthetic gel.
For hypertrophic gingivitis, surgery may be required - a simple gingivectomy. This operation involves excision of excess tissue and application of a bandage, and is performed under local anesthesia.
Treatment of catarrhal gingivitis with folk remedies
Such treatment is effective only after performing the appropriate clinical procedures and all doctor’s prescriptions. However, folk remedies are useful for preventing possible relapses during long-term fixative treatment.
- Infusion of chamomile and sage.
- A decoction of dried bird cherry or blueberry.
- A decoction of sage leaves in an infusion of oak bark.
Preventive measures
Prevention of gum disease consists of maintaining oral hygiene at home, as well as regular professional cleanings. You need to visit the dentist twice a year, promptly treat dental diseases, replace old fillings and dentures.
One way to prevent gingivitis is to eat a balanced diet. It is important to eat right, choose foods and drinks that are warm or at room temperature. Do not ignore the importance of using dental floss and mouth rinses after every meal.
Dentists at STOMA clinics know how to treat gingivitis: the accumulated experience, advanced diagnostic and therapeutic methods in the arsenal of our specialists allow us to provide urgent dental care to patients and develop effective treatment regimens.
Diagnosis of necrotizing ulcerative gingivitis
Diagnosis is made through the clinical manifestations of necrotizing ulcerative gingivitis.7,8
During the examination and questioning, the dentist identifies poor hygiene, bleeding gums, poor general condition and the absence of gum pockets (impaired attachment of the gum to the tooth). Be sure to take a panoramic photograph of all teeth to distinguish ulcerative gingivitis from periodontitis.
Additionally, bacteriological examination and the ELISA method can be carried out to confirm the diagnosis, determine the level of immunoglobulins and select appropriate treatment tactics.
It is important to distinguish ulcerative gingivitis from immunodeficiency conditions and blood diseases. For this purpose, if necessary, other tests may be prescribed.
Treatment of necrotizing ulcerative gingivitis with Tantum® Verde
Effective treatment of ulcerative gingivitis is possible with the use of anti-inflammatory drugs, which include Tantum® Verde . Benzidamine in its composition has a complex effect on the gums: reduces swelling, relieves inflammation, reduces pain and kills microbes on the surface and inside the affected tissues. Benzidamine penetrates well into the mucous membranes, which allows you to quickly cope with the disease. Tantum®Verde allows you to quickly relieve pain9, which is especially important in the treatment of necrotizing ulcerative gingivitis. From the first minute, Tantum® Verde has an anti-inflammatory and local anesthetic effect on the symptoms of gingivitis, such as a burning sensation, swelling and swelling of the gums. After the acute effects have subsided, it is possible to dissolve Tantum® Verde , since they have an anti-inflammatory effect within 9 minutes, which will allow you to quickly cure gingivitis.10, 11, 12
Differential diagnosis of gingivitis
It is based on the complaints presented to the patient, a visual examination of the patient, the results of functional tests and laboratory tests. The goal of differential diagnosis is to distinguish gingivitis from other periodontal diseases, such as periodontitis and periodontal disease.
The main feature that distinguishes gingivitis from other periodontal diseases is that the inflammatory process affects only the gum tissue, the remaining structures (muscle ligaments that hold the tooth in the jaw and bone tissue) remain unchanged.
Along with this symptom, gingivitis is not characterized by periodontal pockets, exposure of the necks of teeth, or their mobility. And the x-ray shows no signs of bone resorption.
Identifying gingivitis in a timely manner, determining its form and prescribing the correct treatment is the task of a periodontist. But not to forget about prevention and regularly visit the dental clinic is the maximum program for the patient. This is the only way to avoid a more serious periodontal disease – periodontitis.