There are many clinical conditions whose nature and distribution can be clarified by MRI.
To begin with, it is worth saying a few words about the development options, of which the most common are hypoplasia and aplasia of the sinuses.
Hypoplasia of the frontal sinus
Particularly noteworthy is such a development option as excessive pneumatization of the sphenoid sinus and posterior ethmoid cells in the form of developed upper lateral recesses, in the presence of which the internal carotid arteries and optic nerve canals can protrude into their lumen. As a result, during inflammatory processes in the mucous membranes of these sections (including subacute and chronic), a clinical picture of progressive atrophy of the optic nerves may develop. In addition, when performing surgical interventions in this anatomical area, the risk of damage to the carotid arteries and optic nerves increases many times.
Developed superolateral recesses, against which the optic nerves are identified
Inflammatory changes in the paranasal sinuses are the most common diseases of the upper respiratory tract. From 5 to 15% of the world's population suffers from various types of sinusitis. In addition, there is a trend towards an increase in chronic forms.
Facial pain with sinusitis is localized in the projection of the affected sinus. With frontal sinusitis and sinusitis, in addition to pain, there is pain on palpation. Ethmoiditis and sphenoiditis are characterized by constant pain in the eye and nose and nasal congestion. Diagnosis of chronic sinusitis is especially difficult. With mucoceles and tumors, swelling and displacement of the eyeball are observed: upward - with damage to the maxillary sinus, outward - with damage to the ethmoidal labyrinth, and downward - with damage to the frontal sinus.
Let's look at examples of pathology of the paranasal sinuses detected during an MRI examination.
Swelling of the mucous membrane of the right maxillary sinus with fluid level
MR picture of polysinusitis with a total disturbance of pneumatization of the cells of the ethmoid bone, moderate, sometimes uneven, local disturbance of pneumatization of the right half of the main sinus and the upper parts of the left maxillary sinus, without an exudative component.
What does a sinus x-ray show?
An x-ray shows the human skull with bone structures, cavities and septa. The method is used at the preparatory stage in surgery.
What can be seen on a sinus x-ray:
- Foreign object in the nasal passages.
- Inflammatory process, thickening of the mucous membrane of the infected area.
- Consequences of injuries to the face and head.
- The presence of exudate (mucous, blood, purulent) in the paranasal and frontal cavities.
- "Airiness" of the sinuses.
- Neoplasms: polyps, tumors, cysts.
- Anomalies in the structure of the facial skeleton.
X-rays help to correct the diagnosis in case of fever or headache of unknown etiology.
The most common (58-90%) is squamous cell carcinoma.
1. are asymptomatic for a long time, under the guise of inflammatory changes, especially in the absence of destruction of the walls 2. quickly spread to neighboring structures and by the time of recognition, infiltrate several areas 3. it is difficult or impossible to establish the original site of tumor origin 4. extremely rarely metastasizes to distant organs and tissue 5. it is not possible to clearly define the boundaries of the lesion 6. MR semiotics: tissue formation, spread to surrounding tissues, bone destruction
If bone structures are damaged - the hard palate and the alveolar process of the upper jaw, it is necessary to undergo an additional radiological examination - X-ray CT, which clarifies the presence or absence of bone destruction.
Detection of tumor tissue against the background of soft tissue structures - the pterygopalatine and infratemporal fossa, masticatory muscles, soft tissues of the cheek, as well as the spread of the tumor to the frontal and sphenoid sinuses, the ethmoidal labyrinth intracranially requires MRI (with contrast enhancement). In addition, MR imaging is indispensable in the differential diagnosis of postoperative or post-radiation changes with relapse or continued growth.
Thus, in order to exclude a pathological process and begin treatment on time, it is necessary to undergo a complete radiation examination.
How is a sinus x-ray performed?
The procedure is not painful and does not require preparation. Receive a referral at an appointment with an otolaryngologist, infectious disease specialist or surgeon.
How to do a sinus x-ray:
- The patient removes metal jewelry, glasses, and dentures.
- To protect against radiation, he wears a lead apron or vest with a collar.
- The laboratory assistant indicates how to position yourself correctly relative to the apparatus. Depending on the required projections, the position is changed at the command of a specialist.
- While taking the photo, you should not move and hold your breath.
- After development and decoding, the film with the description is given to the patient.
The conclusion is not considered a final diagnosis, but provides clarifying information for the treating specialist.
conclusions
1. High-tech methods of radiological diagnostics (MSCT or CBCT) are a necessary component of the complex diagnosis of HFRS.
2. The use of computed tomography (MSCT or CBCT) makes it possible to determine the cause of AHF and, thus, choose the correct tactics for patient management.
3. MSCT or CBCT should be recommended to patients before and after endodontic treatment of teeth and dental implantation, as well as during surgical interventions on the upper jaw in order to timely identify possible pathological changes in the maxillary sinuses (including asymptomatic ones).
Conflict of interest: The authors of the article have confirmed that they have no financial support/conflict of interest to report.
Darkening of the sinuses on x-ray
The method is based on the different permeability of hard and soft tissues by electromagnetic waves. Bones block radiation and appear white in the picture. Specialists are interested in blackouts, which determine the nature of the disorder.
Darkening of the sinuses on an x-ray indicates fluid accumulation. This is a sign of inflammation with the release of mucous or purulent secretion. Sometimes, the picture shows thickening of the walls of the mucous membrane lining the sinuses.
New growths stand out as clear dark spots with shadows. Polyps look like peas on a “pedicle”, and cysts have a cavity filled with fluid inside.
Chronic rhinosinusitis
characterized by parietal thickenings caused by hyperplasia of the mucosa and partial fibrous changes in it. The thickness of the mucous membrane ranges from 4-5 mm.
Sinonasal polyposis, hypertrophic sinonasal rhinosinusitis. Non-tumor inflammatory swelling of the mucous membrane.
Recently, there has been an increase in the number of fungal sinusitis. Chronic forms occur under the guise of polypous recurrent sinusitis, the MRI picture is nonspecific, and laboratory diagnosis is difficult. There may be a change in the bony walls of the sinuses due to hyperostosis or destruction of the sinus wall as a result of prolonged pressure from the fungal body.
X-ray of the sinuses during pregnancy
The radiation dose during the study is 20 μSv and is considered safe even when performed repeatedly for an adult. The fetus is susceptible to ionizing radiation, which causes intrauterine developmental defects. Carrying a child is a contraindication to the procedure.
X-rays of the nasal sinuses during pregnancy and breastfeeding are done exclusively for health reasons. The potential benefit of the research must outweigh the harm to the child. After the procedure, a pregnant woman needs an ultrasound of the fetus, and a nursing woman needs to transfer the baby to artificial nutrition for a day.
Results and discussion
Analysis of the results of radiological diagnostic methods revealed signs of RFS in 110 (66.2%) of 166 cases. 66 (39.7%) patients had characteristic clinical symptoms of the disease (headache, low-grade fever, sleep disturbance, a feeling of heaviness in the corresponding half of the face when tilting the head anteriorly, nasal congestion on one side only); these patients were referred for radiation examination by otorhinolaryngologists. The remaining 44 (26.5%) people did not have complaints from the maxillary sinuses; Previously, they were sent for examination by dentists and maxillofacial surgeons for the following reasons: 22 (13.2%) patients - to clarify their dental status, 12 (7.3%) patients - before dental implantation, 10 (6%) patients - for postoperative control after surgical interventions on the upper jaw. In these cases, the identified inflammation of the maxillary sinus was a diagnostic finding.
As is known, acute odontogenic inflammation of the maxillary sinus develops within 1-3 days. Quite often the cause is an inflammatory process of the upper jaw (acute or exacerbation of a chronic one). Such conditions include complications of dental caries, periodontitis, periostitis, osteomyelitis, as well as suppuration of dental cysts or granulomas [7, 8].
Typical complaints of patients with acute maxillary sinusitis were: difficulty in nasal breathing, rhinorrhea, loss of smell, headache and facial pain, a feeling of heaviness in the corresponding half of the face when tilting the head forward, low-grade fever, as well as night cough and sleep disturbances. Odontogenic sinusitis, in contrast to rhinogenic sinusitis, has the following distinctive features: isolated damage to one of the maxillary sinuses, pain in the tooth or in periodontal tissues that precedes the disease, disruption of the facial configuration as a result of swelling of the soft tissues of the cheek and pain on palpation of the anterolateral wall of the maxillary sinus.
In acute sinusitis, x-rays showed thickened mucous membranes, darkening, and fluid levels. In chronic sinusitis, a decrease in sinus transparency was noted.
When assessing and analyzing diagnostic images, the criteria for odontogenic sinusitis were the following: the presence of a foreign body of metallic density corresponding to a filling material or implant in the sinus cavity; deep caries and signs of periodontitis of premolars and molars of the upper jaw; destruction of the lower bone wall of the maxillary sinuses in the area of pathologically changed teeth, as well as partial adentia of the upper jaw in the area corresponding to changes in the maxillary sinus.
During an X-ray examination, in 44 (26.5%) patients with acute maxillary sinusitis, a thickened mucous membrane and/or subtotal darkening with a horizontal fluid level was detected on a plain radiograph. In 78 (47%) patients, there was a total decrease in sinus transparency, of which 38 (22.8%) patients had foreign bodies of metal density (corresponding to filling material) found in the sinus cavity. However, the low contrast of liquid and soft tissues and the summation of shadows made it difficult to objectively assess the obtained radiographs. For additional assessment of the condition of the teeth of the upper jaw, all patients underwent orthopantomography, which did not allow reliably assessing the condition of the maxillary sinuses, and in 13 (7.8%) patients, accurately interpreting changes in the area of the apexes of the teeth of the upper jaw (due to the reflection of the projection layering of complex anatomical structures ).
According to the results of our study, 24 (14.5%) patients showed signs of chronic periodontitis in the area of premolars and molars of the upper jaw (Fig. 1). Deep caries was diagnosed in 4 (2.4%) patients, maxillary cysts in the area of the roots of premolars and molars were visualized in 6 (3.6%) cases.
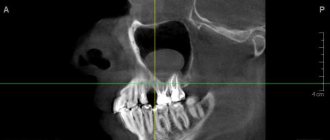
Rice. 1. CBCT. Panoramic (a) and multiplanar reconstructions of the right (b) and left (c) maxillary sinuses of patient M., 37 years old. Diagnosis: bilateral odontogenic chronic maxillary sinusitis. CT signs of chronic granulomatous periodontitis of teeth 1.8, 2.7, 2.8 are noted (in the form of foci of destruction at the apices of the roots, round in shape, with clear, even contours). The lower bone walls of the sinuses are thinned and cannot be traced in the periodontal area of teeth 1.8 and 2.8 (indicated by arrows). In the lower part of the right maxillary sinus, a parietal soft tissue formation of a homogeneous structure with a polycyclic upper contour is determined. The left maxillary sinus is subtotally filled with soft tissue contents of a homogeneous structure with a rounded upper contour.
Filling material was found in 38 (22.8%) patients (Fig. 2). Of these, in 34 (20.4%) patients in the submucosal layer of the lower wall of the sinus, in 4 (2.4%) - in the upper section near the medial wall of the sinus (Fig. 3). 8 (4.8%) patients were diagnosed with dental implantation errors: the tip of the implant was immersed in the sinus cavity, which caused the development of chronic odontogenic maxillary sinusitis, as well as complications in the form of chronic polysinusitis ( n
=4; 2,4%).
Rice. 2. MSCT. Coronal (a) and sagittal (b) reconstruction of the right maxillary sinus of patient K., 29 years old. Diagnosis: right-sided odontogenic chronic maxillary sinusitis. The roots of teeth 1.6, 1.7 and 1.8 are immersed in the cavity of the maxillary sinus. Condition after endodontic treatment of teeth 1.6 and 1.7, with removal of the filling material beyond the apex of the palatal root 1.7. In the area of the roots of teeth 1.6 and 1.7, there is a rarefaction of bone tissue with fuzzy, uneven contours (radiological signs of granulating periodontitis). In the lower part of the sinus, a parietal soft tissue formation with a polycyclic contour is determined; the bony walls of the sinus are not traced in this area.
Rice.
3. CBCT. Sagittal reconstruction, right maxillary sinus. Patient U., 48 years old. Diagnosis: right-sided odontogenic chronic maxillary sinusitis. Teeth 1.6 and 1.7 after endodontic treatment, the filling material is removed from the apex of the roots of tooth 1.6 (the material is located in the bone tissue of the alveolar process and in the submucosal layer of the sinus). A loss of bone tissue is determined in the area of roots 1.6 and 1.7; the bone wall of the sinus is not visible in this area (arrow). In the lower part of the sinus, thickening of the mucous membrane up to 10 mm is determined, in the superomedial part of the sinus an irregularly shaped foreign body of metal density is visualized (corresponding to fragments of filling material). In our study, 30 (18.1%) patients had absence of maxillary teeth in the area corresponding to changes in the maxillary sinus, which also made it possible to judge the odontogenicity of maxillary sinusitis.
In all cases, computed tomography (MSCT or CBCT) made it possible to accurately diagnose the form of the disease, determine the extent of damage to the sinuses, assess the condition of the lower bone wall of the sinus (identify a violation of its integrity and the communication of the tooth socket with the sinus), determine the source of inflammation in the periodontium, and also identify the presence of foreign bodies in the maxillary sinus. At the same time, the data from MSCT and CBCT were completely comparable with each other, significantly superior to traditional X-ray techniques in terms of diagnostic information content and had such advantages as the absence of superposition, high contrast resolution and the ability to obtain higher-quality reconstructions of images in various planes and 3D images of the area of interest, and also a significant reduction in patient examination time and a reduction in radiation exposure. After computed tomography, treatment tactics were adjusted in 38 (22.9%) patients.
X-ray of the sinuses for children
Pediatricians try to protect preschool children from the harm caused by X-ray radiation to the fragile skeletal system. The procedure is allowed to be performed on patients over 7 years of age.
Before this period, a clear justification for the importance of intervention is necessary - for example, severe facial trauma or severe sinusitis with a risk of inflammation of the meninges.
It is difficult for a young child to sit or stand still during an x-ray. To distract him, they use toys, sedatives, and in emergency cases, anesthesia. At an older age, you can captivate your child with a game in which you should freeze for a short time.
Sign up for the study
Patients and methods
In the period from 2013 to 2015 in the Department of Radiation Diagnostics of Clinical Hospital No. 1 of the First Moscow State Medical University named after. THEM. Sechenov examined 166 patients with maxillary sinusitis of various etiologies. In 110 patients (66.2%) the odontogenic etiology of the disease was confirmed. An analysis of the distribution of patients according to age and gender showed that of the examined patients with TFS, the majority - 91 (54.8%) people - were young and mature, from 21 to 60 years of age. There were 19 (11.4%) patients over 60 years of age; the average age of patients was 48 years (from 21 to 81 years). The majority were female (62 (37.3%) women and 48 (28.9%) men) of working age.
A comparison of the clinical manifestations of odontogenic HFS and the X-ray picture made it possible to conditionally group patients into two groups: 66 (39.7%) patients with an acute inflammatory process in the maxillary sinus had corresponding clinical symptoms of the disease, and 44 (26.5%) patients had complaints from the maxillary sinus no sinuses were presented (the inflammatory process in the maxillary sinus was chronic).
A comprehensive X-ray examination was performed in all cases. All patients underwent computed tomography (MSCT or CBCT): MSCT - 76 (45.8%) patients, CBCT - 90 (54.2%) patients. 122 (73.5%) patients underwent radiography of the paranasal sinuses in the nasomental, semi-axial projections. To clarify the condition of the teeth of the upper jaw, orthopantomography was performed ( n
=166, 100%) and intraoral contact radiography (
n
=12, 7.3%).
When assessing and analyzing diagnostic images, the criteria for odontogenic sinusitis were the following: the presence of a foreign body of metallic density corresponding to a filling material or implant in the sinus cavity; deep caries and signs of periodontitis of premolars and molars of the upper jaw; destruction of the lower bone wall of the maxillary sinuses in the area of pathologically changed teeth.
Treatment of advanced sinusitis
After developing radiographs, one can judge the severity of the inflammatory process occurring in the maxillary sinuses. In case of total blackout, the doctor may prescribe a shock course of antibiotics and antihistamines to suppress inflammatory processes and reduce the severity of some symptoms.
In the most severe cases, surgical intervention may be indicated - puncture of the sinuses. This procedure has been known for a long time and is widely used in many countries around the world. Using a special syringe, excess fluid and pus are pumped out of the maxillary sinus. Then the sinus is filled with a special solution containing antiseptic drugs. This is done to reduce inflammation of the mucous membrane. Then the solution is pumped out of the sinuses. That's it, the procedure is completed.
This type of surgery is not dangerous, but it can speed up recovery and reduce the appearance of major symptoms, such as headaches.
For more effective treatment of sinusitis, the pus obtained after puncture can be sent for culture to identify the pathogen and determine which antibacterial drugs it is most sensitive to. Along with antibiotics, antihistamines are often prescribed to help reduce swelling, nasal congestion and other manifestations of the disease.
Some traditional medicines can be used to treat sinusitis. Such remedies should not replace the primary treatment prescribed by a doctor. They can only complement it. Moreover, before using any means, you should consult your doctor.
Using exclusively traditional medicine to treat sinusitis can lead to disastrous results. Untreated sinusitis will become chronic and will periodically trouble the patient throughout his life.
Decoding the testimony
The radiologist deciphers what an x-ray of the paranasal sinuses shows. First of all, the condition and location of bone structures and cartilage is assessed. The liquid on the x-ray image appears as an intensely darkened horizontal boundary. Thickening of the mucous membrane indicates swelling in the paranasal sinus. You will receive a transcript of the research results in the form of a conclusion, but the final diagnosis is made by the doctor. Usually, when a pathology is identified that requires a more detailed study, another diagnostic method is prescribed.
Location and functions of the maxillary sinuses
The maxillary sinus is also called the maxillary sinus. It is a paired paranasal sinus of the nasal cavity. It is located almost throughout the entire space of the maxillary bone, inside the upper jaw. The sinuses consist of the nasal, facial and orbital, posterior and inferior walls.
The maxillary sinuses are lined from the inside with a mucous membrane, which is represented by ciliated epithelium.
There are few nerves and blood vessels in this area. Therefore, inflammatory diseases of the paranasal sinuses remain undiagnosed for a long time, as they occur without severe pain. Pain usually appears during the height of the disease.
Functions of the maxillary sinuses:
- Humidification of inhaled air.
- Participation in the formation of voice.
- Regulation of intracranial pressure.
- Lightening the weight of the skull bones.
- Air filtration and protection against pathogenic microorganisms.
Why, when symptoms of acute purulent sinusitis appear, you should urgently consult an ENT doctor:
Do not forget that “the nose grows on the head,” which means that any purulent diseases of the paranasal sinuses mean the presence of pus in the skull, in close proximity to the cavity of the orbits and to the brain, therefore complications can be extremely serious, with the most unpredictable consequences:
- Otitis
- Intraorbital complications (orbital cellulitis, orbital abscess)
- Intracranial complications (meningitis, encephalitis, brain abscess)
There is no need to try to cope with sinusitis on your own. The presence of a purulent process in the sinus indicates that it cannot empty itself and if time is lost, there is a high probability that the pus will make its way into one of the nearby organs.