Tooth extraction in dentistry is divided into simple and complex. When extracting a tooth with one root, such manipulation is considered simple. If the tooth has a complex root with several branches, then the procedure for removing it will be complex and is carried out using special tools and techniques.
In what cases is dental surgery difficult?
Complex manipulations regarding tooth extraction include the following situations:
- with disconnected roots that are excessively curved inward or directed in different directions;
- when the problem tooth is located in the affected bone;
- in the complete absence of a crown, when there is nothing to grab onto with forceps;
- if a filling was previously installed in the tooth, which can crack under the mechanical influence of forceps;
- when the tooth is impacted or dystopic;
- removing the "eight"
These are the main clinical features in which it is impossible to get rid of a diseased tooth using a standard simple procedure. Moreover, in each specific case the reasons for complex extraction may be individual.
Cases when complex surgery is necessary
It often happens that the only possible way to get rid of a defect formed by a complex tooth is to remove it.
Indications for this type of procedure are as follows:
- the formation of periodontal tumors and edema, accompanied by soreness of the mucous membranes and gums;
- numbness of the face resulting from damage to the nerve endings of a diseased tooth;
- with an increased risk of curvature of adjacent teeth;
- in the presence of diseases caused by improper positioning of the tooth.
Surgeries to remove problematic teeth are contraindicated for those who suffer from pathologies of the cardiovascular system, with poor blood clotting, patients who have undergone a hypertensive crisis, in the presence of infectious or viral processes in the body, as well as other individual contraindications.
Preparing for dental surgery
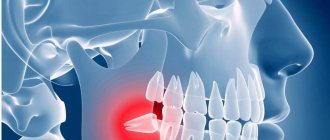
If a patient is faced with the removal of a complex tooth, then an experienced doctor will not perform such manipulations without prior preparation. An x-ray is required before the operation. This is necessary to clarify the location of the tooth in the bone, as well as to evaluate the tissues surrounding it.
When a patient has an inflammatory process, it is first cured by taking antibiotics.
Complications after pulling out problem teeth rarely occur, but to avoid them, the procedure should be trusted to a highly qualified doctor.
Types of Impacted Teeth
The position of an unerupted tooth inside the gum varies, and depending on how it is located there, the doctor decides whether to remove the tooth or relieve inflammation and allow the tooth to erupt.
Degree of retention:
- Complete (the tooth is completely hidden by the gum and bone, it cannot be seen or felt. Most often this refers to impacted wisdom teeth);
- Partial (a small part of the crown is visible, the rest is hidden);
- Retention in hard tissues (bones);
- Retention in soft tissues (gums).
Inclination of impacted tooth and crown:
- Mesial (the tooth is slightly tilted forward - this is the type of retention that most often occurs);
- Vertical (the tooth grows correctly, but cannot erupt due to lack of space);
- Horizontal (the tooth lies completely inside the gum or bone with the tip facing the other teeth);
- Distal (tooth tilted back).
In addition, although quite rare, retention occurs not of one tooth, but of several adjacent teeth of the same type (for example, two molars). This problem most often occurs in children.
How to remove complex teeth: basic techniques
In dentistry, various methods are used to eliminate a complicated tooth, the essence of which depends on the instruments chosen for manipulation:
- removal using forceps. Compared to
in other ways, this is considered the most gentle. This technique is used in cases where the integrity of the crown is preserved. The surgeon grabs the crown with forceps and loosens it in a circular motion until the tooth root ruptures from the alveolus, after which he pulls it out; - elevator extraction. If it is located outside the dentition, it is impossible to pull it out with ordinary forceps, then this technique is used. The instrument is inserted into the periodontal fissure and rotated, as a result of which the ligaments are torn. The tooth is not pulled out of the hole, but squeezed out;
- removal with a drill. This method is used to pull out teeth with multiple roots. First, the roots are separated using a drill and then each piece is removed separately. If a resorcinol-formalin filling is installed on a tooth, then a drill is also used to pull it out.
Which method is the best? Each has certain characteristics and is selected based on the condition of the tooth, the number and depth of its roots.
Removing 4 eights in one session
Removing all the sages at once can be a very reasonable and rational decision for certain indications. Most often, one-stage extraction is carried out for orthodontic indications, when it is necessary to install braces or corrective aligners.
The main advantage of such surgical treatment is the uniform and symmetrical movement of dental units due to the voids formed in the jaw in place of the sockets. After about 2 months, the sockets are overgrown with new bone, and the teeth can no longer move as easily and quickly. Thus, the duration of treatment by an orthodontist is reduced.
If removal is carried out for other indications, then this also has its advantages:
- When teeth are crowded, they move apart, thereby aligning the dentition. Otherwise, the doctor may recommend wearing special aligners to contain the process, in order to avoid the formation of large interdental gaps in the row;
- manipulations are performed by two dental surgeons in an average of 1 hour;
- anesthesia or sedation is carried out once, and not several times, if you part with the eights in turn;
- It is enough to take antibiotics only once instead of four times, which is especially important for chronic diseases;
- discomfort, pain and inconvenience when eating also will not have to be experienced twice.
Dystropic tooth: indications for removal
A tooth with an incorrect location in the dentition relative to its neighbors is called dystrophic. It can take the place of another, spontaneously turn, change the angle of growth, which significantly interferes with neighboring teeth and leads to the formation of a malocclusion.
Indications for extraction of a dystrophic tooth are:
- swelling of the gums and pain;
- numbness of the face due to damage to nerve endings;
- pronounced curvature of adjacent teeth;
- periodontitis or chronic pulpitis;
- when, due to a problem tooth, it is impossible to perform prosthetics;
- if a dystrophic tooth is the cause of periostitis or osteomelitis.
The removal process itself is similar to the procedure for removing an impacted tooth.
Wisdom teeth. Execution cannot be pardoned...
How to place commas correctly in the title? What do you need to know and what to guide you when deciding whether to preserve or remove these teeth that are problematic from a dental point of view? Let's try to figure it out.
“Wisdom teeth” or “eight teeth” usually appear in a person closer to 20 years of age, plus or minus a few years (much more often plus than minus)... Not everyone really becomes wiser by this age, but people began to call them that, hinting specifically at their late appearance. At the same time, despite the name, 8s don’t make us smarter, but we’ll get tired of listing the hassle. Why is this happening?
This is how it is in nature: everything that it does not need gradually disappears. Man has long been getting his food not in the forest, but in the supermarket, eating not raw tough meat and plant roots, but a refined Big Mac... Therefore, we no longer have a great need for so many chewing teeth and such large massive jaws as our ancestors had. And that’s why we are evolving in the direction of reducing jaws and the number of teeth. Even now there are quite a few “advanced” individuals in evolutionary terms who generally lack the rudiments of the 8th teeth (and not only them, but sometimes also incisors and canines, which is less pleasant). Although, at the moment, this is rather an exception to the general rule. But the lack of space in the jaws for all 32 teeth, on the contrary, is rather the rule. And since wisdom teeth are the very last to appear, they usually lack this very place in the dentition. That's why we have so many problems with them. This is just one of the factors, but perhaps one of the main ones.
Now let’s look at exactly what problems “wise teeth” can cause us.
Complete tooth retention.
Retention is a condition in which a tooth, for various reasons, could not erupt at the right time and in the right place. Well, with complete retention, accordingly, the tooth does not show out at all and remains lying inside the jaw.
Red arrows show wisdom teeth, which lie completely in the thickness of the lower jaw. This is complete retention. Also, this patient naturally received a “bonus” of a completely impacted central upper incisor (shown by the blue arrow).
This arrangement could be considered quite good. Because the tooth lies inside the jaw, doesn’t touch anyone, doesn’t bother anyone... it would seem, and God is with it. In general, this is how it is. It’s probably not worth running as fast as you can to pick it out of your jaw. In this form, it can lie there all its life and not cause any trouble. Or maybe not entirely so. A so-called tooth may appear around such a tooth. follicular cyst. Therefore, it is best to observe such unerupted teeth by doing an orthopantomogram at least once a year*. Well... or remove such a tooth, forever forgetting about it and the need to monitor it. After all, there are many other things in life that you have to constantly think about and remember.
Partial retention.
By analogy, here we are talking about those cases when the wisdom tooth was still able to partially erupt, but not completely. What most often bothers him? Either a powerful bony protrusion of the jaw, or an incorrect position of the rudiment, or a neighboring 7... in general, there can be many reasons, the essence remains the same - part of the unerupted tooth remains inside, and part sticks out outside. This is the most common situation and it is this that most often leads to various really tangible problems. Which one exactly?
— pericoronitis is perhaps the most common complication of a partially erupted wisdom tooth. This is inflammation in the tissues surrounding this most problematic tooth - in the gums and bone. It manifests itself as pain, swelling and redness of the gums, difficulty swallowing, and fever.
In the farthest nook of the lower jaw you can see a partially erupted number 8 and the inflamed gum above it.
Often, patients try to self-medicate in such situations - they rinse the tooth with various drugs that are at hand (from chamomile decoction to five-star cognac), swallow painkillers uncontrollably, or, worse, antibiotics. Indeed, such measures (especially antibiotics) may subside the inflammation. But an unresolved cause will sooner or later lead to a relapse. Moreover, any inflammation in the area of wisdom teeth can easily develop into an abscess or phlegmon of the face and neck, and these are serious, life-threatening surgical problems. And they are treated, among other things, by making external incisions on the face and neck. And this is really serious. I won’t insert unappetizing pictures here; a query in any search engine will help create additional motivation for any unbelieving Thomas.
I hope I have scared you enough so that you don’t feel the urge to self-medicate in such cases. You definitely need to visit a dental surgeon. If he sees no problems in the further teething of the figure eight, he will simply remove the gum hanging over the tooth (“hood”) and prescribe the necessary medications. If the tooth objectively can no longer erupt normally, then it will need to be removed. This is the only way to eliminate the cause and protect yourself from relapses of inflammation, as well as from serious purulent complications of an initially trivial problem.
— caries of the root of the adjacent 7th tooth. Often, when the 8 is “stuck” and has no chance of cutting through further, but does not bother, patients do not even think about contacting a doctor, because "does not hurt". In fact, such a semi-erupted tooth makes it difficult to maintain normal hygiene in this area and this leads to caries damage to the neighboring tooth. Moreover, the most unpleasant thing about this option is that caries develops near the very base of the tooth, develops unnoticed, and the cavity can remain invisible for a long time. As a result, a huge “hole” grows, going deep under the gum, and it is not always possible to restore such a defect qualitatively. As a finale - the loss of a good neighbor due to the “wise tooth” not being removed in time. Moreover, it will be possible to make up for the lost 7 only with an implant (which is not cheap) or a removable prosthesis (which is inconvenient to use and significantly reduces the quality of life)
On the x-ray, the arrow shows a carious cavity that arose on the 7th tooth due to its careless, wise neighbor. On the right is about the same thing, only in a live photo. The stuck figure eight is shown in green, and the caries that arose on the number 7 as a result of it is shown in blue.
- resorption (simply resorption) of the root of the adjacent 7th tooth. In general, the situation is similar to the previous one, with the same consequences. The only difference is that, having rested against its neighbor, the “wise tooth” can turn out to be very persistent and, with its pressure on the 7th tooth, cause the resorption of its hard tissues.
On the x-ray we see a wisdom tooth resting on the upper 7th. In the photo on the right is the same seven, after removal. This is the kind of root resorption that a stubborn wisdom tooth can cause due to its pressure.
- loss of bone from the adjacent 7th tooth... this is the third variation on the theme that behind a problematic, but seemingly not bothersome wisdom tooth, an innocent, good and necessary neighbor can easily suffer. An incompletely erupted wisdom tooth, resting against the 7-point, can create a space in which food debris will accumulate. This will cause periodontal pocket formation and bone loss between the 8th and 7th. But the result is still the same - removal of both teeth, bone grafting and implantation of the 7-piece.
Here the wisdom teeth decided to create problems for their owner as a couple. The lower one collapsed and rested on the 7th, causing bone loss. The top one, deprived of his partner, crawled down to meet him. What happens from this - read on.
- chronic injury to the mucous membrane. Often crookedly erupted wisdom teeth (especially the upper ones) when chewing cause chronic injury to the mucous membrane of the cheek and gums on the opposite jaw. This is unpleasant both in itself and in terms of prognosis - any chronic injury to the same place can lead to malignancy.
An upper wisdom tooth that grows unevenly towards the cheek (the gray arrow points to its tubercle) causes chronic injury to the mucous membrane (yellow arrow)
- blocking normal movements of the lower jaw with the possible development of problems of the temporomandibular joint. This is a rarer problem, but it still occurs. Each tooth in the dentition has its own pair on the opposite jaw - an antagonist tooth. And 8s are no exception. When wisdom tooth is removed or does not erupt , the other, opposite one, moves out. As a result, it can block the movements of the lower jaw and cause it to shift into an unphysiological position when chewing. This can be completely asymptomatic until symptoms begin in the joint - clicking, crunching, pain... etc.
Here the top eight lost their antagonist “thanks” to natural forces...
...and here thanks to the strength of the dentist. True, when removing one eight, you should immediately think about removing the antagonist. Well... or immediately put an implant and a crown in place of the removed wisdom tooth... if life seems too simple and bland to you.
Well, now a few words about what could happen to wisdom teeth , which still managed to erupt in their place and quite evenly. Can they really cause inconvenience in such a situation? It turns out they can.
Erupted wisdom teeth.
The main problem with properly grown 8s, despite everything, is their inaccessibility... both for hygienic measures and for quality treatment. Laziness, haste, and an increased gag reflex are the most common reasons why the hygiene of wisdom teeth is, as a rule, insufficient to prevent the occurrence of caries on them. For the same reason, quality treatment is difficult. Poor visibility, difficulties with applying a rubber dam, frequent “exclusive” structure of the canals, making them difficult to pass even for well-trained and equipped endodontists, difficulty opening the patient’s mouth (and even with normal opening, getting close to the figure eight with an instrument is not so easy), the same increased gag reflex in the patient... All these objective difficulties often force one to make a decision to remove the apparently good 8-ok. Because it’s better to remove it well once and forget about the problem, than to redo the same tooth many times, and then... remove it anyway.
There are doctors who unreasonably expand the indications for the treatment of 8th teeth, i.e. seemingly showing genuine care for the patient’s teeth, but in reality... But in reality, what happens first is the treatment of small caries, after a short time - relapse of caries, then pulpitis, then periodontitis... and, finally, natural removal after a few years. It seems that nothing has changed, except that the doctor manages to remove several “harvests” from the same problem before actually solving it. This does not always happen maliciously; some actually believe that they are prolonging the life of 8s for the benefit of the patient. Moreover, patients themselves often ask for this. At the same time, I often heard from opponents of the removal of the 8th teeth that “there is always time to remove”, “what’s mine is mine and I won’t give it up for anything”, “then, if something happens to the 7th, it will be possible to install a bridge with a support at 8." I think all the previous examples speak quite eloquently about the fact that it is not always possible to “delete” on time. If it’s such a pity to part with your teeth in favor of the dentist, then you can take them away and make a stylish decoration for a long memory... both your health will benefit, and your wisdom will always remain with you.
As for 8s as a support for bridges, the time has already passed when it was possible to talk about this seriously. Today, implantation solves the problem of the absence of any tooth without the need to “sharpen” neighboring ones. In addition, wisdom teeth, in principle, should not bear the load of their more functionally loaded colleagues (6s and 7s), because They are not at all suited for this work. Try to force a podium model, who has been on diets all her life, not just to lift a barbell, but to set a new world record in women's weightlifting... I'm afraid she will simply be crushed by sports equipment that trained female athletes can easily lift. For to each his own... It’s the same with teeth. The 6th and 7th teeth have 3 or even 4 multidirectional powerful roots, which nature designed to withstand heavy chewing loads. And in the eighth teeth, the roots almost always grow together into a single monolith, which has a cone shape and is not at all so stable - God forbid it could hold itself in the jaw. And if some irresponsible orthopedic dentists try to put an additional load on such a root, then this 8 comes to an end quite quickly, just like the “weightlifter” model... Another trouble that orthodontists often have to deal with... 8s they can grow... and grow seemingly correctly and well, but at the cost of the fact that the remaining teeth will be completely shamelessly moved, and the doctor will state that your teeth are crowded .
And since this process is not momentary, it is usually noticed too late. The price of such inattention is the removal of 8s and wearing braces.
So, to summarize, in the vast majority of cases, eights are a real headache for both patients and dentists. Modern man (if he does not live in the forest the life of our distant ancestors) really needs them insofar as. Those. If your wisdom teeth have grown evenly and in their place, you are able to care for and cherish them along with everyone else, then, thank God! Let them chew. Although I can admit from my own experience, such lucky people are an overwhelming minority. If signs of one of the above-mentioned problems appear, then there is no need to hesitate, be afraid and regret losing a part of yourself... Wisdom teeth are far from the most valuable thing about us. And without them, life does not get worse, but rather the opposite. This “on the contrary” is what I wish for you!.. With or without wisdom teeth.
Extraction for acute and chronic inflammation
Quite often, the removal of a problematic tooth is accompanied by the presence of purulent foci, gum inflammation or periodontitis. In such cases, the doctor prescribes intensive therapy with the use of antibacterial drugs, and only after the inflammatory process has been suppressed is surgery to remove the tooth performed.
There are also situations when a tooth needs to be removed urgently. Only an experienced, highly qualified doctor can perform surgery in such cases.
Consequences
After tooth extraction, some complications may appear, the cause of which may be the patient’s failure to comply with medical instructions, or a violation of the procedure technique. Frequent complaints from patients include pain in the socket area, which is present for the first time 3 days after the procedure. The second common consequence is infection of the socket, into which a secondary infection can penetrate and provoke the development of alveolitis. If a secondary infection is suspected, the doctor will prescribe antibiotics, anti-inflammatory drugs, and the hole may need to be cleaned.
Other consequences include:
- Injuries during surgery.
- Hole bleeding.
- Parasthesia.
If there are suspicions of complications after tooth extraction, any self-medication should be excluded and you should consult a doctor as soon as possible.
Complex tooth extraction: when is it necessary?
Clinical indications for which the dentist prescribes complex tooth extraction are as follows:
- the presence of an unerupted wisdom tooth in the jaw;
- if the figure eight is incorrectly positioned;
- when removing molars with two or three roots;
- with a severely damaged or twisted root;
- in case of fusion of the tooth root with the jaw bone tissue;
- in the presence of a fistula or cyst;
- with excessive fragility of the crown due to treatment with resorcinol-formalin composition.
The operation itself consists of several stages and is carried out under the influence of powerful anesthetics.
Symptoms of retention
Sometimes tooth impaction is asymptomatic, without causing pain or discomfort, but most often patients with impacted wisdom teeth notice the following symptoms:
- Unpleasant sensations when chewing food;
- Bad breath;
- Swelling of the gums and redness around the impacted tooth;
- pain or tenderness in the gums or jawbone;
- Frequent headaches or jaw pain;
- Difficulty opening the mouth;
- Temperature increase.
If such symptoms appear during the eruption of figure eights, a visit to the doctor is required. This does not mean that the tooth will have to be removed. First, the doctor will examine the oral cavity, take a photo, and only then will a decision be made on the correct treatment.
Stages of complex tooth extraction
Complex removal surgery is carried out only after x-ray diagnostics, during which the shape, length and depth of the roots are determined. If the patient has inflammation, he is prescribed treatment with antibacterial drugs.
Technique of the procedure
Wisdom tooth removal is carried out in the following order:
- the gum is separated from the neck of the tooth by making an incision in the soft tissue;
- if necessary, the interroot septum is sawed or sections of bone tissue are cut out at the location of the tooth;
- then, using forceps, the tooth is rocked and pulled out of the socket;
- Sutures are placed on the gum.
Painkillers are not required after the procedure, since the effect of the anesthetics is still present.
Causes of retention and dystopia of teeth
- Hereditary factor;
- Too early loss of baby teeth. If, after the loss of a baby tooth, the molar does not immediately grow in this place, the position of the teeth that have not yet erupted in the jaw may shift, resulting in dystopia. The later a molar erupts, the greater the risk of it becoming dystopic;
- Malocclusions, crowded dentition.
Among baby teeth, dystopic ones are rare, but this problem can arise due to too dense gums, through which it is difficult for weak teeth to break through, as a result of which they grow incorrectly. In its normal state, a child’s gums, before the eruption of baby and molar teeth, become more elastic and easily part, making room for new teeth.
In addition, in the case of childhood retention, it is often not the wisdom teeth that fail to erupt (as in most adults), but the canines and small molars, which grow later than all the others. This is not only a rather painful process, but also potential problems with the correct bite of the teeth.
On a note!
The evolutionary version explains tooth retention by the fact that after a long period of time, our jaw has significantly decreased and lost capacity, which now creates an obstacle to the eruption of wisdom teeth and, as a result, leads to dental dystopia.
The healing process of the hole after a complex removal
Basically, tissue healing occurs after 7-10 days. It should be noted that this period is quite difficult for the patient. As soon as the effect of the anesthetics stops, aching pain immediately occurs. To eliminate it, you should take pain medication.
The swelling and redness that appears will decrease every day. If there is slight itching in the socket area, this indicates intensive tissue restoration. Removal of sutures after healing is not required since they “dissolve” on their own.
During the regeneration period after removal, it is very important not to disrupt the integrity of the blood clot formed in the socket. To do this, you need to follow a few simple rules:
- during the first 2-3 hours after surgery, do not consume any drinks, much less food;
- Under no circumstances should the well be heated, cleaned or washed;
- do not rinse your mouth for 24 hours after removal;
- When eating food, you need to chew it on the opposite side in relation to the hole.
If you follow these recommendations, the tissue will soon recover without complications.
What to do if the bleeding does not stop
Immediately after removing a molar, the surgeon places a tampon on the socket to stop capillary bleeding. The patient needs to clench his jaw and not remove the tampon for 20 minutes. During this time, the blood coagulates and a clot forms in the hole, protecting the fresh wound from the penetration of bacteria into it.
If the patient has high blood pressure or poor blood clotting, the tampon should be kept in place for 40-60 minutes.
When a person strictly adheres to medical recommendations, but the bleeding does not stop, he should contact a dentist for help.