From this article you will learn:
- methods of treating pulpitis in dentistry,
- how to remove a nerve from a tooth - video, stages of therapy,
- Is it painful to remove a nerve from a tooth?
Pulpitis is an inflammation of the neurovascular bundle located inside the tooth, which in dentistry is called the term “dental pulp.” The neurovascular bundle is located in the center of the tooth (in the cavity that dentists call the pulp chamber), as well as in the root canals. Through the tips of the root canals, the vessels and nerves of the pulp anastomose with the vessels and nerves outside the tooth. The name of such a disease as pulpitis arose from a combination of the word “pulp” and the ending “it” (the latter denotes the presence of inflammation).
In an article devoted to the reasons for the development of pulpitis (you can read them at the link above), we have already written that the main reason is long-term dental caries. As a result of the carious process in the hard tissues of the tooth, a carious cavity is formed, the walls of which contain a large amount of infection. When the thickness of healthy tooth tissue separating the pulp from the carious cavity becomes thin, the infection will begin to penetrate into the tooth cavity, causing inflammation of the pulp.
Inflammation of the pulp produces characteristic symptoms – pain. In most cases, treatment will require removal of the inflamed pulp from the tooth cavity and root canals, but in some cases conservative therapy is also possible. The latter is possible only in the early stages of inflammation and in certain groups of patients (we will also discuss this below).
What does the removed tooth pulp look like?
Symptoms of tooth pulpitis -
Pain with pulpitis can be of varying degrees of severity - from minor pain, which is provoked by thermal irritants, to acute paroxysmal spontaneous pain, which makes you want to climb the wall. Given the difference in symptoms, it is customary to distinguish 2 forms of this disease. Below we have described what pulpitis symptoms and treatment will have in each of these cases.
- Acute form of pulpitis – this form is characterized by acute paroxysmal pain that occurs especially at night.
It is typical that the pain increases, while pain-free intervals become shorter and shorter. As a rule, pain occurs spontaneously, i.e. without the participation, for example, of thermal stimuli. However, during the pain-free interval, in some cases it can be provoked by cold or hot water. With pulpitis, it is typical that after the removal of the irritant, the pain persists for about 10-15 minutes (this makes it possible to distinguish pain with pulpitis from pain with deep caries). With the latter, the pain stops immediately after the cessation of exposure to the stimulus. Very often, patients cannot even indicate which tooth exactly hurts, which is due to the irradiation of pain along the nerve trunks. The pain increases due to the gradual transition of inflammation from serous to purulent. With the development of purulent inflammation in the pulp, the pain becomes pulsating, shooting, and pain-free intervals almost completely disappear.
- Chronic form of pulpitis - in this form the inflammation is unexpressed. Patients usually complain of slight aching pain, most often arising from exposure to heat and cold irritants. Sometimes, by the way, with this form of pain there may be no pain at all. Keep in mind that the chronic form of pulpitis can periodically worsen, and during periods of exacerbation of inflammation, the symptoms will be exactly the same as in the acute form.
Rinse
To relieve pain caused by inflammation of the pulp, rinsing with tinctures or decoctions of medicinal herbs is often used at home. This procedure has many advantages:
- relieves pain;
- reduces swelling and itching;
- eliminates pathogens;
- prevents the spread of the inflammatory process to healthy tissue.
For rinsing to be beneficial, it is necessary to repeat it after 2-3 hours and use water at a temperature comfortable for the oral cavity.
.
To prepare medicinal decoctions, dentists recommend using various plants: chamomile, dry sage, oak or willow bark, elderberry.
Sage
To prepare the decoction, you need to pour 5 tablespoons of dried sage with two glasses of hot water, bring to a boil over the fire and continue to simmer for 35-40 minutes. The liquid should sit for at least two hours, after which it should be strained, cooled and used to rinse the mouth every 2.5-3 hours.
A decoction of sage will help reduce fever, reduce pain and eliminate pathogenic microorganisms from the carious cavity.
willow bark
The peeled willow tree bark is thoroughly crushed using a grater or a sharp knife, after which two tablespoons of this substance are poured into a glass of boiling water and left for 40-50 minutes.
A well-strained product can be used to rinse the mouth to relieve pain, inflammation and swelling. Rinsing should be done less than three times a day, preferably after eating.
Bay leaf
The leaves of the bay tree must be thoroughly crushed, then pour a tablespoon of the resulting crumbs with a glass of boiling water and leave for about two hours.
The liquid filtered through gauze is used to rinse the painful area of the mouth three to five times a day. The resulting medicinal solution helps reduce swelling of the gums, reduce the number of bacteria and slow down the development of the inflammation process.
Knotweed and elderberry
To prepare a healing decoction, dried elderberry and knotweed flowers are crushed, then mixed in a small container, a full tablespoon of each herb, and poured with a liter of boiling water. The solution, steeped for one hour, is filtered and used to rinse teeth every 2-3 hours.
This medicinal composition has antiseptic, anti-inflammatory and analgesic effects.
Pomegranate peel
The peel of one or two pomegranate fruits must be cut, pour a liter of boiling water and simmer over low heat for 2 hours. After cooling, the liquid is filtered and used for rinsing every three hours.
This remedy helps prevent the progression of the disease and relieves the pain associated with it.
Propolis with calamus
The solution is prepared as follows:
- 3 tablespoons of dry propolis must be thoroughly crushed;
- the resulting mass should be poured with alcohol in an amount of 100 ml and left in a dark place for 3-4 days;
- Add calamus tincture to the strained alcohol infusion at a ratio of 1:2.
To rinse the mouth, you need to dilute a tablespoon of the prepared infusion with a glass of boiled or filtered water.
The effect of the product is to disinfect the cavity present in the molar and reduce inflammation of the gum tissue.
Soda
To prepare the solution, a teaspoon of soda is dissolved in a glass of boiling water. After the liquid reaches room temperature, rinse the oral cavity thoroughly, especially the area of inflammation. It is important to rinse at least three times a day, half an hour after meals.
A soda solution helps to disinfect the affected area of soft tissue, relieve inflammation and reduce pain.
Peroxide
Rinse the mouth with an aqueous solution of hydrogen peroxide three times a day. They will help eliminate infection from the carious cavity, reduce the number of pathogenic organisms in the mouth, thereby preventing the progression of the disease.
Treatment of tooth pulpitis: methods
Treatment of pulpitis is most often carried out by depulping the tooth. This method involves completely removing the nerve in the tooth, after which the doctor mechanically expands and then fills the root canals. In young patients (provided they apply at an early stage of inflammation), it is possible to carry out treatment while preserving the living pulp of the tooth.
Of course, it is best to leave the nerve alive, because pulpless teeth become more fragile and also change their color to a grayer color. However, in most cases, the use of biological methods for treating pulpitis is impossible, because Patients extremely rarely apply at the very beginning of pulp inflammation (when the first symptoms have just appeared). Age also plays a decisive role in the choice of this method - this method is indicated for use only in people under 25-27 years of age.
Below we will talk in detail about the traditional treatment of pulpitis (read about the conservative method in the link above). By the way, according to official statistics, treatment of pulpitis is carried out poorly in 60-70% of cases, which requires subsequent retreatment of the tooth. This is due to poor-quality root canal filling.
Is it painful to treat pulpitis?
Pulpitis is actually an acute inflammation of the nervous tissue, so any manipulation of a diseased tooth can cause significant discomfort to the patient. However, the use of modern painkillers can reduce pain to a minimum. The least painful are conservative and devital surgical methods of treatment. Sometimes pain may persist for some time after treatment; in this case, the doctor may prescribe the patient to take painkillers. However, severe or prolonged pain after pulpitis treatment is often a sign of improper treatment and requires a second visit to the dentist.
Prevention of pulpitis is compliance with the rules of oral hygiene. Use toothpastes with sufficient mineral content, since thinned enamel is less resistant to initial caries and, as a result, inflammation of the pulp. Thus, Asepta Plus remineralization toothpaste will provide additional supply of minerals to the tooth, which is an excellent prevention of diseases of the teeth and gums.
How to remove a nerve from a tooth - video, stages
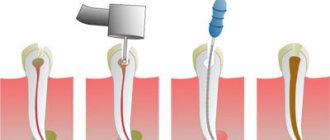
Removal of the tooth nerve is a classic method of treating pulpitis. Its essence lies in the following steps:
- drilling out all tissues affected by caries (Fig. 2),
- removal of dental pulp (carried out using a special instrument),
- mechanical expansion of channels (Fig. 3),
- filling of tooth root canals (Fig. 4),
- filling the coronal part of the cube (Fig. 5).
Treatment of pulpitis: stages of tooth depulpation
Below we will describe in more detail each stage of treatment for pulpitis; perhaps this information will help you identify a would-be dentist and prevent poor-quality treatment and its complications.
Reasons for the development of chronic pulpitis
Factors affecting the dental nerve: caries and its consequences, trauma, illiterate dental intervention, diseases of the lymphatic system, increased wear of teeth, periodontal pathologies. However, the causes of the chronic condition are late diagnosis of infection and late treatment. The peculiarity of pulpitis: many forms occur without obvious symptoms; the patient turns to somatology when the pain cannot be removed with pharmaceutical anesthetics. As a result, upon examination, the doctor sees that the pulp chamber, at best, is affected by bacteria, inflamed, and at worst, filled with pus, which can penetrate the blood channels.
Algorithm for the treatment of pulpitis using a specific example -
If you have pulpitis, treatment of a single-rooted tooth with one canal is usually carried out in 2 visits (at the second visit a permanent filling is already placed). In multi-rooted teeth, which have a significantly larger number of canals (from 2 to 4), pulpitis treatment is carried out in 3 visits.
The rule is categorical - a permanent filling on a tooth is not placed in the same visit as the root canal filling, i.e. The filling material in the root canals must first harden (moisture evaporates). Only after this can a permanent filling be placed. But to save time, some dentists neglect this. Below we will look at the algorithm for treating pulpitis of a multi-canal tooth in three visits.
What is pulpitis and how does the disease progress?
Pulpitis develops when carious destruction of the integrity of the tooth occurs when food and microorganisms penetrate the tooth cavity (pulp). Another way of developing the disease is infection from neighboring affected teeth through blood vessels, which occurs much less frequently and is called retrograde pulpitis. There are other, rare pulpitis:
- Traumatic, develops as a result of a crack, break, or chip of a tooth.
- Concrete occurs when there is excessive deposition of mineral formations that begin to replace the internal tissues of the tooth.
- Inflammation develops due to incorrect treatment, the use of low-quality materials, and accidental opening of the pulp.
Regardless of the type of infection, inflammation requires immediate treatment. Among the factors that increase the likelihood of developing pulpitis are: insufficient hygiene, osteoporosis and diabetes.
There are three stages of pulpitis: acute, chronic and aggravated chronic pulpitis. According to the ICD-10 classification used when making a diagnosis, the disease is divided into several categories.
Pulpitis acute
- K04.00 - initial inflammation of the pulp.
- K04.01 - acute focal pulpitis.
- K04.02 - purulent abscess.
The diagnosis is made when the pulp first comes into contact with infection. This includes the serous form of the disease, focal and purulent abscess.
First, the tooth becomes sensitive to temperature: hot or cold. Unlike caries, pain does not subside when the irritant is removed. Then comes the diffuse phase - the pain intensifies at night, is periodic, and often radiates to the temple or other parts of the face. With the transition to the chronic phase, the pain disappears, or is characterized by the patient simply as an unpleasant sensation.
Chronic pulpitis
- K04.03 - fibrous.
- K04.04 - gangrenous.
- K04.05 - pulp polyp.
Chronic pulpitis occurs after the acute phase of the disease. It is characterized by (irreversible) destructive changes in tissues, divided into three types according to the type of changes:
- Fibrous
- the most common sluggish form of chronic pulpitis. It is characterized by the growth of connective, fibrous-granulation tissue in the pulp.
- Gangrenous
- This is a putrefactive inflammation, which is marked by a characteristic odor from the mouth. The gums often swell, and fistulas may form through which exudate flows out.
- Hypertrophic
- the most rare pulpitis, characterized by the growth and exit of the pulp into the carious cavity.
The chronic form is not painful, but severe pain may occur periodically.
Note! In the acute stage, the infected tooth mainly reacts to cold; in the chronic form, the source of pain is exposure to high temperature.
Complicated forms
- K04.1 - pulp necrosis.
- K04.2 - pulp degeneration.
By complicated course of the disease we mean both inflammation of the entire pulp and simultaneous damage to several canals. When the pulp degenerates, denticles are formed - dense mineral formations (stones). They cause pain when there is a sudden change in body position, as this causes them to shift. For example, such patients experience pain when flying, going up in an elevator, or playing sports.
Necrosis refers to the death of cells in the neurovascular bundle of the dental root. In fact, this is the final stage of the disease. Necrosis can occur due to pulpitis, damage to the blood supply to the tooth, or under the influence of toxic components of the filling material.
First visit:
Anesthesia or is it painful to remove a nerve from a tooth?
How painful is it to treat pulpitis: It is definitely very painful if you decide to do it without anesthesia. Fortunately, modern anesthetics can completely solve this problem. If you still feel pain after anesthesia, this may be due to the anesthetic not being strong enough or the anesthesia technique being used incorrectly. The latter usually happens when the doctor tries to anesthetize large molars in the lower jaw (mandibular anesthesia, which is complex in technique, is performed there).
An example of anesthesia (video) –
Drilling out all carious tissues with a drill -
Firstly, at this stage all carious tissue is removed. Secondly, healthy tooth tissues are also partially removed, namely all tooth tissues above the pulp chamber and the mouths of the root canals. This is necessary to ensure visualization of the root canal orifices and ease of their processing with instruments. In Fig. 6-7 you can see the boundaries of excision of hard tooth tissues in the treatment of pulpitis. Figure 8 shows a view of the root canal mouths after they have drilled into the required amount of tooth tissue.
Tooth isolation from saliva –
This is done using a rubber dam. Isolation is necessary to prevent infection from the oral cavity from getting into the root canals along with saliva. This is standard international practice, but in Russia a rubber dam can often be seen only when a doctor fills a tooth. Normally, any work with root canals should be carried out using a rubber dam.
Removal of pulp from the tooth crown and root canals –
It is carried out with special tools designed to work in canals.
In Fig. 9 you can see tooth pulp wound around such a tool. By the way, video 1, which we posted above, shows the process of pulp removal. The video below clearly shows the moment when the tooth pulp is removed from the root canal (time – 1 minute 5 seconds). Treatment of pulpitis: video of nerve removal from a tooth
Measuring the length of root canals in a tooth –
This is one of the most important stages, because... if the length of each channel is determined incorrectly, it will cause -
- or underfilling of the canals, which will lead to complications after the end of treatment,
- or refilling the canals, which can lead to long-term pain and injury to the mandibular nerve.
Measuring the length of the canals is ideally carried out using a combination of the x-ray method and the use of an “apex locator”. In this case, first, special K-file instruments are introduced into each root canal in turn (Fig. 10), which are connected to the apex locator using a thin electrode (Fig. 12). The K-files are gradually advanced deeper into the root canal until there is a signal on the apex locator screen that the tip of the instrument has reached the apex of the tooth root.
It is necessary to measure each channel in turn, because The length of each channel is unique and there are no exact standards. After the measurements are completed and the data are recorded, K-files are simultaneously inserted into all channels (each to its own depth), and a control x-ray is taken (Fig. 11). The apex locator sometimes makes mistakes, so the x-ray will show how accurately the length of the canal was measured and whether adjustments are needed.
Mechanical processing of channels –
A budget option for mechanical treatment of root canals involves the use of manual files (K-files or reamers) - in Fig. 13 you can see a K-file in the root canal. The dentist rotates this instrument by the handle with his fingertips, and the cutting edges of the instrument excise chips from the walls of the canal, expanding it. The purpose of mechanical treatment is to widen the canal so that later it can be properly filled.
A better and more expensive processing option involves the use of an endodontic micromotor and special nickel-titanium files with shape memory. Mechanical processing of each channel is carried out to the depth determined at the previous stage. This is necessary to ensure that each root canal is filled exactly to the root apex. During the expansion process, it is very important to constantly rinse the canals with antiseptics, which is necessary for disinfection, but first of all, to wash out the shavings from the canal (24stoma.ru).
Mechanical treatment of root canals:
In video 1, you can see in detail how the expansion of root canals is carried out with ordinary hand instruments (for this, hand-held K-files of different diameters are used - from smaller to larger). In video 2, the dentist processes root canals using an endodontic micromotor and ProTaper Gold nickel-titanium profiles.
Placing a temporary filling –
After the canals are washed and dried to remove excess moisture, turundas soaked in antiseptic are left in them, and a temporary filling is applied to the tooth. The cost of treatment is calculated based on the number of root canals in the tooth.
Second visit:
By the way, it is preferable to fill root canals without anesthesia, but this is not necessary. This is due to the fact that if a slight pain occurs when filling the canals, the doctor immediately understands that he has moved the gutta-percha pin beyond the apex of the root. Accordingly, the doctor can change the filling depth in time.
- Removing a temporary filling.
- Flushing the canals with antiseptics.
- Filling canals using gutta-percha and sealer - after the root canals have been washed and dried, it is necessary to seal them tightly.
This is done using gutta-percha pins of different sizes (Fig. 16) and a sealer (this is something like a paste). The pins are inserted into the root canals and compacted there. In Fig. 14-15 you can see the mouths of the root canals Before and After the canals were filled with gutta-percha. Read more about this stage in our article: → “Mechanical treatment and filling of canals for pulpitis”
- X-ray control of the filling ( required!!! ) if everything is OK on the x-ray, we proceed to the next stage.
But, if we see that the canal is not filled up to the apex, or the gutta-percha pins extend beyond the root into the surrounding tissues, it is necessary to remove all the gutta-percha pins and start filling the canals all over again. In Fig. 17-19 you can see well-sealed root canals (all root canals are sealed to the apex of the root). Unfortunately, it is worth noting that the vast majority of dentists, even if they see that the root canals are filled, do not redo the work. This is precisely what is connected with the percentage of poor-quality treatment of pulpitis that we announced at the beginning of the article (in 60-70% of cases). Type of high-quality filled root canals –
At the end of the visit, a temporary filling is placed, and the patient is warned that the tooth may begin to hurt after undergoing anesthesia. Good tablet analgesics will help relieve pain. A little pain is normal because... during instrumental work in canals, K-files slightly injure the tissue in the area of the root apex.
Quick ways
If you experience severe pain in the tooth area in the evening or on holidays, when you cannot see a dentist, you must use medications that are often present in the family medicine cabinet:
- Non-steroidal anti-inflammatory drugs . In addition to quickly eliminating pain, these drugs help relieve inflammation, reduce swelling of soft tissue and reduce elevated body temperature. The most common drugs in this group are Nurofen, Diclofenac, Ibuklin, Ibuprofen.
- General painkillers help to quickly relieve acute pain for a period of up to 5-6 hours. These include Ketanov, Pentalgin, Nimesulide.
- Antibacterial and local anesthetic agents .
If you have a carious cavity that has caused the development of pulpitis, you should use antimicrobial drugs such as Metrogildent ointment, Betadine cream, Dentinox dental drops. They will help neutralize pathogenic microflora that develops in a damaged tooth and leads to the development of an inflammatory process. - Clove oil . This component has a pronounced anesthetic effect. To relieve pain when the integrity of the tooth is not damaged, applications with this substance are used. 4-5 drops of oil are applied to a cotton pad, which is applied to the site of inflammation for 7-10 minutes. If there is a carious cavity, you can apply a few drops into it.
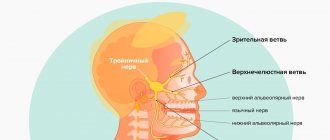
- The analgesic drug Finlepsin is used in case of inflammation of the ternary nerve and the presence of various acute pains, including dental pain. Helps eliminate discomfort and improve mood.
We will talk about the symptoms and methods of treating inflammation of the facial trigeminal nerve in the next article. And here is a list of strong painkillers for toothache.