Trismus is a spasmodic compression of the mandibular muscle group (masticatory, temporal, pterygoid). The jaw loses mobility, freezes in one position, and the person is unable to do anything about it. The situation is accompanied by clenching of teeth, swelling and tightening of muscles, and increased pain on palpation.
This condition belongs to the pathologies of facial myalgia. The spasm can be either unilateral or bilateral (bilateral). In the first case, facial asymmetry is observed, the face skews to one side. In the second case, the person loses the ability to eat and talk. Trismus of the lower jaw has a negative effect on the functions of the gastrointestinal tract and brings significant psycho-emotional discomfort.
Causes of jaw clenching during trismus
- inflammation of the masticatory muscles;
- inflammation of the gums;
- caries;
- abscess;
- inflammation of the periosteum of the lower jaw;
- jaw injuries (cracks, fractures, dislocations);
- dousing with cold water;
- animal or insect bites.
Trismus can also be a consequence of the following diseases:
- osteomyelitis of the jaw;
- periostitis;
- neurosis;
- epilepsy;
- meningitis;
- hysteria;
- arthrosis of the jaw joint;
- cancerous tumors;
- convulsions;
- rabies;
- tetany;
- paralysis;
- tetanus;
- pulpitis in the acute stage, etc.
Drug treatment for muscle spasms
There is no universal remedy for muscle spasms of the head and neck. If the pain is episodic, taking painkillers in combination with supplementation with vitamins and minerals may be enough. If we are talking about chronic involuntary muscle contractions, the patient may be prescribed antiepileptic drugs, muscle relaxants, antidepressants, and antipsychotics. The doctor may also recommend medications to strengthen blood vessels and normalize blood circulation.
All patients with muscle pain are advised to ensure sufficient physical activity, avoid alcohol consumption, reduce stress levels, eat nutritiously and get enough sleep.
The main stages of trismus
- third - a person can open his mouth 10 mm, the most difficult stage;
- second - the patient can open his mouth 10-20 mm;
- first - the patient opens his mouth 30-40 mm, respectively.
In all cases, a person should immediately consult a doctor. You may need treatment in a hospital setting. In the process of clenching the jaw, there is a high probability of damage to the gums and chipped teeth. If help is not provided in time, oxygen starvation may occur.
Dental diagnosis of trismus involves:
- visual examination of the patient;
- to unclench the jaw, the dentist injects a drug that relaxes the muscles;
- To make the diagnosis more comfortable for the doctor and patient, an anesthetic drug is also administered;
- In addition to the dentist, you may need to consult a neurologist, surgeon, or traumatologist.
Signs of involuntary muscle contraction are:
- with bruxism – grinding of teeth during sleep, a feeling of overexertion in the jaws after waking up;
- with spasms of the head muscles - hoop-shaped pain in the temples, in the forehead, in the back of the head;
- pressing, pulsating, squeezing nature of pain;
- feeling of heaviness in the area of spasm;
- pain when pressing trigger points (try to palpate the area of the head when it hurts: when you press certain points, the pain increases significantly);
- nausea, vomiting, dizziness;
- painful reaction to light, loud sounds (infrequently).
When to see a doctor:
- headaches appeared suddenly and do not go away;
- you are experiencing muscle pain for the first time after 50 years;
- pain is accompanied by dizziness, weakness, numbness of the limbs;
- pain lasts more than two weeks in a row;
- painkillers either do not work at all or give an insignificant short-term effect;
- the pain is localized on one side of the head/neck.
Muscle spasms that provoke pain indicate a disruption in the healthy functioning of the body. To prevent the development of the disease, it is important to consult a doctor in time. We advise you to visit a therapist, neurologist, endocrinologist, who will prescribe detailed laboratory diagnostics for you. Based on the research results, specialists of another profile may be involved in your treatment: an orthopedist, a cardiologist, a chiropractor. Complex treatment may include taking medications, a massage course, and therapeutic exercises. A good doctor will definitely give you recommendations on nutrition and daily routine.
MIGUNOVA ANASTASIA ANDREEVNA
Cosmetologist
Initial consultation: 4500 rub.
VYATKINA IRINA SERGEEVNA
Gynecologist-endocrinologist
Initial consultation: RUB 8,500
KALININA EKATERINA ALEXANDROVNA
Cosmetologist
Initial consultation: 4500 rub.
KOZLOVA EKATERINA NIKOLAEVNA
Gynecologist, oncologist
Initial consultation: 5000 rub.
KUSRAEVA DIANA TEYMURAZOVNA
Cosmetologist, dermatovenerologist
Initial consultation: 4500 rub.
How to properly treat trismus of the masticatory muscle?
Treatment of the problem involves:
- immobilization of the jaw by applying a bandage or splint;
- eliminating the underlying cause of trismus (disease or specific condition);
- taking neuropsychic stimulants and sedatives;
- a course of taking muscle relaxants;
- a course of antibiotics (for inflammatory processes);
- physiotherapy;
- peace and release from physical work.
If the patient’s condition is severe, observation in a hospital is necessary under the supervision of a maxillofacial surgeon, neurologist, traumatologist, etc.
After eliminating acute symptoms, a person is recommended a special diet:
- plenty of fluid;
- chopped food;
- vegetables and fruits;
- natural juices.
If it is impossible to eat normally, food is supplied through a tube, and liquid is supplied through the skin.
To restore the functions of the masticatory muscle, the patient is recommended to perform special therapeutic and preventive exercises.
It is important to completely cure trismus, and not just suppress its symptoms. If the cause is not removed, the problem will reoccur. Spasms put a powerful strain on the teeth, gums, and nervous system. It is very important to contact an experienced dentist with a surgical profile, who will help cure the disease and tell you what to do in emergency situations. The 32 Dent network of clinics in Moscow employs specialists who will provide such comprehensive assistance for trismus of the masticatory muscle and other serious problems.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment
Myositis ossificans (OM) is characterized by limited bone formation within the muscle. OM is a tumor-like process localized in soft tissues [1]. The disease was first described in 1648 and is rare in children, except in those with an inherited condition known as progressive OM (fibrodysplasia ossificans progressiva, Münchmeyer's disease). The prevalence is 1 case in 2 million people [4]. There are also traumatic OM or limited OM [8, 16], and in patients with spinal cord injury - neurogenic OM [3].
OM is not associated with muscle inflammation, so some clinicians prefer to call this disease heterotopic ossification. In 70-80% of cases, the disease is localized on the thigh, shoulder, or buttock [1, 8]. In most cases, the appearance of OM is preceded by a single or multiple blunt trauma [5, 6]. The time between injury and detection of muscle changes can vary from 3 weeks to 20 years.
The scientific literature presents isolated cases of OM m. masseter, m. temporalis, m. pterygoideus, m. buccinator, m. platysma, m. sternocleidomastoideus
[10, 14]. Damage to the OM of the masticatory muscles is often unilateral, but bilateral lesions have also been described [7]. Cases of OM of the masticatory muscles were observed after complex removal of the lower third molar [4, 16], 4-week intensive therapy of a cancer patient with developed sepsis, neuromyopathy and nephropathy [7].
The reason for bone formation in muscle is unknown [5]. The pathogenesis of OM remains unknown. One theory is that muscle injury stimulates the proliferation of fibroblasts, which then undergo bone metaplasia. There is also a widely discussed theory that skeletal muscle injury induces the expression of bone morphogenetic protein at the injured site, which in turn stimulates primitive stem cells to differentiate into osteoblasts, leading to heterotopic ossification [16, 17]. According to E. Shore et al. [13], progressive OM is caused by a mutation in the gene encoding activin type kinase, which leads to changes in chondro- and osteogenesis [2, 12].
To date, the pathomorphology of ossification of the masticatory muscles and the differential diagnosis of OM have not been sufficiently studied.
The purpose of the study was to study the morphological features of OM in cases of damage to the masticatory muscles.
Material and methods
The study included 8 patients (3 women, 5 men) aged from 19 to 60 years (average age 33.8 years). When contacted, all patients complained of severe limitation of mouth opening and impaired chewing function. According to the anamnesis, 7 patients had a previous injury to the maxillofacial area; in 1 patient, the restriction of mouth opening was not associated with anything. The duration of the disease ranged from 1 to 12 months.
All patients underwent clinical, radiological, and laboratory examinations. In 7 patients, surgical treatment was performed with subsequent examination of the surgical material. The postoperative period proceeded without complications. Patients were prescribed symptomatic therapy, mechanotherapy, and physiotherapy. One patient refused surgery.
The surgical material was fixed in a 10% solution of neutral formaldehyde, decalcified in Biodek R solution, passed through alcohols of increasing concentrations, embedded in paraffin and microtomized. Histological sections were stained with hematoxylin and eosin, picrofuchsin according to Van Gieson.
Results and its discussion
In 7 patients, unilateral traumatic OM was detected with damage to only the masticatory muscles: m. pterygoideus lateralis
- at 1,
m.
temporalis - at 2,
m.
masseter - in 4. One patient with OM
m.
pterygoideus medialis denied any history of trauma. The duration of the disease was: 1 month - in 2 patients, 2 months - in 2 patients, 3 months - in 1 patient, 6 months - in 2 patients, 12 months - in 1 patient.
The reason for the patients’ referral was a persistent limitation of the mobility of the lower jaw, which interfered with eating and speech. The maximum mouth opening was 5-15 mm. When opening the mouth, the lower jaw shifted towards the affected muscle, sometimes with a clicking sound in the temporomandibular joint. There was no pain syndrome. Skin color was not changed. When m. is affected. temporalis
and
m.
masseter, a painless, non-displaceable area of tissue compaction with clear boundaries was determined by palpation.
Palpate m.
pterygoideus was not possible during clinical examination. No characteristic clinical symptoms of OM were identified.
Computed tomography excluded lesions of the temporomandibular joint and identified areas of ossification in the affected masticatory muscles with clear boundaries. Surgical treatment of 7 patients made it possible to restore the function of the lower jaw and chewing. No relapses of OM were observed.
Microscopic examination revealed different morphological structures of OM nodes in the masticatory muscles. Thus, a 19-year-old patient with a traumatic lesion of m. masseter
on the left 6 months ago, a node with well-formed bone beams, loose connective tissue with a small amount of intertrabecular tissue with weak calcification was microscopically determined
(Fig. 1).
Figure 1. Patient 19 years old. Myositis ossificans. Microphoto. Hematoxylin and eosin staining. ×400. a - formed bone beams among fibrous tissue, b - separated by a layer of loose connective tissue, bone beams with signs of degeneration. Fibrous tissue smoothly transitioned into bone tissue. Muscle fibers with signs of dystrophy.
A 60-year-old patient with damage to m. masseter
on the right, 6 months ago (after tooth extraction), a node was microscopically identified, delimited from the surrounding muscle tissue by coarse fibrous connective tissue
(Fig. 2).
Figure 2. Patient 60 years old. Myositis ossificans, zoning phenomenon. Microphoto. Hematoxylin and eosin staining. ×100. A delimited node (a) among fibrous tissue with a large number of fibroblasts (b) with areas of hyalinosis formed by bone beams (c) with signs of degeneration.
Muscle fibers with dystrophic changes. In the center of the node, fibrous tissue with proliferation of fibroblasts was detected. The middle zone is represented by immature osteoid and developing cartilage and bone tissue. The periphery of the node contained stroma with collagen fibers and a large number of bone beams. The “zoning phenomenon” was microscopically revealed.
A 44-year-old patient with a traumatic lesion of m. temporalis
on the left 12 months ago, OM in the mature stage was detected
(Fig. 3).
Figure 3. Patient 44 years old. Myositis ossificans. Microphoto. Hematoxylin and eosin staining. ×100. a — areas of degeneration of striated muscle fibers, b — a focus of bone tissue with signs of necrosis.
The microscopic picture was characterized by the presence in the muscle tissue of areas of bone structures with signs of necrobiosis. Muscle fibers are dystrophically changed. The node contained well-differentiated bone beams of irregular shape, randomly located areas of osteoid with weak calcification. The “zonal phenomenon” was absent.
OM is characterized by the appearance of a dense, immobile, painless node on palpation. The diagnosis of traumatic OM is based on the history of trauma (although in only 70% of cases patients report the presence of a blow), clinical symptoms, radiological signs and microscopic examination of biopsy material. Patients with OM of the masticatory muscles are characterized by limited mouth opening [11, 15]. According to R. Wiggins et al. [16], the development of traumatic OM goes through several histological phases: 1) early phase - rapid proliferation of fibroblasts; 2) intermediate phase - formation of osteoid, appearance of zoning; 3) the last phase is the formation of spongy bone and fat on the periphery.
The microscopic picture of OM is characterized by a significant diversity of tissue structures [1]. In the early stage, hemorrhages are observed among the fibrous connective tissue, foci of myxomatosis, angiomatosis, chondromatosis, and foci of calcification. Fibroblasts and fibrocytes in some places form clusters in large numbers. Fibroblasts are large or irregular in shape with a hyperchromic nucleus and granular cytoplasm. Mitotic figures are few in number. Inclusions of fat cells and foci of hematopoiesis may be observed. Foci of bone formation are observed at various stages of maturation. These may be areas of enchondral ossification, osteoid with varying degrees of calcification, and randomly arranged formed bone beams, often surrounded by osteoblasts.
In the mature stage of OM, the zoning of the structure is determined [1, 5, 8, 16]. The central zone is represented by undifferentiated spindle-shaped cells with abundant mitoses of fibrous, bone marrow tissue and necrotic muscle tissue. The middle zone with active osteoblasts, immature osteoid, developing cartilage and bone tissue is separated by thin-walled vascular canals [5, 16]. Along the periphery of the node there are well-differentiated bone beams with mature cancellous bone, osteoclasts and stroma containing collagen fibers [8]. The node is separated from the surrounding tissue by a layer of coarse fibrous connective tissue with cartilaginous areas and bone beams oriented along the periphery [1, 16]. The node contains bundles of muscle fibers, individual fibers with dystrophic changes, and myoblasts with eosinophilic cytoplasm.
The zonal architectonics of the histological structure of the OM in cases of damage to the masticatory muscles is described by many researchers [1, 5, 8, 16]. In a histological study of the OM of the masticatory muscles, S. Meng et al. [9] in 5 cases found zonal changes in areas of muscle ossification; in 10 cases there was no zonation. Our study also identified cases of zonal and non-zonal structure of the OM node in cases of damage to the masticatory muscles.
Conclusion
Features of the morphological structure of the OM: abundance of osteoid, immature unevenly mineralized bone trabeculae with round osteoblasts and osteoclasts in the vascular base. These structures are also detected in osteoid osteoma and osteoblastoma, but in them there is “reverse zoning”, i.e. mature bone in the center and immature osteoid with cell proliferation at the edge.
OM must be differentiated from benign connective tissue tumors, osteoma, osteoblastoma, osteosarcoma, nodular fasciitis, rhabdomyoma, chondroma, osteochondroma [1, 16].
Thus, the OM of the masticatory muscles has a different morphological structure with the presence or absence of zonation during tissue ossification. Proposed by E.L. Neustadt and A.B. Markochev [1] differential signs of OM: 1) absence of spicules, Codman’s triangle during X-ray examination, 2) a small number or absence of mitotic figures in cells, 3) a large number of mature bone beams, 4) zonality of the microscopic structure, - must be supplemented with an inconsistent sign of zonation node with damage to the masticatory muscles, persistent impairment of the mobility of the lower jaw without pain.
How long does it take to cure trismus?
Typically, full muscle recovery can take one to three weeks, depending on the cause of the trismus. More time will be needed for fractures of the jaw, which must heal properly and subsequently develop.
To prevent trismus of the masticatory muscle, you must:
- do not cause diseases of teeth and gums;
- get vaccinated against rabies and tetanus (rabies and, as a result, lockjaw can be fatal);
- In case of blows or damage to the jaw, seek emergency help from dentistry;
- avoid stressful situations, nervous tension;
- when engaging in contact sports, wear special helmets and mouthguards for protection;
- undergo regular preventive examinations with a trusted dentist. These are the doctors who work in the 32 Dent network of clinics, where you will be happy to see you at any time. Contact us!
What is muscle spasm, its types and causes
Muscle spasms are involuntary contractions of muscle tissue. Unlike natural contractions (for example, during the digestion of food, during exercise, swallowing water), spasms occur without any external or internal cause, in the absence of a person’s desire, and unpredictably.
As a rule, muscle spasms in the head area affect the temples, forehead, and back of the head. Involuntary contractions of the masticatory muscles can occur due to the use of stimulants (caffeine, taurine, narcotics) or for internal physiological reasons. In the second case we are talking about:
- trismus - a spasm that provokes a tight clenching of the jaws;
- bruxism - involuntary muscle contractions that occur mainly during sleep, at night, and are accompanied by grinding of the upper and lower rows of teeth.
Muscle spasms in the cervical spine can be either unilateral or bilateral. They are often associated with pinched nerves or spinal pathologies (for example, a hernia).
Advantages
Smart medicine for smart people
Safe, effective and natural rejuvenation
The best technologies for communicating with patients
We don't just take care of your beauty - we recharge you!
Types of head muscle spasms:
- episodic involuntary muscle contractions: headache, neck muscle pain lasts no more than 14 days over a period of 1 month;
- chronic spasms: 15 days a month or more.
Typically, the causes of spasms in the muscles of the head, jaws, and neck are:
- metabolic disease;
- lack of physical activity;
- diseases of the musculoskeletal system;
- vascular pathologies;
- deficiency of vitamins, microelements;
- stress: physiological, psychological, emotional stress;
- hypothermia;
- increased body temperature;
- obesity;
- genetic predisposition;
- injuries;
- pinching of nerve fibers.
Features of treatment for older patients
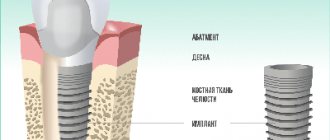
Among the common age-related changes in the lower jaw, changes in the content of water, organic and inorganic substances are noted, osteoporosis, atrophy and thinning of bone tissue are often detected. In addition, older patients often have concomitant diseases, such as diabetes. All of these factors can greatly limit treatment options. For example, if dentures are required, then in some situations the dentist may only offer removable dentures. Placing implants will be risky and ineffective.
Nevertheless, modern dental capabilities make it possible to find a way out of any, even the most difficult situation. A wide variety of materials and techniques can eliminate existing problems and significantly improve the patient’s quality of life.
Prevention
The main preventive measure to prevent the manifestation of severe pain in the jaw is a timely visit to the doctor. If any minor deviations occur, you should immediately consult a specialist. Early identification of the cause of a pathology that begins to develop is the first step towards solving the problem.
The patient should already be alerted by the appearance of unpleasant sensations and discomfort in the form of:
- deterioration of jaw mobility;
- crunching while yawning or chewing food;
- pain when opening the mouth;
- noise or pain in the ears;
- frequent headaches;
- grinding or creaking of the jaw;
- painful sensations in the neck and back.
Such symptoms are a reason to undergo diagnostic measures and, after diagnosis, receive the necessary treatment.
What to do if the lower jaw is inflamed
First of all, it is important to identify the symptoms of the problem. One of the very first and most obvious is an increase in soft tissue volume.
This can be either a slight swelling or a very large tumor-like formation. Other symptoms may include:
- Increased body temperature.
- Redness of the skin.
- Painful sensations.
- Incomplete opening or closing of the jaw.
- Sensation of a foreign body in the throat.
- Difficulty chewing or swallowing.
- Hearing loss.
If the symptoms are confusing and it becomes unclear which doctor you need to see, you can make an appointment with a therapist who will conduct an initial examination, examine the complaints and issue a referral to the right specialist.