How do we treat sinusitis?
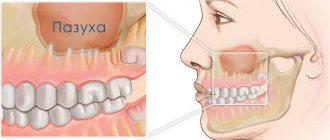
Sinusitis (sinusitis) is inflammation of the maxillary sinuses. Microorganisms (bacteria or viruses) enter the maxillary sinus through the nose or through the bloodstream and cause inflammation of its mucous membrane, often accompanied by the accumulation of pus in the sinus. To drain pus, “punctures” are used - punctures of the maxillary sinus. Unfortunately, many patients, fearing such “punctures,” delay seeing a doctor for sinusitis, thereby harming themselves: creating the threat of developing severe complications of sinusitis associated with the possible spread of infection, as well as conditions for the formation of chronic sinusitis.
What is a cyst in the maxillary sinus called?
A maxillary sinus cyst is a benign formation that has a hollow structure containing fluid inside. Cysts of the maxillary sinuses are quite common, but are almost always found at random. Their location and origin may differ, which will determine the characteristics of the clinic and even treatment.
Odontogenic cyst
Among the many benign tumors of the jaw tissue, the cyst is found most often and represents a pathology quite dangerous for the bone structure. Odontogenic formations in the vast majority of cases remain undiagnosed for a long time, and therefore reach enormous sizes. The growth of the cyst provokes atrophic processes in the bone tissue, which thins, becomes fragile, and then disappears completely.
Such formations are characterized by a long latent course until the cavity grows to gigantic proportions. Then a characteristic crunch begins to be noted in the jaw, especially during chewing loads. Ignoring the problem leads to spontaneous fractures of the jaw, compression of the maxillary sinus with disruption of its functions, exacerbation of the inflammatory process with damage to the structures of the maxillary sinus and the formation of sinusitis.
Tooth cyst growing into the maxillary sinus
Damage to the dental canal involving the root and surrounding tissues is a consequence of an infectious process of bacterial origin. In the absence of adequate and timely treatment, a gradual delimitation of the inflammatory reaction from healthy tissues by a wave of cellular structures occurs.
This creates a cavity called a dental cyst. It gradually increases and destroys the bone tissue of the jaw. When localized in the anterior part of the upper jaw, gradual penetration into the maxillary sinus occurs.
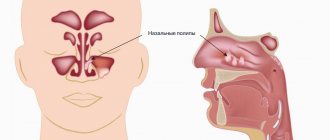
Retention
The most common form of neoplasm in the maxillary sinus, which is also called a true cyst. It is located in the lower wall of the sinus and has an epithelial lining - a distinctive feature of true cystic cavities. The formation is clearly determined by X-ray examination randomly, as it does not manifest itself clinically.
When the cyst reaches a significant size, problems begin with the functioning of the maxillary sinus. The structure and physiology of the microvasculature is disrupted, resulting in the formation of edema. This symptom is manifested by nasal congestion, often without pronounced discharge from it. Due to the lack of specificity of the clinical picture, even the presence of subjective signs of the disease is not a reason to consult a doctor.
Is it possible to treat sinusitis without a puncture?
Very often - yes. Subject to timely contact with an ENT doctor. At the initial stage of sinusitis, it is quite possible to do without a puncture. A “puncture-free” method of treating sinusitis is nasal lavage using the fluid displacement method (“cuckoo”) in combination with laser therapy. The rinsing procedure clears the nasal passages and nasal cavities of pus and mucus, and the laser relieves inflammation. The course is designed for 5-7 procedures. Already after the 1st procedure, patients see a significant improvement in their condition. Another way to avoid a puncture for sinusitis is to use a device that creates negative pressure in the nasal cavity, and thereby helps remove secretions from the maxillary sinuses. A modern method of ensuring outflow from the inflamed sinus and the possibility of carrying out therapeutic actions in it is balloon sinuplasty, performed in our center. It is possible to cure sinusitis without a puncture only if there is nasal discharge, indicating that there is an outflow of the contents of the maxillary sinus. Even the anatomical features of the structure of the ENT organs are important. That is, to determine the optimal treatment tactics for sinusitis, it is necessary to contact an otolaryngologist as early as possible. In our clinic, puncture-free treatment of sinusitis is possible!
- Without pain and blood
- Without piercing the maxillary sinuses
- In just an hour and a half
Healing sinusitis is a huge relief for your body.
Results and discussion
Analyzing the diagnostic images, we drew attention to the following anatomical feature of the structure of the cribriform plate of the ethmoid bone: the low location of the central sections (olfactory fossa) relative to the lateral ones (ethmoidal fossa) (Fig. 1).
Rice. 1. CT scan of the skull in coronal projection. The low location of the olfactory fossa on both sides is determined (indicated by arrows).
P. Keros (1965) identified three types of location of the cribriform plate: high - the cribriform plate is located below the roof of the ethmoidal labyrinth by 1-3 mm, medium - by 4-7 mm and low - by 8-16 mm [6]. However, these measurements were made relative to the medial edge of the ethmoid bone. We, in turn, measured the depth of the olfactory fossa from the line that connects the lateral edges of the ethmoidal fossa of the cribriform plate to the lowest point of the olfactory fossa (Fig. 2). With this measurement, the general direction of the cribriform plate (horizontal or oblique), which also characterizes the features of the anatomical structure of the ethmoid bone, has a significant impact on the objectivity of assessing the depth of the olfactory fossa.
Rice. 2. CT scan of the skull in coronal projection. Landmarks for measuring the depth of the olfactory fossa are shown: a line connecting the medial edges of the ethmoidal fossa and arrows pointing to the lowest points of the olfactory fossa.
In 42 patients with SNL, a low location of the olfactory fossa was found - 7.2±1.8 mm below the level of the ethmoid. In 13 cases, attention was drawn to the asymmetrical location of the reticular plate, and the localization of the SNL corresponded to the side of the lower position of the olfactory fossa (Fig. 3). In 30 cases, fenestration of the cribriform plate was observed over 1-5 mm. The fistula was most often localized in the central sections of the perforated plate (in the area of the olfactory fossa).
Rice. 3. CT scan of the skull in coronal projection. Asymmetrical location of the olfactory fossa, lower on the side of development of the SNL (indicated by an arrow).
In one of the 34-year-old patients, SNL occurred after radical endoscopic surgery for right-sided polypous polysinusitis. A CT study demonstrated the absence of the anterior end of the middle turbinate and individual intercellular septa of the anterior cells of the ethmoidal labyrinth resected during the operation. In this case, the following variant of the anatomical structure of the ethmoid bone on the right was noted: the anterior cell at the base of the middle turbinate extended cranially and penetrated into the posterior sections of the frontal infundibulum; thickened mucosa and a horizontal fluid level were observed in it. In addition, there was a narrow bone defect (no more than 1 mm) of the lateral slope of the olfactory fossa on the right at the level of the posterior end of the cock's crest, opening into the cell of the frontal infundibulum described above. The perpendicular and cribriform plates of the ethmoid bone were covered with polyps with the presence of areas of periosteal ossification; local destruction of the septa of the ethmoidal labyrinth from the pressure created by the polyps was visualized.
Thus, in this case, the polyposis process led to the destruction of the ethmoid bone structures, the reticular plate in the area of the olfactory fossa was filled with polyps, which plugged the resulting bone defects, and after polypotomy, conditions were created for the leakage of cerebrospinal fluid (Fig. 4).
Rice. 4. CT scan of the paranasal sinuses of a 34-year-old patient: coronal (a) and axial (b) projections. The anterior end of the middle turbinate on the right is missing—a condition after its resection. Areas of periosteal bone formation and polyps are identified (indicated by a long arrow). The septa of the ethmoidal labyrinth are locally destroyed, and a defect in the olfactory fossa is revealed (indicated by a short arrow).
Ethmoidal meningocele was diagnosed in 2 patients. In one 37-year-old patient, a CT scan revealed a defect of up to 1.5 mm2 in the cribriform plate on the right in the area of the bottom of the olfactory fossa at the level of the middle cells of the ethmoid bone, through which an area of soft tissue density protruded between the nasal septum and the superior turbinate. At the same time, a small amount of cerebrospinal fluid density fluid was visualized in the right sphenoid sinus and sphenoethmoidal recess (Fig. 5).
Rice. 5. CT scan of the paranasal sinuses of a 37-year-old patient: axial projection (a) and reconstruction in the coronal plane (b): a defect in the olfactory fossa (indicated by arrow 1) and an ethmoidal meningocele with the contents of the cerebrospinal fluid density (indicated by arrow 2) are observed.
In one 45-year-old patient, a CT scan revealed a defect in the cribriform plate of the ethmoid bone on the right in the lateral sections with a length of up to 4 mm, the bone walls of the anterior cells of the ethmoid bone were thinned, and a soft tissue formation up to 10 mm in size was visualized in them (meningocele) (Fig. 6). In the right maxillary and frontal sinuses, and the nasopharyngeal vault, the contents of the cerebrospinal fluid density were determined.
Fig. 6. CT scan of the paranasal sinuses of a 45-year-old patient in the coronal projection. A bone defect of the cribriform plate (a, b; indicated by arrow 1), meningocele (b; indicated by arrow 2), and the contents of the cerebrospinal fluid density in the nasopharyngeal vault (c; indicated by arrows) were revealed.
In one 55-year-old patient, the occurrence of liquorrhea was caused by the presence of a mucocele of the anterior cells of the ethmoidal labyrinth, in which a thin-walled bone cavity was visualized on the right, which included a cell of the nasal tubercle and a ethmoidal bubble measuring 21x9 mm, filled with the contents of soft tissue density and extending to the perforated plate; its local destruction was noted in the area of the ethmoid fossa for about 4 mm (Fig. 7). The uncinate process and the infundibulum on the right were not clearly differentiated, and the frontonasal canal in the caudal sections was not traced. The right frontal sinus was hypoplastic and filled with pathological contents. A small amount of liquid content with a horizontal level was noted in the right maxillary sinus.
Rice. 7. CT scan of the paranasal sinuses of a 55-year-old patient: coronal (a) and axial (b) projections. a — local destruction of the reticular plate of the ethmoid bone at the location of the thin-walled bone cavity (indicated by an arrow); b — mucocele (indicated by an arrow).
In one 53-year-old patient, the development of SNL was caused by the presence of a space-occupying lesion in the right sphenoid sinus. On K.T. an enlarged (swollen) right sphenoid sinus was visualized, filled with a space-occupying formation with a density of up to 34 HU, spreading through the defect of the intersinus septum (mainly in the middle and upper sections, up to 11 mm in length) into the left sphenoid sinus (Fig. 8). The lateral wall of the right sphenoid sinus was destroyed for about 7 mm. Contents with air bubbles (mucus) were visualized in the posterior parts of the left sphenoid sinus. In the right maxillary sinus there was a small amount of liquid content of low density.
Rice. 8. CT scan of the paranasal sinuses of a 53-year-old patient in the axial projection. Destruction of the walls of the right sphenoid sinus (indicated by arrows 1 and 2) and a space-occupying formation (indicated by arrow 3) were revealed.
In some cases, it is possible to detect freely flowing cerebrospinal fluid through a defect in the cribriform plate, which looks like a linear area of lower density than the surrounding mucous membrane. In the presence of additional formations in the sphenoid sinuses and cells of the ethmoidal labyrinth, bone defects through which cerebrospinal fluid leaks occur are also clearly visualized. In such cases, information obtained from CT in the axial plane is sufficient.
In cases where defects in bone structures or dura mater were not clearly identified (44% of patients), nasal liquorrhea was diagnosed by indirect signs, such as thinning of bone structures without obvious destructive changes in combination with pathological contents of liquor density mainly in the posterior parts of the sphenoid sinuses and sphenoethmoidal recesses, as well as in the posterior cells of the ethmoidal labyrinth, less often in the maxillary sinuses. We performed dynamic CT examination in such patients. The primary examination was performed in the axial plane immediately upon admission of the patient to K.T.’s office. A repeat study was performed in the coronal plane 10-20 minutes after the initial one. Between the initial and repeat examinations, the patient was on the table in a supine or abdominal position. The time for repeat testing depended on the rate of cerebrospinal fluid flow: if more than 10 drops flowed in 1 minute, the test was repeated after 10 minutes, if less abundant, after 20 minutes. The amount of fluid in the sinuses listed above increased, and in some cases it was possible to trace a stream of cerebrospinal fluid (a linear area of lower density than the surrounding mucous membrane). In addition, we came to the conclusion that the very first anterior cell of the ethmoidal labyrinth, containing cerebrospinal fluid, corresponds to the level of localization of the fistula.
We did not perform CT cisternography on patients due to the rather high invasiveness of the procedure, the result of which was the entry of the contrast agent into the paranasal sinuses, which does not provide significant additional information, since the cerebrospinal fluid found in them during SNL has a natural contrast and is well differentiated against the background air without additional contrast. According to D.N. Kapitanova and A.S. Lopatin, CT cisternography can sometimes give false negative results due to an inadequate amount of contrast agent administered and poor timing of the study [7].
Causes and development of sinusitis
- rhinitis (runny nose) - infectious or allergic,
- deviated nasal septum (congenital or acquired)
- difficulty in nasal breathing due to hypertrophy of the nasal turbinates and adenoids (in children);
- the existence of foci of chronic infection in the body (for example, staphylococcus);
- weakening of the immune system.
ENT medical doctors have all the technical capabilities necessary to diagnose and treat sinusitis. Extensive experience and attentive attitude of doctors to your problem and your concerns will ensure timely and correct treatment of sinusitis at the modern level and prevent the development of complications. With a runny nose, inflammation of the nasal mucosa can also affect the mucous membrane of the maxillary sinus. There, mucus production, reproduction and accumulation of pathogenic microorganisms increase. The outflow of the contents of the nasal sinus is difficult due to the swollen nasal mucosa, which blocks the opening connecting the nasal cavity and the maxillary sinus. This is how sinusitis develops. The accumulation and stagnation of mucus leads to increased pressure on the walls, which is felt as pain. The formation of pus and the absorption of toxins produced by microbes cause symptoms of intoxication - fever, malaise, headache.
Symptoms and main complaints of sinusitis
- Runny nose, nasal discharge (if the drainage is not blocked), often due to yellowish-greenish pus
- Difficulty in nasal breathing
- Pain in the nose and inflamed maxillary sinus (right or left of the nose)
- General symptoms: fever, headache, weakness.
Sinusitis is confirmed by the results of radiography or computed tomography. As soon as the diagnosis of sinusitis is confirmed, full-fledged qualified treatment is required under the guidance of an ENT doctor (in no case self-medication!).
Acute sinusitis. Symptoms Treatment. Prevention.
- home
- For patients
- Articles
- Acute sinusitis. Symptoms Treatment. Prevention.
»
»
»
Some bones of the human skull are hollow formations, that is, they have sinuses inside (maxillary (maxillary), ethmoid, frontal (frontal), main (sphenoidal)). Inflammation of the mucous membrane of one or more of these sinuses is called the general term sinusitis (from the Latin sinus - sinus).
The largest sinus is the maxillary sinus.
The entry of a bacteria, virus or allergen into the sinus provokes the development of edema, the lumen of the sinus decreases, and an excess amount of mucus is formed, which disrupts the movement of air flow. Bacteria begin to multiply in the cavity, producing pus.
Sinusitis is an inflammation of the maxillary (maxillary) sinus.
Symptoms:
• Increased body temperature, chills.
• General malaise. • Runny nose (nasal discharge is usually mucous at first, and on the 5-7th day it becomes purulent). • Nasal congestion. • Sneezing. • Pain in the maxillary sinuses (infraorbital-buccal region), radiating to the teeth, forehead, and root of the nose. • Pain intensifies when bending the head forward, sneezing or coughing. • Nasality. • Decreased sense of smell.
Forms
According to the type of inflammation, they distinguish: • acute catarrhal sinusitis (viral) usually does not differ from a runny nose and is manifested by congestion, nasal discharge, and sometimes there is a slight heaviness in the buccal-infraorbital area. Acute catarrhal sinusitis can end in recovery or go into the second stage, that is, the stage of acute purulent sinusitis; • acute purulent sinusitis (bacterial) is characterized by the accumulation of pus in the maxillary (maxillary) sinuses. Facial pain becomes more intense, a headache occurs, and the patient’s general condition worsens significantly.
In any of the forms, sinusitis can be: • unilateral (inflammation of the sinus on one side); • bilateral (inflammation of the sinuses on both sides).
Causes
Acute sinusitis develops: • as a complication after acute respiratory infections; • in the presence of foci of infection in the nasopharynx (rhinitis (runny nose), tonsillitis (inflammation of the tonsils)); • against the background of disease of the teeth of the upper jaw (odontogenic sinusitis); • as a result of allergies; • as a result of injuries and wounds of the upper jaw (traumatic). A predisposing factor is also seasonal hypovitaminosis, that is, a state of decreased body tone due to a lack of vitamins (usually in the autumn-winter period).
Diagnostics
• Analysis of complaints and medical history: nasal congestion, thick nasal discharge (possibly green), headache or facial pain, aggravated by bending the head forward, nasal tone, increased body temperature, the presence of a runny nose or colds that preceded the disease, the fact of treatment by a dentist etc. • General examination: the presence of swelling in the cheek area; when pressing in the area of the maxillary sinuses, discomfort is noted - from increased sensitivity and mild pain to sharp pain radiating to the orbital area, etc. • Rhinoscopy - instrumental examination of the nasal cavity, during which signs of the development of the inflammatory process (swelling and redness of the mucous membrane, purulent discharge). • Endoscopic examination of the nose reveals pus in the middle meatus, which indicates the presence of purulent sinusitis. • X-ray diagnosis: in some cases, an X-ray of the maxillary sinuses shows the fluid level. • Diagnostic puncture of the maxillary sinus: the wall of the maxillary sinus in the nose is pierced with a special thin needle under local anesthesia. Then, using a syringe, the contents of the sinus are drawn out. When pus is obtained, the sinus is washed and a medicinal substance is injected into it. • Ultrasound of the paranasal sinuses is sometimes used as an alternative to x-ray examination. • Oropharyngoscopy (examination of the oral cavity) to identify carious teeth, assess the condition of fillings, etc. If necessary, a consultation with a dentist is indicated.
Treatment
Drug treatment: • vasoconstrictor drugs in the form of sprays or drops into the nasal cavity (drugs in this group relieve swelling of the mucous membrane and help remove stagnant fluid from the maxillary sinuses). The products are used in a short course, lasting 5-7 days; • nasal sprays containing antibiotics and steroid hormones (have an anti-inflammatory effect); • antihistamines, if the disease develops against the background of allergic reactions; • mucolytics – drugs that help liquefy the contents of the maxillary sinuses and, as a result, improve its excretion; • for purulent sinusitis, it is possible to prescribe antibiotics (in the form of tablets or injections).
Non-drug treatment. • Puncture (puncture) of the maxillary sinuses. The method allows you to quickly remove purulent contents (which leads to a rapid reduction in headache and facial pain, and improve your general condition) and inject medicinal substances directly into the sinus. Carrying out punctures of the maxillary sinuses in many cases allows you to do without prescribing antibiotics. • Rinsing the nose with saline, herbal and antiseptic solutions: The procedure can be carried out independently at home using special devices for a nasal shower, sprays or syringes; • Physiotherapy (treatment using natural and artificially created physical factors) is prescribed only when there is a good outflow of contents from the sinuses. • Taking general strengthening medications.
Surgical treatment is performed in the presence of orbital (eye) and intracranial complications. Treatment comes down to opening the purulent cavities and their sanitation, that is, removing the pus.
Complications and consequences
• Inflammation of the soft tissues of the face. • Spread of inflammation into the respiratory tract: inflammation of the bronchi (bronchitis), lungs (pneumonia), and ears (otitis). • Spread of the inflammatory process into the cranial cavity with the development of meningitis (inflammation of the meninges), encephalitis (inflammation of the brain substance) or brain abscess (formation of purulent cavities). • Purulent inflammation of the skull bones (a complication requiring surgical intervention). • Inflammation of the eyeball and its membranes, which can cause vision loss. • Inflammation of the trigeminal nerve (the large nerve in the face), accompanied by severe pain. • Sepsis is a severe complication that develops when the pathogen enters the bloodstream, with the further formation of secondary foci of inflammation in vital organs. • Risk of death.
The sooner you seek help from a specialist, the greater the chances of maintaining health and reducing the risk of complications!!!
Prevention
• Timely and adequate treatment of runny nose (rhinitis). • Treatment of nasal diseases accompanied by difficulty in nasal breathing (chronic rhinitis, deviated nasal septum). • Timely sanitation (treatment) of carious teeth. • Timely treatment of allergies. • Prevention of colds and strengthening the immune system:
hardening in the autumn-winter period; avoid hypothermia; taking multivitamin complexes in the autumn-winter period; wearing protective bandages during periods of mass morbidity, for example, influenza; balanced and rational diet (eating foods high in fiber (vegetables, fruits, herbs, etc.).
The information was prepared by an otorhinolaryngologist of the highest category, Doctor of Medical Sciences I. V. Raitselis
Sources: “Otorhinolaryngology”, manual for doctors V. T. Palchun, A. I. Kryukov, Moscow “Medicine”, 2001 “Otorhinolaryngology: national guide” edited by V. T. Palchun, GEOTAR-Media, 2008 G.
Possible complications of sinusitis
If adequate treatment of sinusitis is not carried out, then pus and inflammatory effusion from the maxillary sinuses can penetrate into the surrounding tissues. First of all, the tissues of the eye react, since in the area of the eye sockets there is a lot of loose fiber that easily absorbs liquid. Swelling and redness of the eyelids appears, and exophthalmos may even develop - protrusion of the eyeball forward. If pus destroys the wall of the maxillary sinus, there is a danger of developing osteomyelitis - inflammation of the bone tissue, in this case the upper jaw. With proper and timely treatment, the risk of such complications is low.
How to identify a cyst in the maxillary sinus?
Since cystic cavities are benign neoplasms, they do not cause any systemic manifestations. The local clinical picture manifests itself several months after the onset of the pathological process. But even its occurrence does not always become a reason to go to the doctor. Most often, maxillary sinus cysts are discovered by a dentist during a preliminary examination to perform a sinus lift or implantation.
The main clinical manifestations of cysts in the maxillary sinus:
- Painful sensations in the infraorbital region of a pressing nature (pain intensifies when changing body position);
- Discharge from the nasal passages is purulent or mucopurulent in nature, the amount of which depends on the presence and severity of the inflammatory process;
- Gradually increasing facial asymmetry (when the cyst reaches a large volume);
- Constant exacerbations of infectious lesions of the maxillary sinus;
- Swelling of the nasal passages (severe nasal congestion);
- Pain in the upper jaw (as well as: a characteristic crunch when pressed or loaded);
- Headaches (most often in the forehead or temples).
The clinical picture of cystic formations is practically indistinguishable from acute sinusitis, so doctors always differentiate these two pathologies using instrumental studies. For dental specialists, it is especially important to make the correct diagnosis, since the presence of a cyst is not always a contraindication for sinus lifting, but an acute infection does not allow surgical intervention.
Identification of cystic formations occurs by performing x-rays of the sinuses or in the process of studying the bones of the skull on a computed tomography scan. Additionally, an endoscopic examination may be prescribed, which is both diagnostic and therapeutic. Histological examination using targeted biopsy is mandatory, which allows us to have an idea of the origin of the tumor and exclude malignant oncology.
Treatment of sinusitis
The earlier treatment for sinusitis is started, the better the prognosis. If you consult a doctor before the accumulation of pus in the maxillary sinus (in the first days of the onset of symptoms of sinusitis), the treatment effect is the best (without puncture). Early use of vasoconstrictor drops and sprays will help relieve swelling of the nasal mucosa and restore the outflow of secretions from the maxillary sinuses. Antibacterial therapy and antiallergic treatment are mandatory. Local rinsing of the nose with antiseptic solutions, physical treatment - UHF, UV irradiation of the nasal cavity.
Puncture of the maxillary sinus
If sinusitis is advanced and there is thick pus in the sinuses, then a puncture is necessary. After removing the pus through a needle, the doctor rinses the maxillary sinuses with antibacterial and anti-inflammatory drugs. After the puncture, catheters are inserted into the sinus through the hole - thin tubes, which allow the sinuses to be washed every day in the future without additional punctures. Relief occurs immediately upon completion of the procedure. And recovery is going very quickly. If the doctor insists on performing a puncture, it means that it is necessary for your health.